Tuesday Poster Session
Category: Liver
P6106 - Hepatic Sinusoidal Obstruction Syndrome Induced by FOLFOX Chemotherapy in a Lynch Syndrome Patient With Rectal Cancer Presenting With Anemia
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ricky Rana, MD (he/him/his)
Creighton University School of Medicine
Sugar Land, TX
Presenting Author(s)
Marcellus A. Singh, MD1, Ricky Rana, MD2, Kathryn Henderson, DO1, Clive J. Miranda, DO, MSc1
1CHI Health Creighton University Medical Center, Omaha, NE; 2Creighton University School of Medicine, Omaha, NE
Introduction: Hepatic Sinusoidal Obstruction Syndrome (HSOS) is a rare condition where sinusoidal endothelial cell damage causes obstruction of veins in the liver leading to congestion, cell damage, and liver dysfunction. HSOS is commonly seen as a complication of chemotherapy, particularly with agents like oxaliplatin (OXA). The pathogenesis of OXA-induced HSOS is likely due to oxidative stress, inflammation, and fibrosis. We present a case of HSOS in a patient with stage III rectal cancer with underlying Lynch syndrome highlighting diagnostic challenges and implications for surveillance.
Case Description/
Methods: A 25-year-old female with stage III rectal adenocarcinoma who completed neoadjuvant chemoradiation with 6 cycles of 5-fluorouracil prior to 12 rounds of folinic acid, fluorouracil, and oxaliplatin. Biopsy with genetic testing later showed MLH1 and PMS2 gene mutations, confirming Lynch syndrome. She subsequently underwent colectomy with low colorectal anastomoses along with prophylactic hysterectomy, salpingo-oophorectomy and posterior vaginal wall removal. Patient later presented with anemia with hemoglobin level of 4.9. Subsequent esophagogastroduodenoscopy demonstrated bleeding esophageal varices. Liver biopsy was done due to suspected cirrhosis and showed sinusoidal dilation and periportal hepatocyte necrosis, suggestive of sinusoidal obstructive syndrome. Although no evidence of shrunken central veins or congested sinusoids, which would provide stronger evidence of OXA-induced HSOS, patient continues to undergo surveillance for her esophageal varices with repeated need for banding secondary to portal hypertension in the setting of HSOS.
Discussion: Patients with HSOS often present with symptoms of liver failure such as jaundice, hepatomegaly, and ascites. Diagnosis is made using clinical criteria such as the modified Seattle criteria. Treatment involves cessation of the causative drug and treatment of complications related to portal hypertension. This case highlights a serious adverse drug reaction (ADR) associated with OXA. OXA-induced HSOS is a potentially fatal complication of chemotherapy in obstruction of venous outflow, hepatic congestion, and liver dysfunction. Early recognition is crucial for management. Gastroenterologists must be cognizant of this ADR as timely intervention is critical to preventing irreversible hepatic damage and avoid complications related to portal hypertension that may require long-term surveillance.
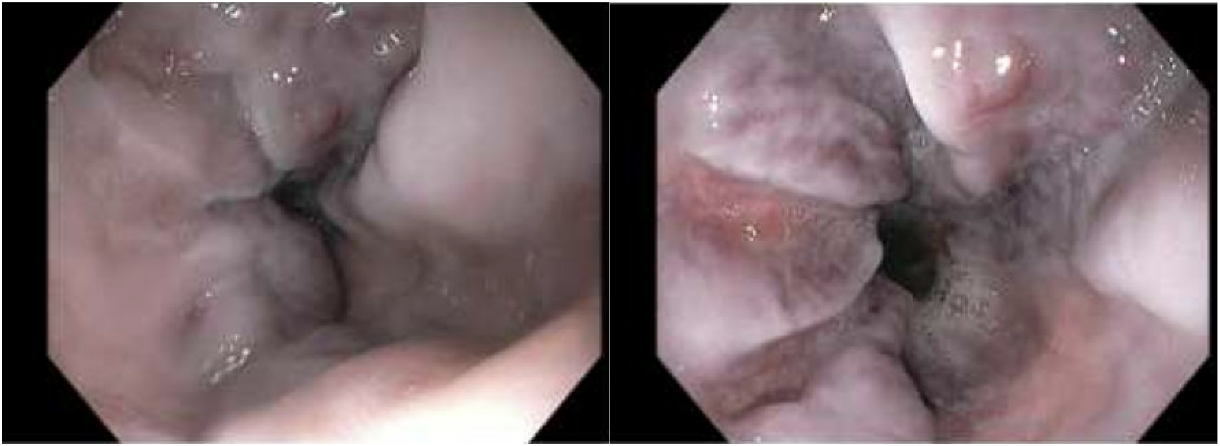
Figure: Figure 1: EGD image showing four columns of Grade 2, large ( > 5mm) varices in lower third of esophagus with Red wale signs present.

Figure: Figure 2: A) Low-power view of liver needle core biopsy (H&E, 4x). B) Liver parenchyma with mild sinusoidal dilatation (arrow) on a background of mildly reactive hepatocytes (H&E, 20x). C) Reticulin stain highlighting foci of hepatocyte loss (collapse), 20x.
Disclosures:
Marcellus Singh indicated no relevant financial relationships.
Ricky Rana indicated no relevant financial relationships.
Kathryn Henderson indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Marcellus A. Singh, MD1, Ricky Rana, MD2, Kathryn Henderson, DO1, Clive J. Miranda, DO, MSc1. P6106 - Hepatic Sinusoidal Obstruction Syndrome Induced by FOLFOX Chemotherapy in a Lynch Syndrome Patient With Rectal Cancer Presenting With Anemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1CHI Health Creighton University Medical Center, Omaha, NE; 2Creighton University School of Medicine, Omaha, NE
Introduction: Hepatic Sinusoidal Obstruction Syndrome (HSOS) is a rare condition where sinusoidal endothelial cell damage causes obstruction of veins in the liver leading to congestion, cell damage, and liver dysfunction. HSOS is commonly seen as a complication of chemotherapy, particularly with agents like oxaliplatin (OXA). The pathogenesis of OXA-induced HSOS is likely due to oxidative stress, inflammation, and fibrosis. We present a case of HSOS in a patient with stage III rectal cancer with underlying Lynch syndrome highlighting diagnostic challenges and implications for surveillance.
Case Description/
Methods: A 25-year-old female with stage III rectal adenocarcinoma who completed neoadjuvant chemoradiation with 6 cycles of 5-fluorouracil prior to 12 rounds of folinic acid, fluorouracil, and oxaliplatin. Biopsy with genetic testing later showed MLH1 and PMS2 gene mutations, confirming Lynch syndrome. She subsequently underwent colectomy with low colorectal anastomoses along with prophylactic hysterectomy, salpingo-oophorectomy and posterior vaginal wall removal. Patient later presented with anemia with hemoglobin level of 4.9. Subsequent esophagogastroduodenoscopy demonstrated bleeding esophageal varices. Liver biopsy was done due to suspected cirrhosis and showed sinusoidal dilation and periportal hepatocyte necrosis, suggestive of sinusoidal obstructive syndrome. Although no evidence of shrunken central veins or congested sinusoids, which would provide stronger evidence of OXA-induced HSOS, patient continues to undergo surveillance for her esophageal varices with repeated need for banding secondary to portal hypertension in the setting of HSOS.
Discussion: Patients with HSOS often present with symptoms of liver failure such as jaundice, hepatomegaly, and ascites. Diagnosis is made using clinical criteria such as the modified Seattle criteria. Treatment involves cessation of the causative drug and treatment of complications related to portal hypertension. This case highlights a serious adverse drug reaction (ADR) associated with OXA. OXA-induced HSOS is a potentially fatal complication of chemotherapy in obstruction of venous outflow, hepatic congestion, and liver dysfunction. Early recognition is crucial for management. Gastroenterologists must be cognizant of this ADR as timely intervention is critical to preventing irreversible hepatic damage and avoid complications related to portal hypertension that may require long-term surveillance.
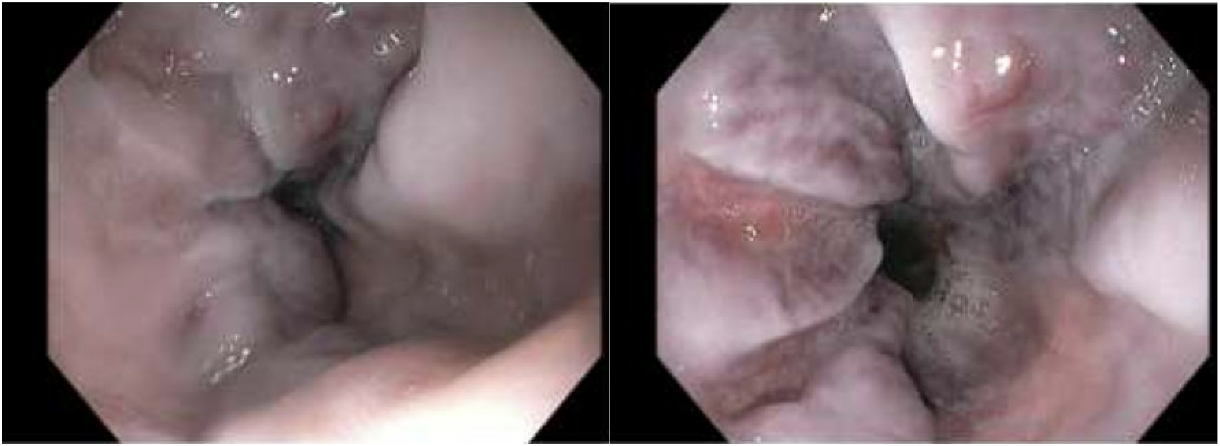
Figure: Figure 1: EGD image showing four columns of Grade 2, large ( > 5mm) varices in lower third of esophagus with Red wale signs present.

Figure: Figure 2: A) Low-power view of liver needle core biopsy (H&E, 4x). B) Liver parenchyma with mild sinusoidal dilatation (arrow) on a background of mildly reactive hepatocytes (H&E, 20x). C) Reticulin stain highlighting foci of hepatocyte loss (collapse), 20x.
Disclosures:
Marcellus Singh indicated no relevant financial relationships.
Ricky Rana indicated no relevant financial relationships.
Kathryn Henderson indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Marcellus A. Singh, MD1, Ricky Rana, MD2, Kathryn Henderson, DO1, Clive J. Miranda, DO, MSc1. P6106 - Hepatic Sinusoidal Obstruction Syndrome Induced by FOLFOX Chemotherapy in a Lynch Syndrome Patient With Rectal Cancer Presenting With Anemia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
