Tuesday Poster Session
Category: Liver
P6111 - Unexpected Decompensated Cirrhosis and Ascitic Peritonitis Following Elective Hysterectomy: A Case of Missed Preoperative Liver Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ishan Antony, MD
Beth Israel Lahey Health
Burlington, MA
Presenting Author(s)
Ishan Antony, MD1, Ali Shaat, MD2, Ming V.. Lin, MD2
1Beth Israel Lahey Health, Burlington, MA; 2Lahey Hospital and Medical Center, Burlington, MA
Introduction: In patients without known liver disease, intraoperative discovery of ascites may be the first sign of advanced cirrhosis. This case highlights how elective pelvic surgery triggered a cascade of complications in a patient with unrecognized decompensated alcohol-related liver disease.
Case Description/
Methods: A 53-year-old woman with a history of alcohol use disorder underwent elective vaginal hysterectomy with salpingectomy for symptomatic uterovaginal prolapse. Intraoperatively, 750 mL of ascitic fluid was removed, and the liver appeared cirrhotic. She denied prior knowledge of liver disease, and she did not recall any preoperative abdominal imaging. Few days later, she developed hemorrhagic shock requiring emergent exploratory laparotomy, which revealed 2 L of pelvic clot and recurrent ascites.
Her postoperative course was complicated by worsening ascites, acute kidney injury concerning for hepatorenal syndrome, and neutrocytic ascitic fluid (ANC 800), prompting treatment for presumed secondary bacterial peritonitis including IV antibiotics, serial paracenteses, and abdominal drain placements. Despite broad-spectrum antibiotics, she deteriorated clinically. Repeat imaging revealed extravasation of enteric contrast, and she underwent open laparotomy which showed a missed iatrogenic small bowel perforation near a prior pelvic drain, confirming the source of her secondary bacterial peritonitis. A J-tube was placed for nutritional support. Her case was further complicated by hepatic encephalopathy and persistent ascitic fluid collections. The patient eventually underwent inpatient liver transplant evaluation following treatment with long-term antibiotics, nutritional optimization, and aggressive supportive care. She had a successful orthotopic liver transplantation 158 days after her initial presentation.
Discussion: This case illustrates how unrecognized cirrhosis may first present as intraoperative ascites during unrelated elective surgery and should prompt urgent hepatology evaluation and surgical reconsideration. The patient’s eventual stabilization and successful transplantation highlight the value of multidisciplinary rescue even when the initial opportunity is missed. This case underscores the need for preoperative liver disease screening in high-risk patients, particularly those with heavy alcohol use, to avoid preventable morbidity and mortality.
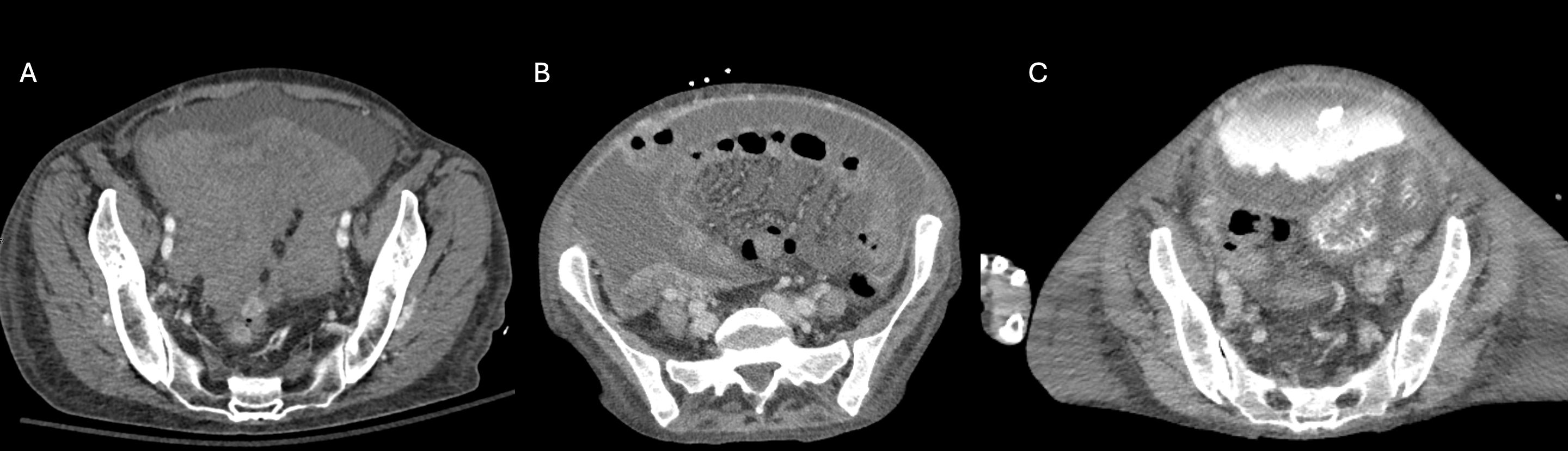
Figure: Figure 1: Sequential abdominal imaging: (A) Initial postoperative CT imaging following vaginal hysterectomy demonstrating large pelvic hematoma (12.5 × 15 × 11.5 cm) with moderate ascites. (B) Follow-up CT abdomen/pelvis showing new peritoneal enhancement and thickening, concerning for evolving peritonitis. (C) Contrast-enhanced CT demonstrating extravasation of enteric contrast into the peritoneal cavity, confirming bowel perforation.
Disclosures:
Ishan Antony indicated no relevant financial relationships.
Ali Shaat indicated no relevant financial relationships.
Ming Lin indicated no relevant financial relationships.
Ishan Antony, MD1, Ali Shaat, MD2, Ming V.. Lin, MD2. P6111 - Unexpected Decompensated Cirrhosis and Ascitic Peritonitis Following Elective Hysterectomy: A Case of Missed Preoperative Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Beth Israel Lahey Health, Burlington, MA; 2Lahey Hospital and Medical Center, Burlington, MA
Introduction: In patients without known liver disease, intraoperative discovery of ascites may be the first sign of advanced cirrhosis. This case highlights how elective pelvic surgery triggered a cascade of complications in a patient with unrecognized decompensated alcohol-related liver disease.
Case Description/
Methods: A 53-year-old woman with a history of alcohol use disorder underwent elective vaginal hysterectomy with salpingectomy for symptomatic uterovaginal prolapse. Intraoperatively, 750 mL of ascitic fluid was removed, and the liver appeared cirrhotic. She denied prior knowledge of liver disease, and she did not recall any preoperative abdominal imaging. Few days later, she developed hemorrhagic shock requiring emergent exploratory laparotomy, which revealed 2 L of pelvic clot and recurrent ascites.
Her postoperative course was complicated by worsening ascites, acute kidney injury concerning for hepatorenal syndrome, and neutrocytic ascitic fluid (ANC 800), prompting treatment for presumed secondary bacterial peritonitis including IV antibiotics, serial paracenteses, and abdominal drain placements. Despite broad-spectrum antibiotics, she deteriorated clinically. Repeat imaging revealed extravasation of enteric contrast, and she underwent open laparotomy which showed a missed iatrogenic small bowel perforation near a prior pelvic drain, confirming the source of her secondary bacterial peritonitis. A J-tube was placed for nutritional support. Her case was further complicated by hepatic encephalopathy and persistent ascitic fluid collections. The patient eventually underwent inpatient liver transplant evaluation following treatment with long-term antibiotics, nutritional optimization, and aggressive supportive care. She had a successful orthotopic liver transplantation 158 days after her initial presentation.
Discussion: This case illustrates how unrecognized cirrhosis may first present as intraoperative ascites during unrelated elective surgery and should prompt urgent hepatology evaluation and surgical reconsideration. The patient’s eventual stabilization and successful transplantation highlight the value of multidisciplinary rescue even when the initial opportunity is missed. This case underscores the need for preoperative liver disease screening in high-risk patients, particularly those with heavy alcohol use, to avoid preventable morbidity and mortality.
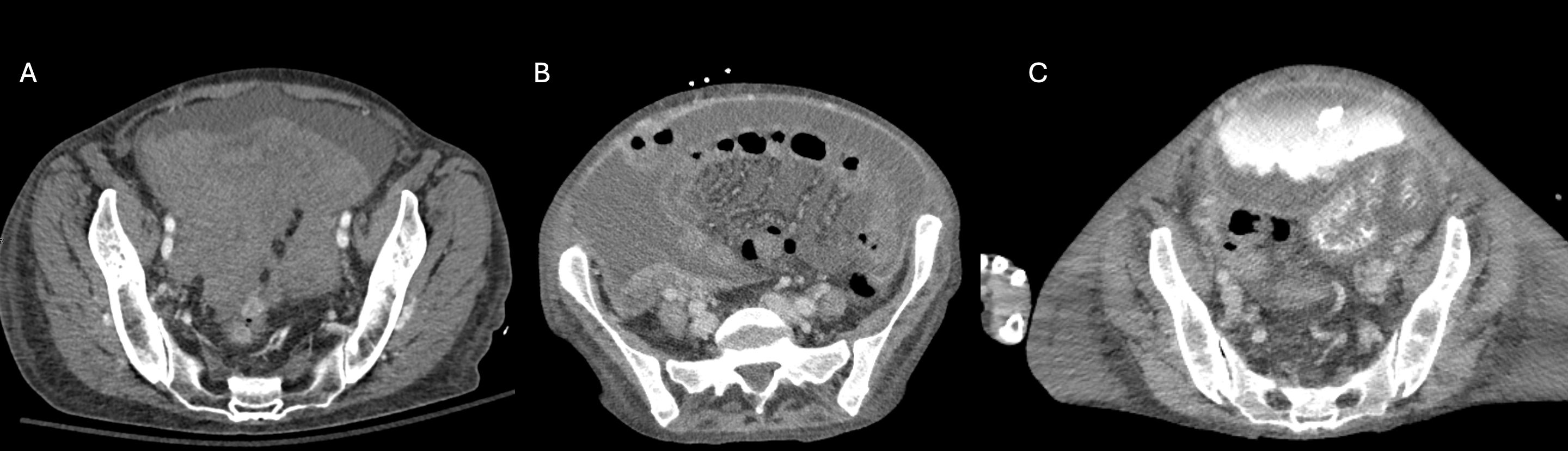
Figure: Figure 1: Sequential abdominal imaging: (A) Initial postoperative CT imaging following vaginal hysterectomy demonstrating large pelvic hematoma (12.5 × 15 × 11.5 cm) with moderate ascites. (B) Follow-up CT abdomen/pelvis showing new peritoneal enhancement and thickening, concerning for evolving peritonitis. (C) Contrast-enhanced CT demonstrating extravasation of enteric contrast into the peritoneal cavity, confirming bowel perforation.
Disclosures:
Ishan Antony indicated no relevant financial relationships.
Ali Shaat indicated no relevant financial relationships.
Ming Lin indicated no relevant financial relationships.
Ishan Antony, MD1, Ali Shaat, MD2, Ming V.. Lin, MD2. P6111 - Unexpected Decompensated Cirrhosis and Ascitic Peritonitis Following Elective Hysterectomy: A Case of Missed Preoperative Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
