Tuesday Poster Session
Category: Small Intestine
P6243 - When the Gut Doesn’t Forget: Recurrent Eosinophilic Gastroenteritis Following COVID-19 Infection
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Andreina Martinez Paulino, MD (she/her/hers)
Jersey City Medical Center
Jersey City, NJ
Presenting Author(s)
Andreina Martinez Paulino, MD, Fnu Soxi, MD, Dheeraj Pinninty, MD
Jersey City Medical Center, Jersey City, NJ
Introduction: Eosinophilic gastroenteritis (EGE) is a rare inflammatory disorder of the stomach and small intestine, characterized by dense eosinophilic infiltration in the absence of secondary causes (e.g., parasitic infection, malignancy, or systemic eosinophilic syndrome). Its prevalence in the United States is approximately 5.1 per 100,000.
Case Description/
Methods: A 28-year-old man presented with a three-day history of profuse, watery diarrhea and lower abdominal pain. He reported three similar episodes over the past four years, the first occurring weeks after a hospitalization for COVID-19. He denied food intolerances, atopic disorders, or significant environmental exposures.
Laboratory tests showed WBC 15.1 × 10³/µL (16% eosinophils), and elevated CRP (1.6 mg/dL) and stool calprotectin (53 µg/g). Celiac and parasitic studies, ANCA panel, ASCA titers, serum tryptase and IgE levels, and cultures were unremarkable. CT showed diffuse gastritis and enterocolitis with skip lesions, suggesting IBD.
EGD showed normal esophagus and stomach but moderate, diffuse edema and erythema in the duodenum. Colonoscopy showed a grossly normal terminal ileum and colon. Duodenal biopsies revealed preserved villi with a marked eosinophilic infiltration ( >100/HPF) in the lamina propria and submucosa, without lymphocytosis, celiac changes, dysplasia, or malignancy. Gastric biopsies showed 15-20 eosinophils/HPF, and a random ascending colon biopsy revealed reactive lymphoid aggregates with focal eosinophilia. Collectively, these findings supported the diagnosis of EGE.
The patient received IV methylprednisolone for two days with rapid resolution of diarrhea and eosinophilia. He was discharged on a 4-week prednisone taper with GI follow-up.
Discussion: Recent evidence shows that COVID-19 can trigger eosinophilic gastrointestinal disorders (EGIDs) like EGE, by disrupting gut immunity and causing a type 2 helper T-cell response that recruits eosinophils into the intestinal lining. Multiple case reports document EGE onset within weeks of acute COVID-19, even in patients without a history of atopy. In these cases, symptoms and imaging often resemble IBD, but targeted biopsies reveal eosinophilic infiltration essential for an accurate diagnosis. As post-COVID-19 EGE becomes increasingly recognized, clinicians should consider EGIDs in any patient with recent SARS-CoV-2 infection who presents with diarrhea and abdominal pain, especially when imaging suggests IBD but endoscopic mucosa appears deceptively normal.
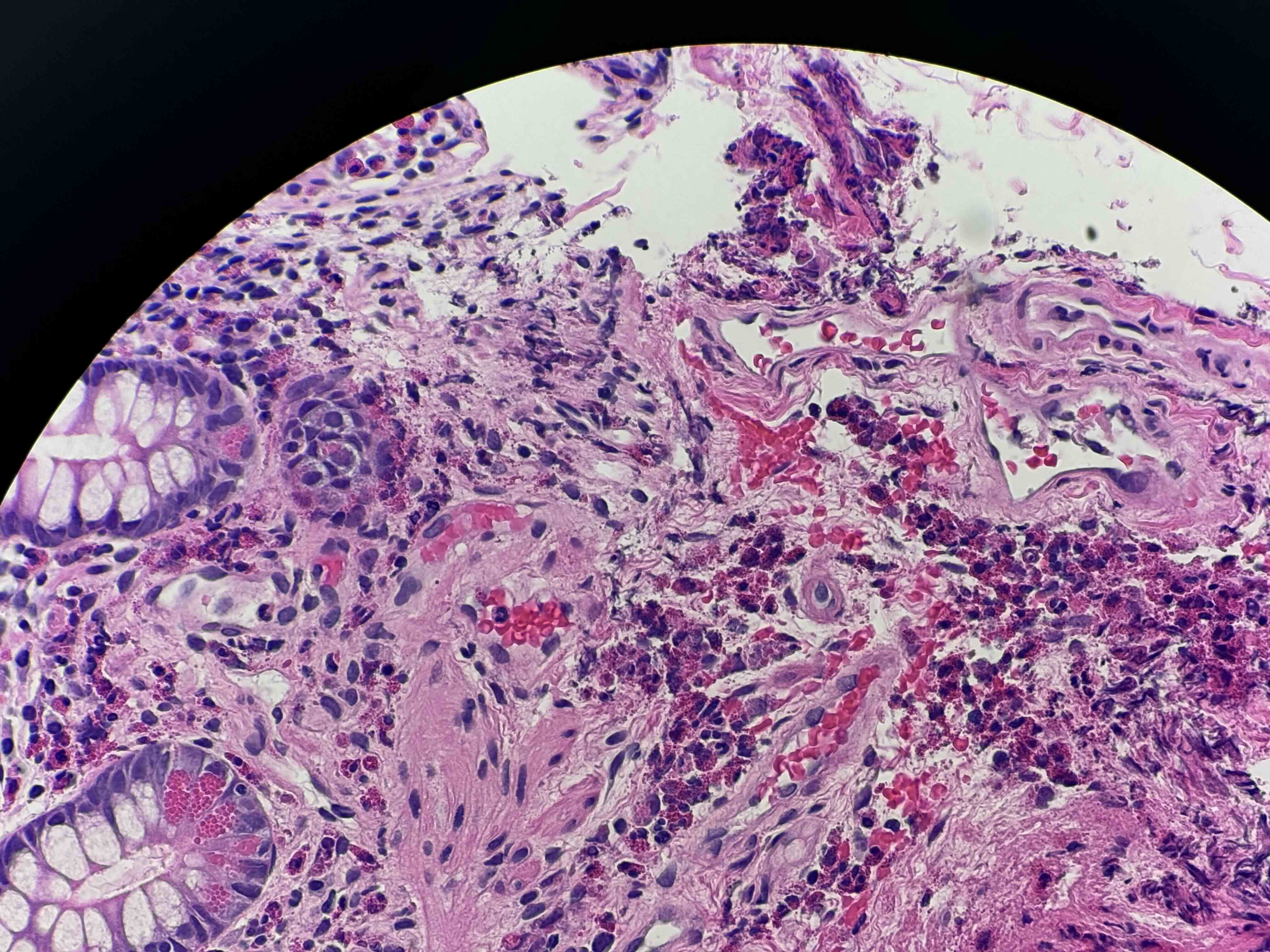
Figure: Biopsy of colonic mucosa with increased localized eosinophils in the lamina propria
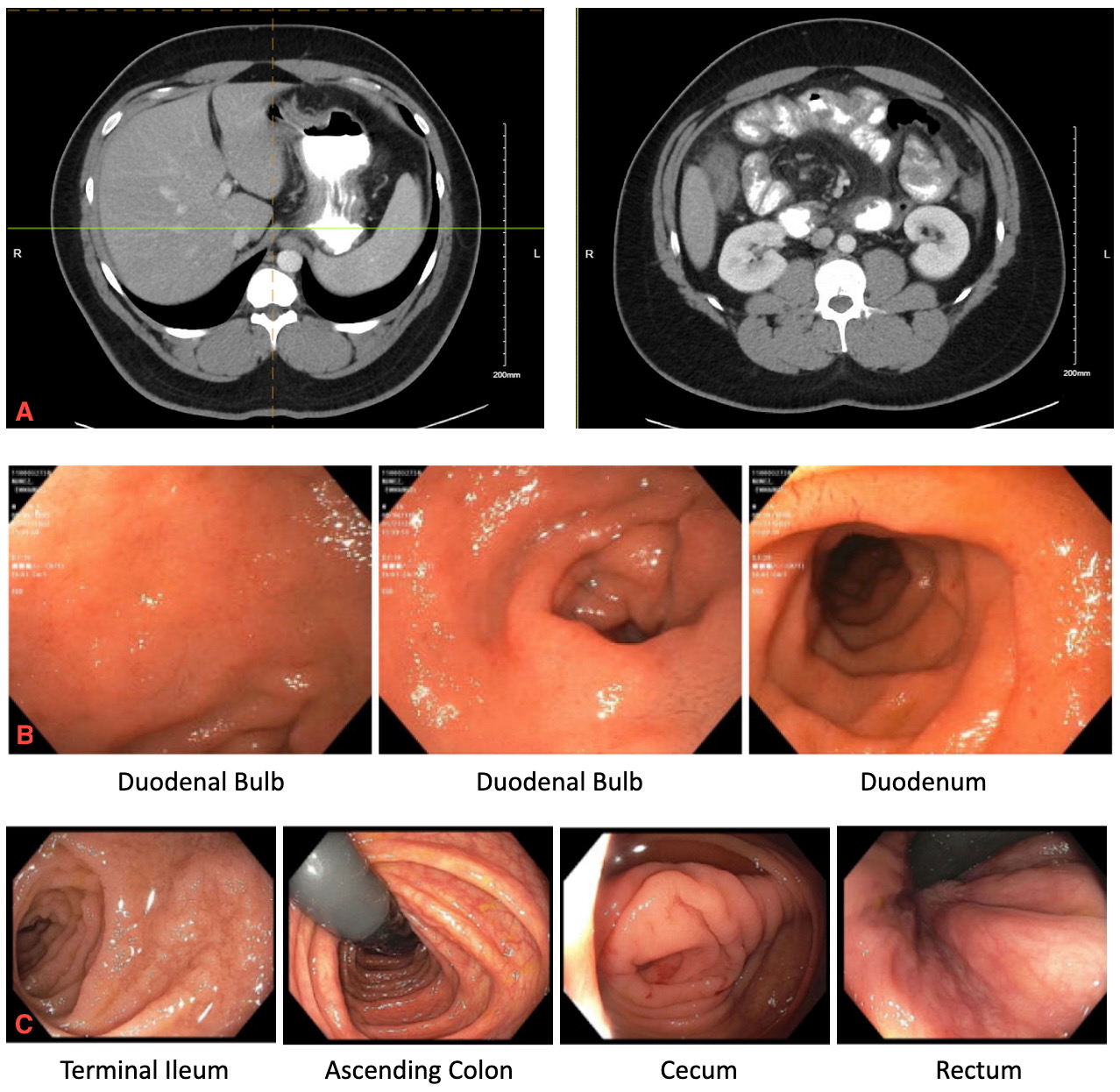
Figure: CT abdomen and pelvis (A) showing distal gastric, small bowel wall and colonic wall thickening suggestive of enterocolitis. EGD (B) revealing diffuse duodenal erythema, and colonoscopy (C) with normal terminal ileum, ascending colon, cecum, and rectum.
Disclosures:
Andreina Martinez Paulino indicated no relevant financial relationships.
Fnu Soxi indicated no relevant financial relationships.
Dheeraj Pinninty indicated no relevant financial relationships.
Andreina Martinez Paulino, MD, Fnu Soxi, MD, Dheeraj Pinninty, MD. P6243 - When the Gut Doesn’t Forget: Recurrent Eosinophilic Gastroenteritis Following COVID-19 Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Jersey City Medical Center, Jersey City, NJ
Introduction: Eosinophilic gastroenteritis (EGE) is a rare inflammatory disorder of the stomach and small intestine, characterized by dense eosinophilic infiltration in the absence of secondary causes (e.g., parasitic infection, malignancy, or systemic eosinophilic syndrome). Its prevalence in the United States is approximately 5.1 per 100,000.
Case Description/
Methods: A 28-year-old man presented with a three-day history of profuse, watery diarrhea and lower abdominal pain. He reported three similar episodes over the past four years, the first occurring weeks after a hospitalization for COVID-19. He denied food intolerances, atopic disorders, or significant environmental exposures.
Laboratory tests showed WBC 15.1 × 10³/µL (16% eosinophils), and elevated CRP (1.6 mg/dL) and stool calprotectin (53 µg/g). Celiac and parasitic studies, ANCA panel, ASCA titers, serum tryptase and IgE levels, and cultures were unremarkable. CT showed diffuse gastritis and enterocolitis with skip lesions, suggesting IBD.
EGD showed normal esophagus and stomach but moderate, diffuse edema and erythema in the duodenum. Colonoscopy showed a grossly normal terminal ileum and colon. Duodenal biopsies revealed preserved villi with a marked eosinophilic infiltration ( >100/HPF) in the lamina propria and submucosa, without lymphocytosis, celiac changes, dysplasia, or malignancy. Gastric biopsies showed 15-20 eosinophils/HPF, and a random ascending colon biopsy revealed reactive lymphoid aggregates with focal eosinophilia. Collectively, these findings supported the diagnosis of EGE.
The patient received IV methylprednisolone for two days with rapid resolution of diarrhea and eosinophilia. He was discharged on a 4-week prednisone taper with GI follow-up.
Discussion: Recent evidence shows that COVID-19 can trigger eosinophilic gastrointestinal disorders (EGIDs) like EGE, by disrupting gut immunity and causing a type 2 helper T-cell response that recruits eosinophils into the intestinal lining. Multiple case reports document EGE onset within weeks of acute COVID-19, even in patients without a history of atopy. In these cases, symptoms and imaging often resemble IBD, but targeted biopsies reveal eosinophilic infiltration essential for an accurate diagnosis. As post-COVID-19 EGE becomes increasingly recognized, clinicians should consider EGIDs in any patient with recent SARS-CoV-2 infection who presents with diarrhea and abdominal pain, especially when imaging suggests IBD but endoscopic mucosa appears deceptively normal.
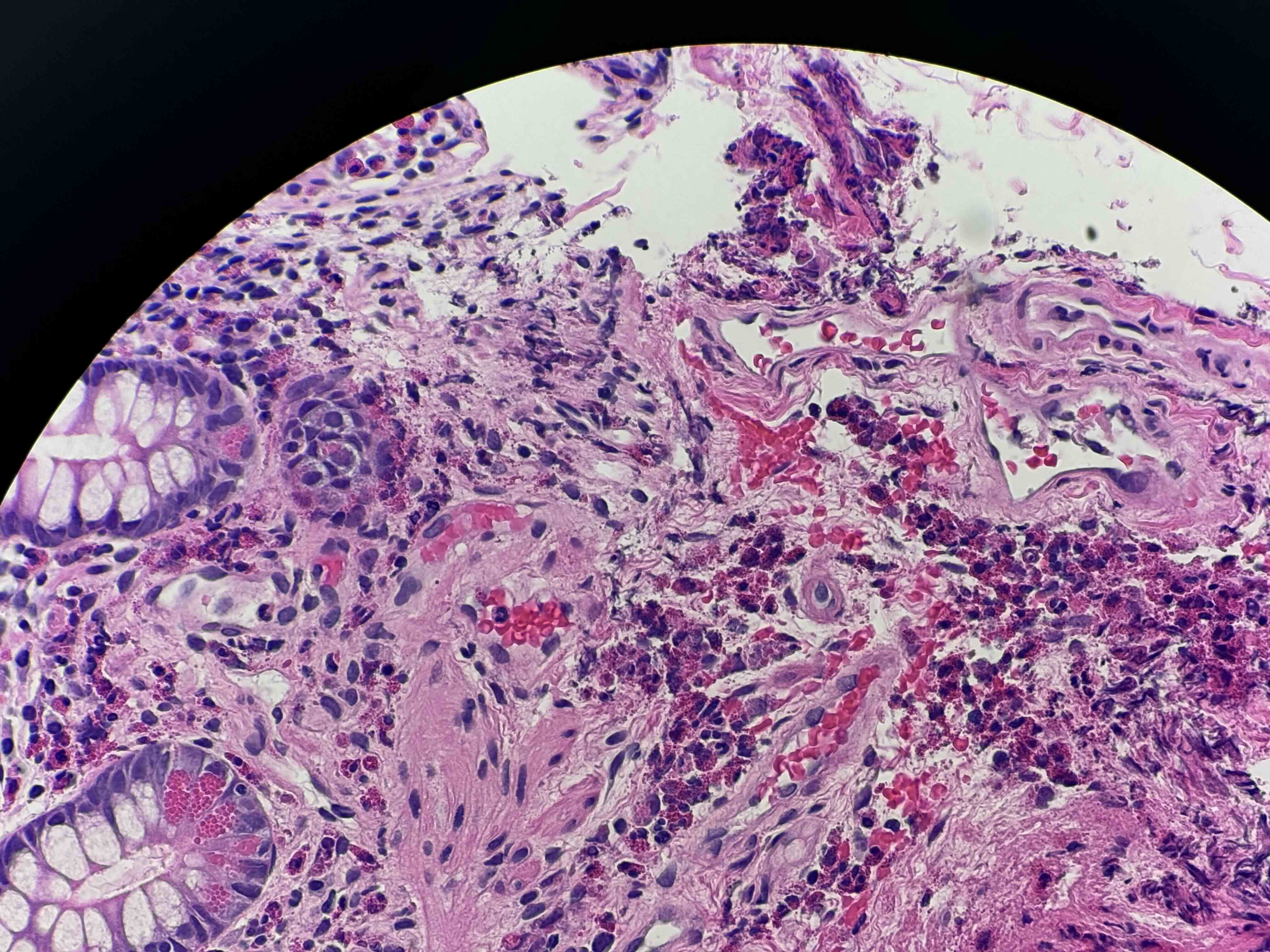
Figure: Biopsy of colonic mucosa with increased localized eosinophils in the lamina propria
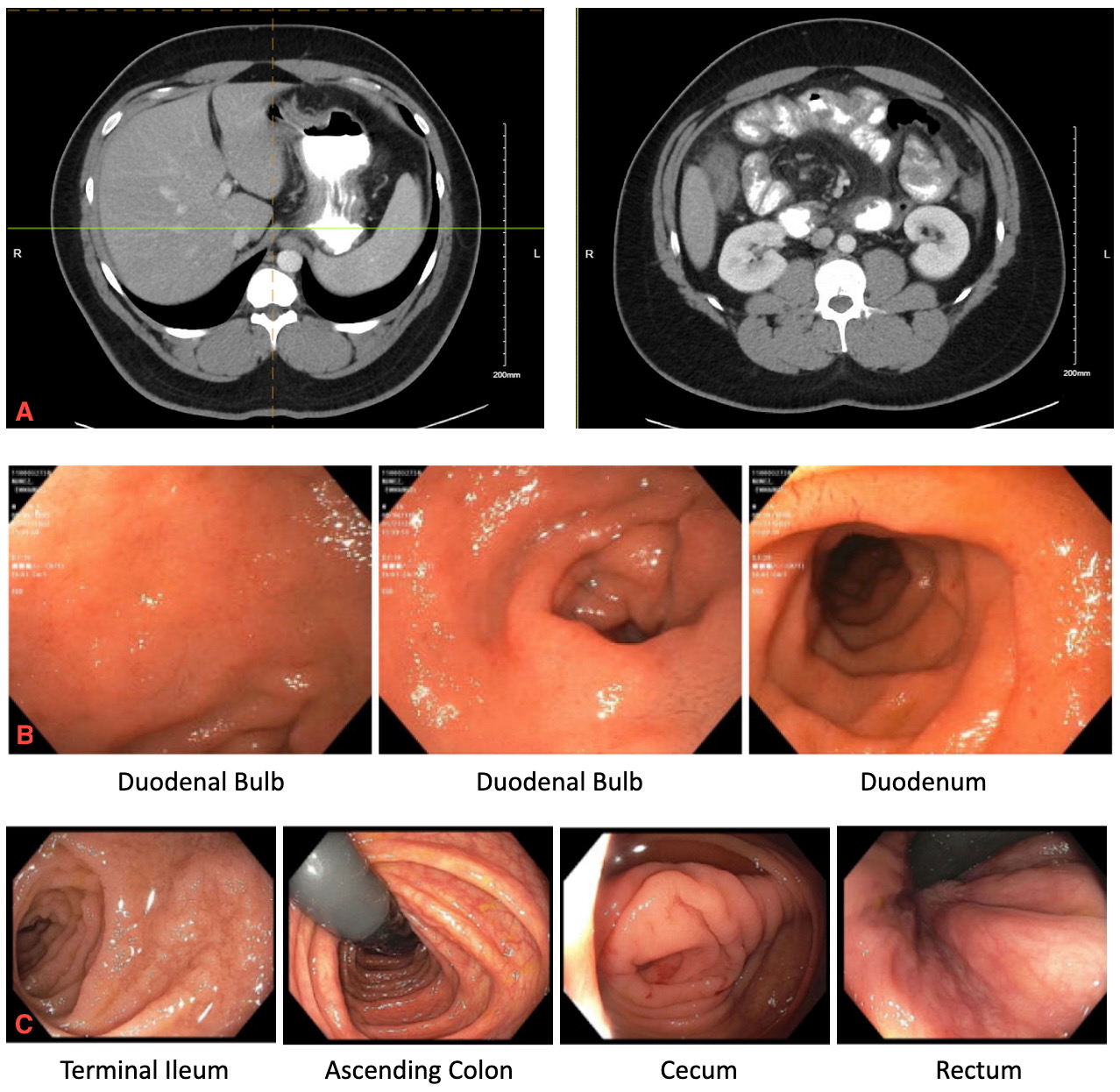
Figure: CT abdomen and pelvis (A) showing distal gastric, small bowel wall and colonic wall thickening suggestive of enterocolitis. EGD (B) revealing diffuse duodenal erythema, and colonoscopy (C) with normal terminal ileum, ascending colon, cecum, and rectum.
Disclosures:
Andreina Martinez Paulino indicated no relevant financial relationships.
Fnu Soxi indicated no relevant financial relationships.
Dheeraj Pinninty indicated no relevant financial relationships.
Andreina Martinez Paulino, MD, Fnu Soxi, MD, Dheeraj Pinninty, MD. P6243 - When the Gut Doesn’t Forget: Recurrent Eosinophilic Gastroenteritis Following COVID-19 Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
