Tuesday Poster Session
Category: Practice Management
P6196 - Auto-Fax Intervention Improves Hepatology Referrals in a Dual EMR Urban Health System
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpeg.jpg)
Ahmed Attia, MD (he/him/his)
Transplant Institute, Department of Surgery, George Washington University School of Medicine and Health Science
Washington, DC
Presenting Author(s)
Ahmed Attia, MD1, Abdelrhman Refaey, MD2, Ahmed Ebeid, MD1, Mohamed Abdou, MD1, Khaled Elsakka, MD1, Asil Alsaad, MD1, Ameer Abutaleb, MD3
1Transplant Institute, Department of Surgery, George Washington University School of Medicine and Health Science, Washington, DC; 2Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 3The George Washington Transplant Institute, Department of Surgery, The George Washington University Hospital, Washington, DC
Introduction: Dual electronic medical record (EMR) systems can disrupt referral workflows and patient continuity of care. In our urban health care center, EPIC is the EMR used in the outpatient clinics while Cerner is used for inpatient encounters and transplant institute visits. In September 2024, we implemented an auto-fax system that transmits EPIC referrals to hepatology providers and evaluated its impact on referral completion.
Methods: We analyzed hepatology clinic referrals both preceding and following the auto-fax intervention deployed in September 2024. The primary outcome was the number of referrals. Secondary outcomes included completion rates (patients seen by hepatology) and how many previously missed referrals were recovered after the intervention.
Results: From February 2024 to April 2025, 161 patients were referred to hepatology: 57 pre-intervention and 104 post intervention, representing an 82.5% increase. Referral completion improved significantly, with 25 of 57 patients (43.9%) seen before auto-fax, compared to 64 of 104 (61.5%) after (p < 0.001). Notably, 15 patients from the pre-intervention cohort (26.3%) recovered and scheduled through the new system.
Discussion: Dual-EMR systems can result in significant missed referrals and delayed access to care. This simple, low cost auto-fax intervention proved to be a powerful bridge between two EMRs without an existing interface. It led to a statistically significant increase in referral completion rates (from 43.9% to 61.5%, p < 0.001) and recovery of 26.3% of pre-intervention referrals. Additionally, the intervention was associated with an 82.5% increase in the number of referrals to hepatology, suggesting enhanced provider engagement and improved referral workflows. Future steps include expanding this model to other specialties and advocating for unified EMR integration to further reduce care gaps.
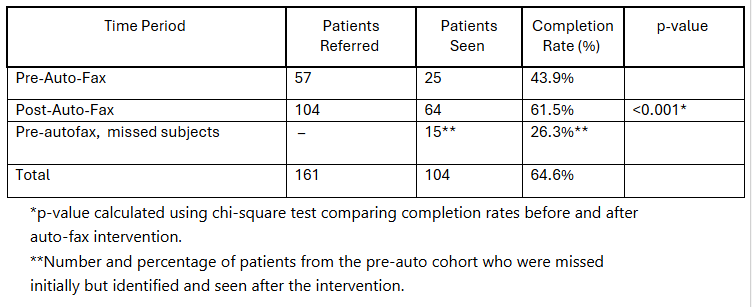
Figure: Table 1. Hepatology referral outcomes before and after implementation of an auto-fax intervention bridging dual EMR systems.

Figure: Pic 1. Average Referral to Appointment Time before and after the Auto-Fax
Disclosures:
Ahmed Attia indicated no relevant financial relationships.
Abdelrhman Refaey indicated no relevant financial relationships.
Ahmed Ebeid indicated no relevant financial relationships.
Mohamed Abdou indicated no relevant financial relationships.
Khaled Elsakka indicated no relevant financial relationships.
Asil Alsaad indicated no relevant financial relationships.
Ameer Abutaleb indicated no relevant financial relationships.
Ahmed Attia, MD1, Abdelrhman Refaey, MD2, Ahmed Ebeid, MD1, Mohamed Abdou, MD1, Khaled Elsakka, MD1, Asil Alsaad, MD1, Ameer Abutaleb, MD3. P6196 - Auto-Fax Intervention Improves Hepatology Referrals in a Dual EMR Urban Health System, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Transplant Institute, Department of Surgery, George Washington University School of Medicine and Health Science, Washington, DC; 2Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 3The George Washington Transplant Institute, Department of Surgery, The George Washington University Hospital, Washington, DC
Introduction: Dual electronic medical record (EMR) systems can disrupt referral workflows and patient continuity of care. In our urban health care center, EPIC is the EMR used in the outpatient clinics while Cerner is used for inpatient encounters and transplant institute visits. In September 2024, we implemented an auto-fax system that transmits EPIC referrals to hepatology providers and evaluated its impact on referral completion.
Methods: We analyzed hepatology clinic referrals both preceding and following the auto-fax intervention deployed in September 2024. The primary outcome was the number of referrals. Secondary outcomes included completion rates (patients seen by hepatology) and how many previously missed referrals were recovered after the intervention.
Results: From February 2024 to April 2025, 161 patients were referred to hepatology: 57 pre-intervention and 104 post intervention, representing an 82.5% increase. Referral completion improved significantly, with 25 of 57 patients (43.9%) seen before auto-fax, compared to 64 of 104 (61.5%) after (p < 0.001). Notably, 15 patients from the pre-intervention cohort (26.3%) recovered and scheduled through the new system.
Discussion: Dual-EMR systems can result in significant missed referrals and delayed access to care. This simple, low cost auto-fax intervention proved to be a powerful bridge between two EMRs without an existing interface. It led to a statistically significant increase in referral completion rates (from 43.9% to 61.5%, p < 0.001) and recovery of 26.3% of pre-intervention referrals. Additionally, the intervention was associated with an 82.5% increase in the number of referrals to hepatology, suggesting enhanced provider engagement and improved referral workflows. Future steps include expanding this model to other specialties and advocating for unified EMR integration to further reduce care gaps.
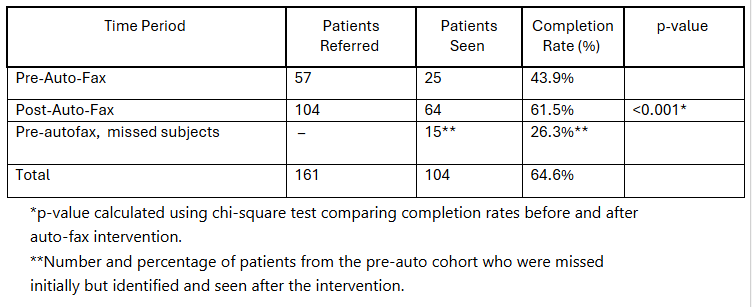
Figure: Table 1. Hepatology referral outcomes before and after implementation of an auto-fax intervention bridging dual EMR systems.

Figure: Pic 1. Average Referral to Appointment Time before and after the Auto-Fax
Disclosures:
Ahmed Attia indicated no relevant financial relationships.
Abdelrhman Refaey indicated no relevant financial relationships.
Ahmed Ebeid indicated no relevant financial relationships.
Mohamed Abdou indicated no relevant financial relationships.
Khaled Elsakka indicated no relevant financial relationships.
Asil Alsaad indicated no relevant financial relationships.
Ameer Abutaleb indicated no relevant financial relationships.
Ahmed Attia, MD1, Abdelrhman Refaey, MD2, Ahmed Ebeid, MD1, Mohamed Abdou, MD1, Khaled Elsakka, MD1, Asil Alsaad, MD1, Ameer Abutaleb, MD3. P6196 - Auto-Fax Intervention Improves Hepatology Referrals in a Dual EMR Urban Health System, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
