Tuesday Poster Session
Category: Liver
P6104 - Double Whammy: A Rare Case of Hepatitis a and EBV-Induced Acute Hepatitis in an Immunocompetent Patient
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

David Okuampa, MD
Louisiana State University Health
Shreveport, LA
Presenting Author(s)
David Okuampa, MD1, Michael Tran, MD2, Sarav Daid, MD2
1Louisiana State University Health, Shreveport, LA; 2LSU Health Shreveport, Shreveport, LA
Introduction: Hepatitis A virus (HAV) and Epstein-Barr virus (EBV) are established causes of acute hepatitis, though their routes of transmission and clinical manifestations differ. While HAV typically causes self-limited hepatocellular injury, EBV-related hepatitis is usually mild and subclinical in immunocompetent individuals. Co-infection with both viruses is exceedingly rare, with few cases reported. We present a unique case of concurrent acute HAV and primary EBV infection in a healthy adult, resulting in significant cholestatic hepatitis with histologic evidence of EBV-associated hepatic injury.
Case Description/
Methods: A 28-year-old healthy male presented with four days of progressive nausea, vomiting, epigastric pain, fever, dyspnea, and a single episode of hematemesis. Laboratory evaluation revealed leukocytosis, elevated AST (476 U/L), ALT (423 U/L), ALP (854 U/L), and total bilirubin (4.1 mg/dL), with an R-factor of 1.5, indicating a cholestatic pattern of liver injury.
Workup revealed positive HAV IgM and EBV serologies (positive VCA (viral capsid antigen) IgM, EA (early antigen) IgG, and heterophile antibodies) consistent with acute infection. Physical exam noted occipital and inguinal lymphadenopathy. Imaging demonstrated hepatosplenomegaly and periportal edema without biliary obstruction. Despite supportive care, ALP peaked at 1131 U/L. Endoscopic ultrasound with liver biopsy revealed portal and sinusoidal lymphocyte-predominant inflammation, consistent with EBV-associated hepatitis. The patient was started on ursodiol and experienced resolution of symptoms with gradual improvement in liver enzymes.
Discussion: This case highlights a rare co-infection of HAV and EBV leading to clinically significant cholestatic hepatitis in an immunocompetent adult. The unusual presentation underscores the importance of always including both hepatotropic and non-hepatotropic viruses in the diagnostic workup of acute hepatitis, especially when liver injury patterns are atypical or accompanied by systemic symptoms such as lymphadenopathy or night sweats. Comprehensive serologic evaluation is critical for accurate diagnosis and optimal management. Early recognition of co-infection can guide appropriate supportive management and avoid unnecessary interventions.
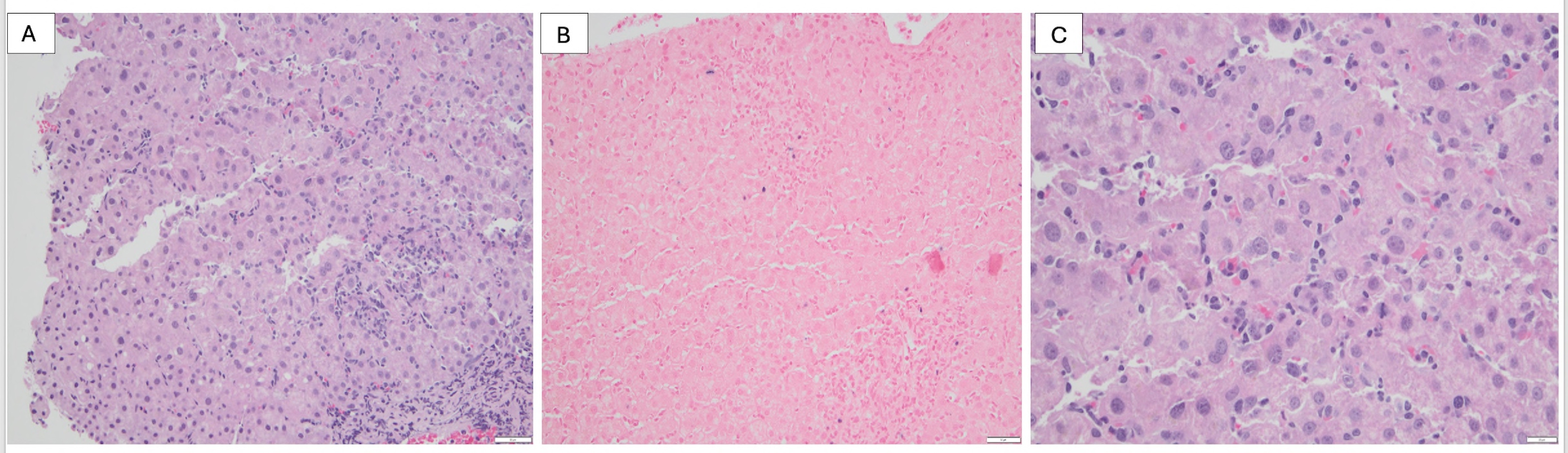
Figure:
Histological images from liver biopsy
Figure 1A-B. H&E stain of EBV Hepatitis showing sinusoidal and lobular inflammation -
Figure 1C - Histological results showing EBER positive (blue color) in liver biopsy result.
Disclosures:
David Okuampa indicated no relevant financial relationships.
Michael Tran indicated no relevant financial relationships.
Sarav Daid indicated no relevant financial relationships.
David Okuampa, MD1, Michael Tran, MD2, Sarav Daid, MD2. P6104 - Double Whammy: A Rare Case of Hepatitis a and EBV-Induced Acute Hepatitis in an Immunocompetent Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Louisiana State University Health, Shreveport, LA; 2LSU Health Shreveport, Shreveport, LA
Introduction: Hepatitis A virus (HAV) and Epstein-Barr virus (EBV) are established causes of acute hepatitis, though their routes of transmission and clinical manifestations differ. While HAV typically causes self-limited hepatocellular injury, EBV-related hepatitis is usually mild and subclinical in immunocompetent individuals. Co-infection with both viruses is exceedingly rare, with few cases reported. We present a unique case of concurrent acute HAV and primary EBV infection in a healthy adult, resulting in significant cholestatic hepatitis with histologic evidence of EBV-associated hepatic injury.
Case Description/
Methods: A 28-year-old healthy male presented with four days of progressive nausea, vomiting, epigastric pain, fever, dyspnea, and a single episode of hematemesis. Laboratory evaluation revealed leukocytosis, elevated AST (476 U/L), ALT (423 U/L), ALP (854 U/L), and total bilirubin (4.1 mg/dL), with an R-factor of 1.5, indicating a cholestatic pattern of liver injury.
Workup revealed positive HAV IgM and EBV serologies (positive VCA (viral capsid antigen) IgM, EA (early antigen) IgG, and heterophile antibodies) consistent with acute infection. Physical exam noted occipital and inguinal lymphadenopathy. Imaging demonstrated hepatosplenomegaly and periportal edema without biliary obstruction. Despite supportive care, ALP peaked at 1131 U/L. Endoscopic ultrasound with liver biopsy revealed portal and sinusoidal lymphocyte-predominant inflammation, consistent with EBV-associated hepatitis. The patient was started on ursodiol and experienced resolution of symptoms with gradual improvement in liver enzymes.
Discussion: This case highlights a rare co-infection of HAV and EBV leading to clinically significant cholestatic hepatitis in an immunocompetent adult. The unusual presentation underscores the importance of always including both hepatotropic and non-hepatotropic viruses in the diagnostic workup of acute hepatitis, especially when liver injury patterns are atypical or accompanied by systemic symptoms such as lymphadenopathy or night sweats. Comprehensive serologic evaluation is critical for accurate diagnosis and optimal management. Early recognition of co-infection can guide appropriate supportive management and avoid unnecessary interventions.
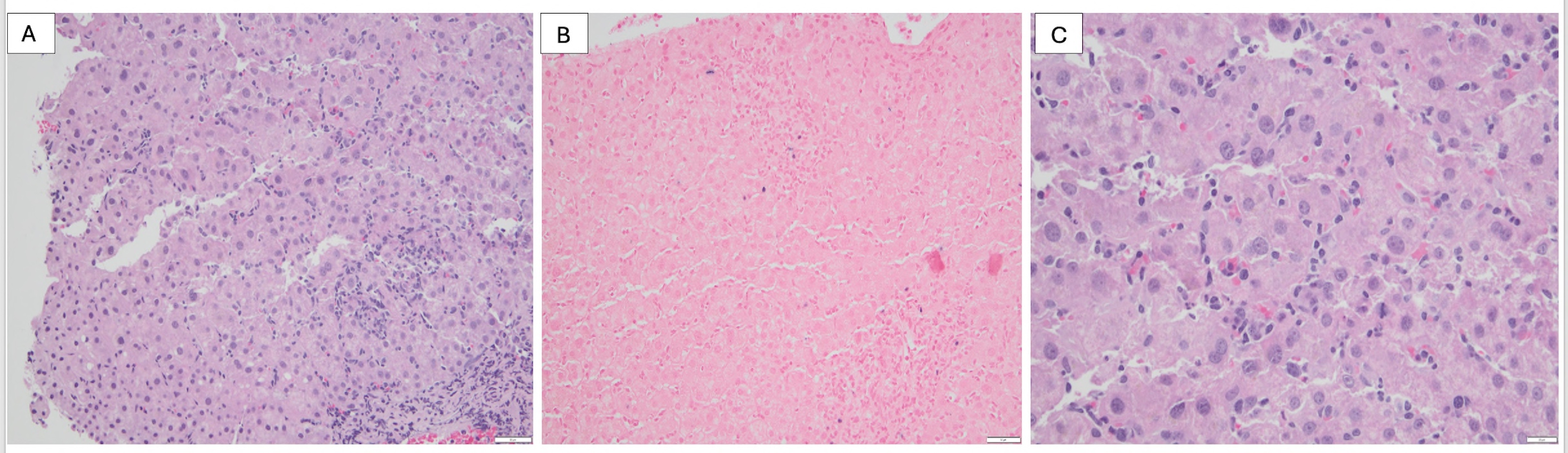
Figure:
Histological images from liver biopsy
Figure 1A-B. H&E stain of EBV Hepatitis showing sinusoidal and lobular inflammation -
Figure 1C - Histological results showing EBER positive (blue color) in liver biopsy result.
Disclosures:
David Okuampa indicated no relevant financial relationships.
Michael Tran indicated no relevant financial relationships.
Sarav Daid indicated no relevant financial relationships.
David Okuampa, MD1, Michael Tran, MD2, Sarav Daid, MD2. P6104 - Double Whammy: A Rare Case of Hepatitis a and EBV-Induced Acute Hepatitis in an Immunocompetent Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
