Tuesday Poster Session
Category: Practice Management
P6189 - Promoting Patient-Centered Language in Gastroenterology Documentation: The Impact of an Educational Intervention
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Abdelrhman Refaey, MD
Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences
Teaneck, NJ
Presenting Author(s)
Abdelrhman Refaey, MD1, Maria Elena. Ruiz, MD2, Mrudula Bandaru, MD3, Robert Gordon, DO3, Susie Park, MD3, Zeina Bani Hani, MBBS3, Ahmed Attia, MD4, Mohamed Abdou, MD4, Pavan Vemulakonda, MD3, Valerie S. Stark, MD, MPH3, Asil Alsaad, MD4, Ahmed Ebeid, MD4, Maxwell S. Madani, BA5, Calvin Tabetah, BA5, Sarah A. Bokaee, BA6, Marie L. Borum, MD, EdD, MPH, FACG1
1Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 2Division of Infectious Diseases, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 3Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 4Transplant Institute, Department of Surgery, George Washington University School of Medicine and Health Science, Washington, DC; 5George Washington University School of Medicine and Health Sciences, Washington, DC; 6George Washington University School of Medicine and Health Sciences, Washington DC, DC
Introduction: Stigmatizing language in medical documentation can compromise patient trust, engagement, and communication. In gastroenterology (GI), terms such as morbid obesity, alcoholic, drug abuse or addict, non-compliant, poor historian, and poor prep can carry negative connotations. This study evaluated the impact of an educational intervention on the prevalence of stigmatizing language in GI medical records at an urban university medical center in effort to promote respectful, patient-centered documentation.
Methods: A review of outpatient and endoscopy records during a 2-month pre-intervention (pre) period was conducted to identify stigmatizing terminology. An educational session introduced evidence-based alternatives for stigmatizing terms: BMI for obesity, alcohol use disorder for alcoholic, substance use disorder for drug abuse or addict, unable to adhere to recommendations because of a stated reason instead of non-compliant and Boston Bowel Preparation Scale (BBPS) instead of poor prep. Records were assessed for 2-months post-intervention (post). Analysis was performed using Fischer Exact test with significance set at p< 0.05.
Results: 3417 records were reviewed (pre: 1653, post: 1764). Use of the term obesity significantly decreased (pre: 5.6%, post: 3.6%; p=0.012), while use of BMI significantly increased (pre: 8.8%, post: 16.6%; p< 0.001). There was a non-significant decrease in the term alcoholic (pre: 1.1%, post: 0.6%; p=0.17), with an increase in alcohol use disorder (pre: 0.12%, post: 0.4%; p=0.11). There was no significant difference in the use of the terms drug abuse or addict (pre: 0.73%, post: 0.45%; p=0.36), non-compliant (pre: 0.24%; post: 0.06%; p=0.21) or poor historian (pre: 0.18%; post: 0.34%; p=0.51).
Of 1028 colonoscopy records, 873 had optimal preparation and were excluded resulting in 155 (pre: 99 pre; post: 56) eligible records. There was a significant decrease in the use of poor prep (pre: 51.5%; post: 23.2%; p=0.002) with a significant increase in the use of BBPS < 6 (pre: 48.5%; post: 76.8%; p=0.001).
Discussion: Stigmatizing language was infrequently used in GI documentation at baseline, suggesting an existing culture of thoughtful and respectful communication. Nevertheless, a brief targeted intervention led to a significant decrease in the use of the terms obesity and poor prep to more objective, patient-centered alternatives. These findings demonstrate the effectiveness of low-resource educational efforts to foster inclusive and respectful medical documentation.
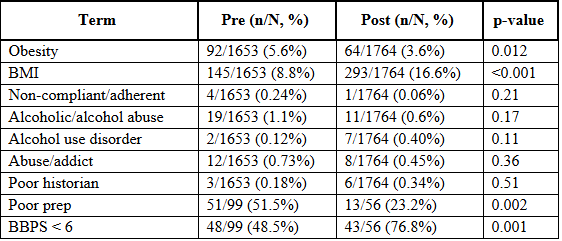
Figure: Table 1. Frequency and Statistical Comparison of Stigmatizing vs. Patient-Centered Terminology Pre- and Post-Intervention.
Disclosures:
Abdelrhman Refaey indicated no relevant financial relationships.
Maria Ruiz indicated no relevant financial relationships.
Mrudula Bandaru indicated no relevant financial relationships.
Robert Gordon indicated no relevant financial relationships.
Susie Park indicated no relevant financial relationships.
Zeina Bani Hani indicated no relevant financial relationships.
Ahmed Attia indicated no relevant financial relationships.
Mohamed Abdou indicated no relevant financial relationships.
Pavan Vemulakonda indicated no relevant financial relationships.
Valerie Stark indicated no relevant financial relationships.
Asil Alsaad indicated no relevant financial relationships.
Ahmed Ebeid indicated no relevant financial relationships.
Maxwell Madani indicated no relevant financial relationships.
Calvin Tabetah indicated no relevant financial relationships.
Sarah Bokaee indicated no relevant financial relationships.
Marie Borum indicated no relevant financial relationships.
Abdelrhman Refaey, MD1, Maria Elena. Ruiz, MD2, Mrudula Bandaru, MD3, Robert Gordon, DO3, Susie Park, MD3, Zeina Bani Hani, MBBS3, Ahmed Attia, MD4, Mohamed Abdou, MD4, Pavan Vemulakonda, MD3, Valerie S. Stark, MD, MPH3, Asil Alsaad, MD4, Ahmed Ebeid, MD4, Maxwell S. Madani, BA5, Calvin Tabetah, BA5, Sarah A. Bokaee, BA6, Marie L. Borum, MD, EdD, MPH, FACG1. P6189 - Promoting Patient-Centered Language in Gastroenterology Documentation: The Impact of an Educational Intervention, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 2Division of Infectious Diseases, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 3Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 4Transplant Institute, Department of Surgery, George Washington University School of Medicine and Health Science, Washington, DC; 5George Washington University School of Medicine and Health Sciences, Washington, DC; 6George Washington University School of Medicine and Health Sciences, Washington DC, DC
Introduction: Stigmatizing language in medical documentation can compromise patient trust, engagement, and communication. In gastroenterology (GI), terms such as morbid obesity, alcoholic, drug abuse or addict, non-compliant, poor historian, and poor prep can carry negative connotations. This study evaluated the impact of an educational intervention on the prevalence of stigmatizing language in GI medical records at an urban university medical center in effort to promote respectful, patient-centered documentation.
Methods: A review of outpatient and endoscopy records during a 2-month pre-intervention (pre) period was conducted to identify stigmatizing terminology. An educational session introduced evidence-based alternatives for stigmatizing terms: BMI for obesity, alcohol use disorder for alcoholic, substance use disorder for drug abuse or addict, unable to adhere to recommendations because of a stated reason instead of non-compliant and Boston Bowel Preparation Scale (BBPS) instead of poor prep. Records were assessed for 2-months post-intervention (post). Analysis was performed using Fischer Exact test with significance set at p< 0.05.
Results: 3417 records were reviewed (pre: 1653, post: 1764). Use of the term obesity significantly decreased (pre: 5.6%, post: 3.6%; p=0.012), while use of BMI significantly increased (pre: 8.8%, post: 16.6%; p< 0.001). There was a non-significant decrease in the term alcoholic (pre: 1.1%, post: 0.6%; p=0.17), with an increase in alcohol use disorder (pre: 0.12%, post: 0.4%; p=0.11). There was no significant difference in the use of the terms drug abuse or addict (pre: 0.73%, post: 0.45%; p=0.36), non-compliant (pre: 0.24%; post: 0.06%; p=0.21) or poor historian (pre: 0.18%; post: 0.34%; p=0.51).
Of 1028 colonoscopy records, 873 had optimal preparation and were excluded resulting in 155 (pre: 99 pre; post: 56) eligible records. There was a significant decrease in the use of poor prep (pre: 51.5%; post: 23.2%; p=0.002) with a significant increase in the use of BBPS < 6 (pre: 48.5%; post: 76.8%; p=0.001).
Discussion: Stigmatizing language was infrequently used in GI documentation at baseline, suggesting an existing culture of thoughtful and respectful communication. Nevertheless, a brief targeted intervention led to a significant decrease in the use of the terms obesity and poor prep to more objective, patient-centered alternatives. These findings demonstrate the effectiveness of low-resource educational efforts to foster inclusive and respectful medical documentation.
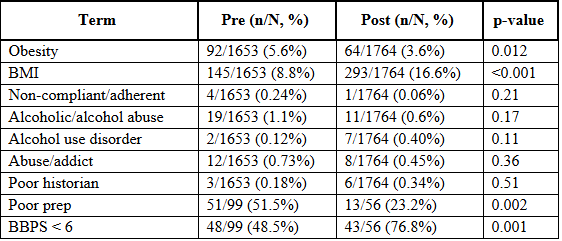
Figure: Table 1. Frequency and Statistical Comparison of Stigmatizing vs. Patient-Centered Terminology Pre- and Post-Intervention.
Disclosures:
Abdelrhman Refaey indicated no relevant financial relationships.
Maria Ruiz indicated no relevant financial relationships.
Mrudula Bandaru indicated no relevant financial relationships.
Robert Gordon indicated no relevant financial relationships.
Susie Park indicated no relevant financial relationships.
Zeina Bani Hani indicated no relevant financial relationships.
Ahmed Attia indicated no relevant financial relationships.
Mohamed Abdou indicated no relevant financial relationships.
Pavan Vemulakonda indicated no relevant financial relationships.
Valerie Stark indicated no relevant financial relationships.
Asil Alsaad indicated no relevant financial relationships.
Ahmed Ebeid indicated no relevant financial relationships.
Maxwell Madani indicated no relevant financial relationships.
Calvin Tabetah indicated no relevant financial relationships.
Sarah Bokaee indicated no relevant financial relationships.
Marie Borum indicated no relevant financial relationships.
Abdelrhman Refaey, MD1, Maria Elena. Ruiz, MD2, Mrudula Bandaru, MD3, Robert Gordon, DO3, Susie Park, MD3, Zeina Bani Hani, MBBS3, Ahmed Attia, MD4, Mohamed Abdou, MD4, Pavan Vemulakonda, MD3, Valerie S. Stark, MD, MPH3, Asil Alsaad, MD4, Ahmed Ebeid, MD4, Maxwell S. Madani, BA5, Calvin Tabetah, BA5, Sarah A. Bokaee, BA6, Marie L. Borum, MD, EdD, MPH, FACG1. P6189 - Promoting Patient-Centered Language in Gastroenterology Documentation: The Impact of an Educational Intervention, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
