Tuesday Poster Session
Category: Practice Management
P6197 - Assessing Inpatient Endoscopy Delays: Steps Towards Non-urgent Procedure Triage
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anoushka Dua, MD
University of California Irvine Digestive Health Institute
Irvine, CA
Presenting Author(s)
Anoushka Dua, MD1, Sophie Trujillo, DO2, Robert Fearn, MD2
1University of California Irvine Digestive Health Institute, Irvine, CA; 2University of California Irvine Health, Orange, CA
Introduction: Timely inpatient endoscopy is critical to patient outcomes, hospital length of stay, and healthcare costs but is often subject to non-clinical delays. Existing guidance allows for lower risk inpatient presentations to be discharged with outpatient investigation. The objective of this study was to identify reasons for delays from initial gastroenterology (GI) consult to endoscopic procedure (esophagogastroduodenoscopy and colonoscopy) and to identify opportunities for streamlined management of these cases.
Methods: We conducted a prospective analysis of inpatient GI consults at our institution over a 14-day period in August 2024. Patients were categorized into three groups: procedure completed within 24 hours, procedure completed after 24 hours, and inpatient procedure not completed. Variables analyzed included procedural urgency, reason for delays, day of the week of consultation, and patient demographics.
Results: A total of 80 inpatient GI consults were analyzed. 58 (72.5%) were recommended to have inpatient procedures of whom 48 ultimately went on to have inpatient procedures (Figure 1). Of these, 21 (43.8%) spent >24h awaiting their procedure (a total of 76 patient-nights). Mean time to procedure was 1.8 days (0-8) and mean time to discharge was 6.1 days (0-30). 77% of delays >24h were attributed to operational factors (principally capacity in endoscopy or the OR). Patients consulted on a Saturday waited longest (mean 3.5 days). Patients categorized as ‘emergent’ had the shortest waits (0 days), followed by ‘urgent’ (1.4 days) and ‘non-urgent’ (3.1 days). No patients who underwent procedures classified as ‘non-urgent’ required endotherapy or experienced a change to inpatient management. 27% of patients overall would have met criteria for safe early discharge based on the proposed pathway. This group accounted for 24 nights of hospital stay.
Discussion: The most common causes of inpatient endoscopy delays beyond 24 hours were operational issues, including weekend closures and limited operating room capacity. These challenges could be mitigated by extending endoscopy unit operations to weekends and reducing unnecessary use of inpatient resources. Notably, all procedures categorized as non-urgent neither required endoscopic therapy nor altered inpatient management. Based on these findings, we developed a triage pathway to safely and effectively redirect nonurgent procedures to the outpatient setting on an urgent basis (Figure 1). This pathway is currently undergoing pilot evaluation.
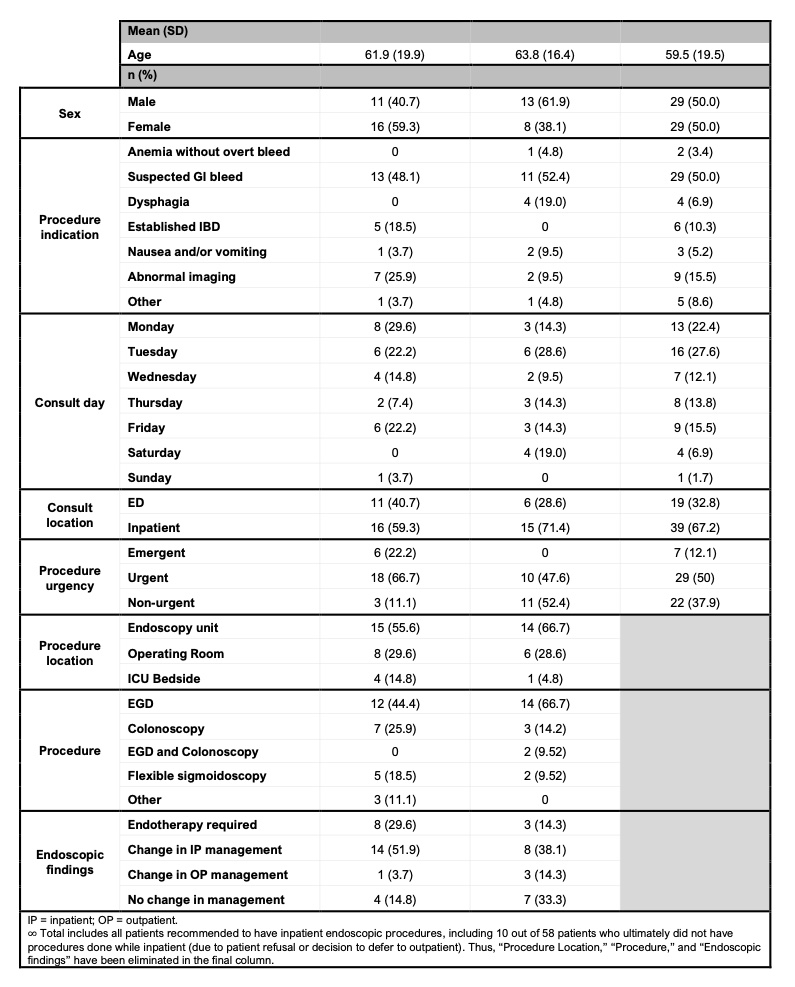
Figure: Summary of baseline inpatient consult audit over two-week period— total, and separated by patients who underwent procedures within and after 24 hours.

Figure: Summary of procedural indications, discharge criteria, and urgency criteria for the urgent outpatient endoscopic procedure pathway, developed as a result of baseline audit research.
Disclosures:
Anoushka Dua indicated no relevant financial relationships.
Sophie Trujillo indicated no relevant financial relationships.
Robert Fearn indicated no relevant financial relationships.
Anoushka Dua, MD1, Sophie Trujillo, DO2, Robert Fearn, MD2. P6197 - Assessing Inpatient Endoscopy Delays: Steps Towards Non-urgent Procedure Triage, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Irvine Digestive Health Institute, Irvine, CA; 2University of California Irvine Health, Orange, CA
Introduction: Timely inpatient endoscopy is critical to patient outcomes, hospital length of stay, and healthcare costs but is often subject to non-clinical delays. Existing guidance allows for lower risk inpatient presentations to be discharged with outpatient investigation. The objective of this study was to identify reasons for delays from initial gastroenterology (GI) consult to endoscopic procedure (esophagogastroduodenoscopy and colonoscopy) and to identify opportunities for streamlined management of these cases.
Methods: We conducted a prospective analysis of inpatient GI consults at our institution over a 14-day period in August 2024. Patients were categorized into three groups: procedure completed within 24 hours, procedure completed after 24 hours, and inpatient procedure not completed. Variables analyzed included procedural urgency, reason for delays, day of the week of consultation, and patient demographics.
Results: A total of 80 inpatient GI consults were analyzed. 58 (72.5%) were recommended to have inpatient procedures of whom 48 ultimately went on to have inpatient procedures (Figure 1). Of these, 21 (43.8%) spent >24h awaiting their procedure (a total of 76 patient-nights). Mean time to procedure was 1.8 days (0-8) and mean time to discharge was 6.1 days (0-30). 77% of delays >24h were attributed to operational factors (principally capacity in endoscopy or the OR). Patients consulted on a Saturday waited longest (mean 3.5 days). Patients categorized as ‘emergent’ had the shortest waits (0 days), followed by ‘urgent’ (1.4 days) and ‘non-urgent’ (3.1 days). No patients who underwent procedures classified as ‘non-urgent’ required endotherapy or experienced a change to inpatient management. 27% of patients overall would have met criteria for safe early discharge based on the proposed pathway. This group accounted for 24 nights of hospital stay.
Discussion: The most common causes of inpatient endoscopy delays beyond 24 hours were operational issues, including weekend closures and limited operating room capacity. These challenges could be mitigated by extending endoscopy unit operations to weekends and reducing unnecessary use of inpatient resources. Notably, all procedures categorized as non-urgent neither required endoscopic therapy nor altered inpatient management. Based on these findings, we developed a triage pathway to safely and effectively redirect nonurgent procedures to the outpatient setting on an urgent basis (Figure 1). This pathway is currently undergoing pilot evaluation.
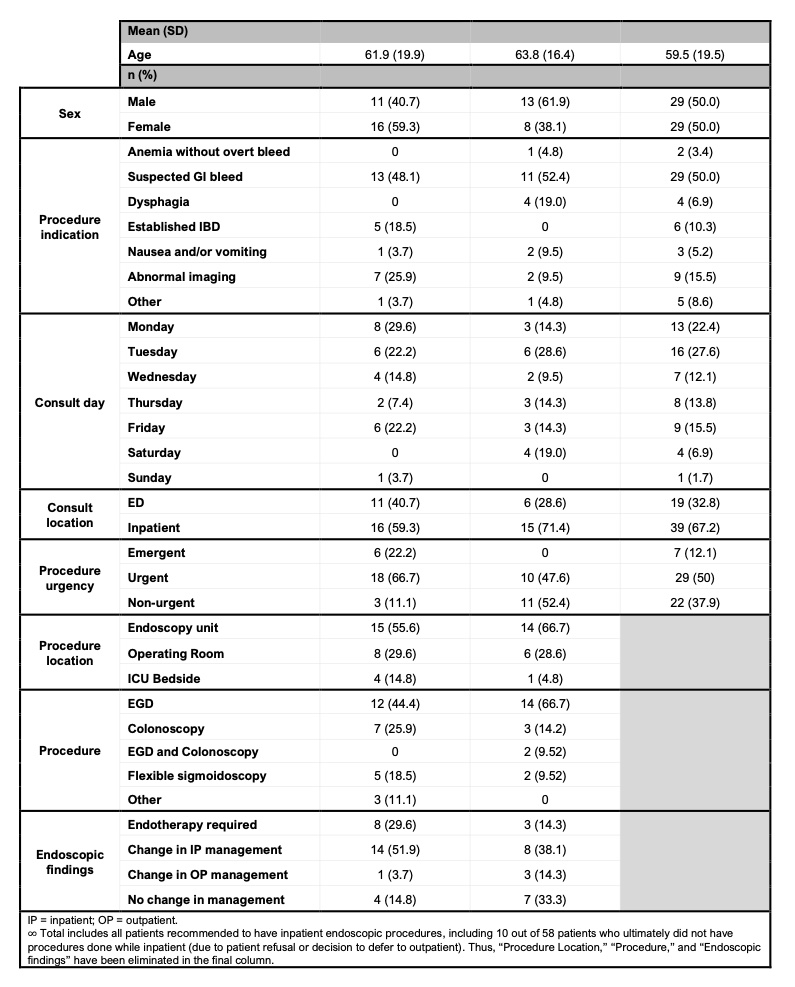
Figure: Summary of baseline inpatient consult audit over two-week period— total, and separated by patients who underwent procedures within and after 24 hours.

Figure: Summary of procedural indications, discharge criteria, and urgency criteria for the urgent outpatient endoscopic procedure pathway, developed as a result of baseline audit research.
Disclosures:
Anoushka Dua indicated no relevant financial relationships.
Sophie Trujillo indicated no relevant financial relationships.
Robert Fearn indicated no relevant financial relationships.
Anoushka Dua, MD1, Sophie Trujillo, DO2, Robert Fearn, MD2. P6197 - Assessing Inpatient Endoscopy Delays: Steps Towards Non-urgent Procedure Triage, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
