Tuesday Poster Session
Category: Small Intestine
P6249 - Gastrointestinal Involvement as a Diagnostic Window for Systemic AL Amyloidosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Vishnu Yanamaladoddi, MD
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
Vishnu Yanamaladoddi, MD1, Silpa Choday, MD1, Ashujot K. Dang, MD2, Vikash Kumar, MD1, Sandeep Chikkam, MD, DNBSS3, Indu Srinivasan, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2University of California Riverside School of Medicine, Riverside, CA; 3Asian Institute of Gastroenterology, Hyderabad, Telangana, India
Introduction: Amyloidosis is a systemic disease characterized by extracellular deposition of misfolded protein fibrils. AL (light chain) amyloidosis is most common in multiple myeloma, driven by excess monoclonal light chains from plasma cells. The kidneys, heart, and liver are commonly involved. Gastrointestinal (GI) amyloidosis are less common and can present with nonspecific symptoms like abdominal pain, diarrhea, or weight loss, often mimicking malignancy. Diagnosis hinges on histologic evaluation with Congo red staining.
Case Description/
Methods: A 51-year-old male with no known medical history presented with abdominal pain, night sweats, back pain, weight loss, and alternating diarrhea and constipation. Symptoms progressed over months but were attributed to voluntary weight loss. He was previously evaluated in Mexico, with imaging and labs showing rectal wall thickening, retroperitoneal lymphadenopathy, and lytic bone lesions.
He denied alcohol, tobacco, or drug use. Family history included a sister with GI malignancy. Exam revealed mild right upper quadrant and lumbar tenderness. Labs showed alkaline phosphatase 247 U/L, AST 75 U/L, lipase 489 U/L, hemoglobin 15.7 g/dL. Serum protein electrophoresis showed gamma globulin 0.47 g/dL. Serum free kappa light chains were 1369.2 mg/L, kappa-to-lambda ratio 185. Imaging showed lytic bone lesions, a 2.4 x 4.2 cm liver lesion, and mediastinal lymphadenopathy.
Endoscopy showed junction inflammation, duodenal edema with ulcers, gastropathy, and terminal ileitis. Duodenal biopsy demonstrated villous blunting, lamina propria edema, and eosinophilic deposits. Congo red staining confirmed amyloid deposition. Bone marrow biopsy confirmed multiple myeloma with AL amyloidosis. Despite chemotherapy, his condition deteriorated with jaundice, renal failure, and cardiac involvement. Liver and kidney biopsies confirmed systemic amyloid. He was not a transplant candidate and opted for hospice.
Discussion: This case highlights the GI tract as a rare but critical site for early diagnosis of AL amyloidosis. In this patient, biopsy of duodenal lesions led to the diagnosis before other organ systems decompensated. While amyloidosis often presents with renal or cardiac involvement, GI symptoms may precede them and offer a window for earlier detection. A high index of suspicion and prompt histologic evaluation, particularly in patients with unexplained abdominal symptoms and systemic findings, can lead to earlier diagnosis and intervention before irreversible organ damage occurs.
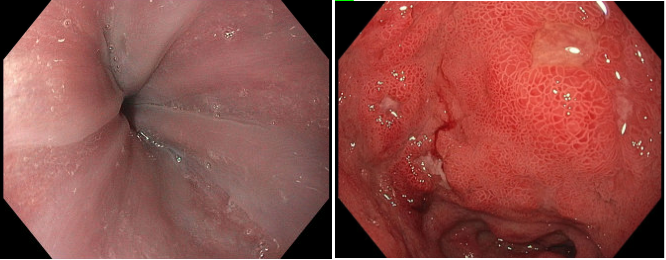
Figure: Upper endoscopy showing edema and inflammation
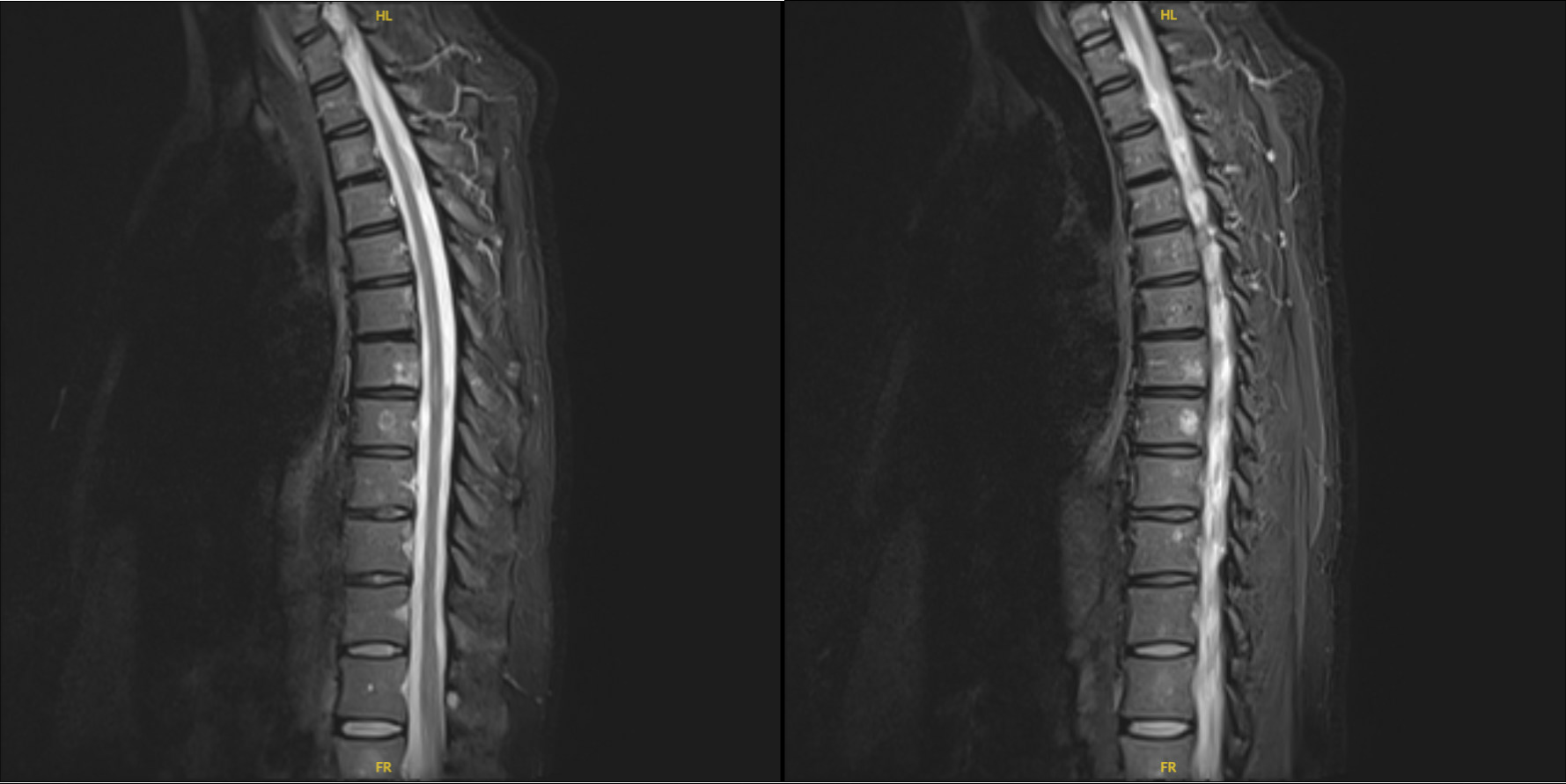
Figure: Imaging showing lytic lesions at multiple spinal levels
Disclosures:
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Silpa Choday indicated no relevant financial relationships.
Ashujot Dang indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Sandeep Chikkam indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Vishnu Yanamaladoddi, MD1, Silpa Choday, MD1, Ashujot K. Dang, MD2, Vikash Kumar, MD1, Sandeep Chikkam, MD, DNBSS3, Indu Srinivasan, MD1. P6249 - Gastrointestinal Involvement as a Diagnostic Window for Systemic AL Amyloidosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University School of Medicine, Phoenix, AZ; 2University of California Riverside School of Medicine, Riverside, CA; 3Asian Institute of Gastroenterology, Hyderabad, Telangana, India
Introduction: Amyloidosis is a systemic disease characterized by extracellular deposition of misfolded protein fibrils. AL (light chain) amyloidosis is most common in multiple myeloma, driven by excess monoclonal light chains from plasma cells. The kidneys, heart, and liver are commonly involved. Gastrointestinal (GI) amyloidosis are less common and can present with nonspecific symptoms like abdominal pain, diarrhea, or weight loss, often mimicking malignancy. Diagnosis hinges on histologic evaluation with Congo red staining.
Case Description/
Methods: A 51-year-old male with no known medical history presented with abdominal pain, night sweats, back pain, weight loss, and alternating diarrhea and constipation. Symptoms progressed over months but were attributed to voluntary weight loss. He was previously evaluated in Mexico, with imaging and labs showing rectal wall thickening, retroperitoneal lymphadenopathy, and lytic bone lesions.
He denied alcohol, tobacco, or drug use. Family history included a sister with GI malignancy. Exam revealed mild right upper quadrant and lumbar tenderness. Labs showed alkaline phosphatase 247 U/L, AST 75 U/L, lipase 489 U/L, hemoglobin 15.7 g/dL. Serum protein electrophoresis showed gamma globulin 0.47 g/dL. Serum free kappa light chains were 1369.2 mg/L, kappa-to-lambda ratio 185. Imaging showed lytic bone lesions, a 2.4 x 4.2 cm liver lesion, and mediastinal lymphadenopathy.
Endoscopy showed junction inflammation, duodenal edema with ulcers, gastropathy, and terminal ileitis. Duodenal biopsy demonstrated villous blunting, lamina propria edema, and eosinophilic deposits. Congo red staining confirmed amyloid deposition. Bone marrow biopsy confirmed multiple myeloma with AL amyloidosis. Despite chemotherapy, his condition deteriorated with jaundice, renal failure, and cardiac involvement. Liver and kidney biopsies confirmed systemic amyloid. He was not a transplant candidate and opted for hospice.
Discussion: This case highlights the GI tract as a rare but critical site for early diagnosis of AL amyloidosis. In this patient, biopsy of duodenal lesions led to the diagnosis before other organ systems decompensated. While amyloidosis often presents with renal or cardiac involvement, GI symptoms may precede them and offer a window for earlier detection. A high index of suspicion and prompt histologic evaluation, particularly in patients with unexplained abdominal symptoms and systemic findings, can lead to earlier diagnosis and intervention before irreversible organ damage occurs.
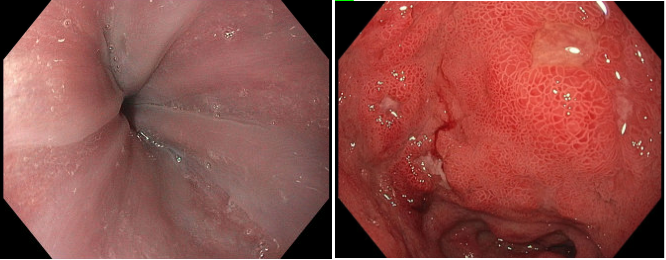
Figure: Upper endoscopy showing edema and inflammation
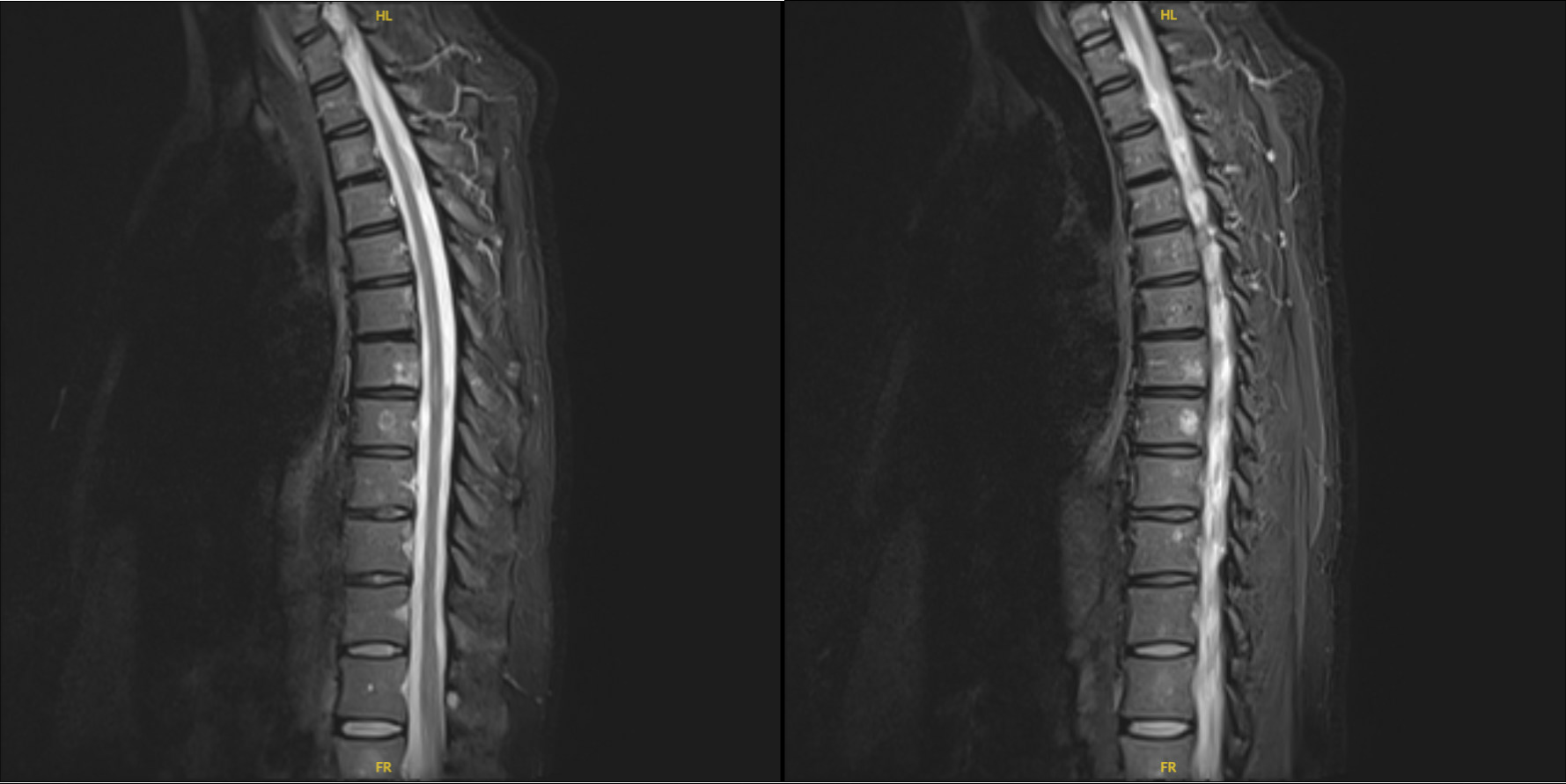
Figure: Imaging showing lytic lesions at multiple spinal levels
Disclosures:
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Silpa Choday indicated no relevant financial relationships.
Ashujot Dang indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Sandeep Chikkam indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Vishnu Yanamaladoddi, MD1, Silpa Choday, MD1, Ashujot K. Dang, MD2, Vikash Kumar, MD1, Sandeep Chikkam, MD, DNBSS3, Indu Srinivasan, MD1. P6249 - Gastrointestinal Involvement as a Diagnostic Window for Systemic AL Amyloidosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
