Tuesday Poster Session
Category: Small Intestine
P6214 - Combined Oral Contraceptives Are Associated With Increased Risk of Developing Small Intestinal Bacterial Overgrowth in Pre-Menopausal Women
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JK
Jacqueline Khalil, DO, MS
Case Western Reserve University / MetroHealth
Cleveland, OH
Presenting Author(s)
Jacqueline Khalil, DO, MS1, Gengqing Song, MD, PhD2, Kaynat Khalid, DO2
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2Case Western Reserve University/Metro Health, Cleveland, OH
Introduction: SIBO disproportionately affects women. Sex hormones may influence the higher prevalence of SIBO in females. This study investigated the effects of combined oral contraceptives (COC) on SIBO and its related symptoms, medication use, and diagnostic testing in pre-menopausal women.
Methods: Utilizing the TriNetX platform, we conducted a large population-based cohort study involving pre-menopausal women aged 18-49, with and without COC (estrogen and progesterone). 1:1 propensity score matching was performed to adjust for age, race, and ethnicity. Exclusion criteria included ICD codes for menopause, UC, Crohn’s, diabetes, IBS, PPI usage, gastroparesis, lactose intolerance, functional dyspepsia, pancreatic insufficiency, liver disease, intestinal pseudo-obstruction, adhesions, connective tissue disorders, opiate use, intestinal malignant neoplasms, bariatric and surgical procedures. Odds ratios with 95% confidence intervals were calculated.
Results: After applying exclusion criteria, we identified 1,443,477 pre-menopausal women prescribed COC and 11,929,503 not prescribed COC. Post-propensity matching, each cohort comprised 1,421,461 patients. 239 pre-menopausal women prescribed COC developed SIBO at least 30 days after being prescribed COC compared to 96 pre-menopausal women not prescribed COC (OR=2.49, 95% CI [1.96-3.15]). These associations persisted in sensitivity analysis over 3 years (OR=1.56 95% CI [1.16-2.28]). COC were associated with increased GI symptoms including abdominal pain (OR=2.11 95% CI [2.06-2.16]), gas pain (OR=2.98 95% CI [2.79-3.18]), abdominal distention (OR=3.02 95% CI [2.93-3.12]), flatulence (OR=2.84 95% CI [2.67-3.03]), intestinal malabsorption (OR=1.94 95% CI [1.85-2.04]), abnormal weight loss (OR=2.92 95% CI [2.83-3.01]), diarrhea (OR=2.21 95% CI [2.17-2.25]), and b12 deficiency (OR=2.16 95% CI [1.97-2.37]). Medications including rifaximin (OR=3.53 95% CI [3.12-4.01]) and neomycin (OR=2.25 95% CI [2.19-2.32]) were more likely to be prescribed in pre-menopausal women on COC. Colonoscopy (OR=2.28 95% CI[1.65-3.15]), and hydrogen/methane breath test (OR 1.79 95% CI [1.58-2.02]) were more likely to be performed in pre-menopausal women prescribed COC.
Discussion: Our study reveals a compelling association between COC and an increased risk of developing SIBO, which persists overtime. Additionally, COC are correlated with elevated gastrointestinal symptoms, augmented medication utilization, and heightened diagnostic testing commonly seen in patients with SIBO.
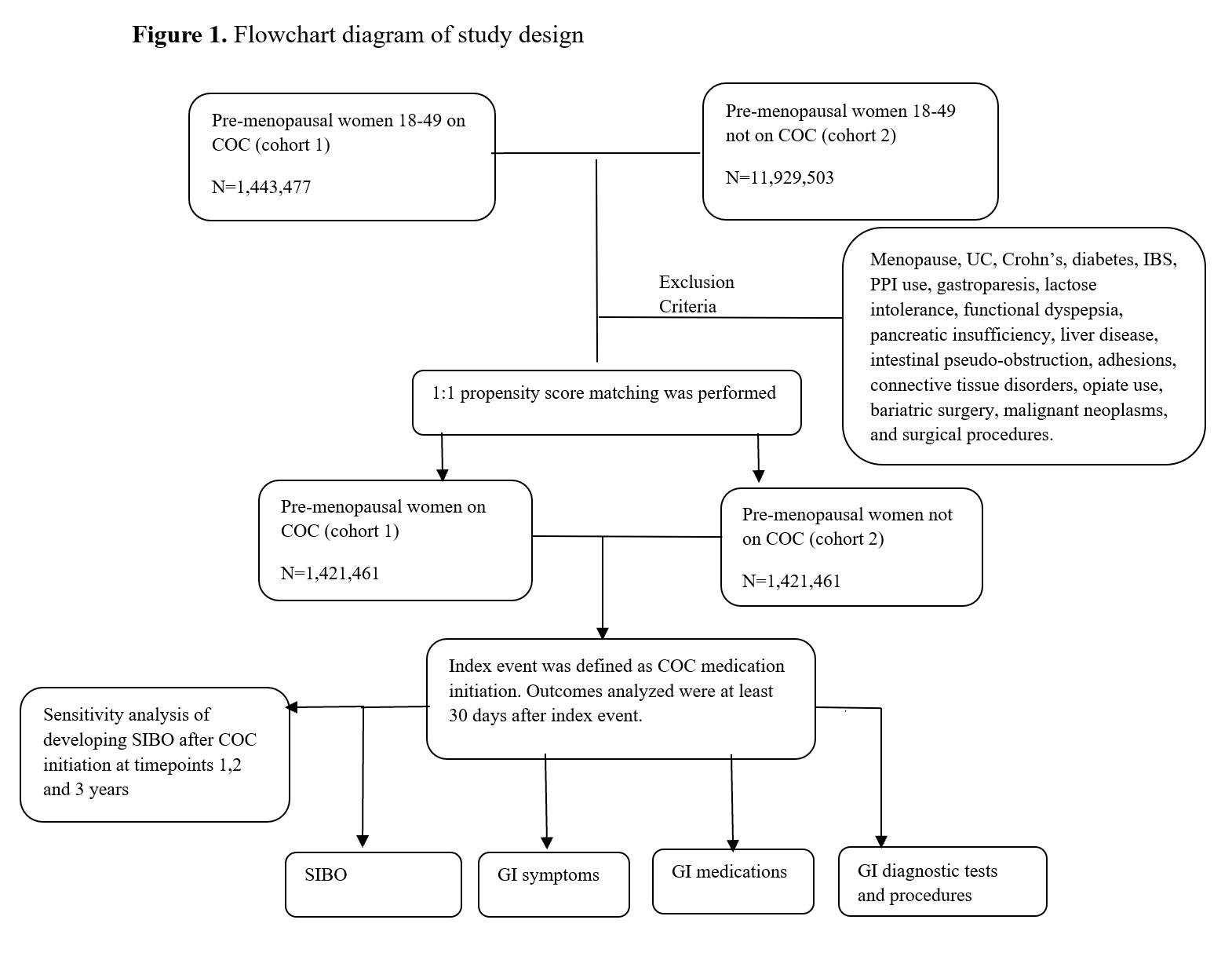
Figure: Flowchart Diagram of Study Design
Disclosures:
Jacqueline Khalil indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Kaynat Khalid indicated no relevant financial relationships.
Jacqueline Khalil, DO, MS1, Gengqing Song, MD, PhD2, Kaynat Khalid, DO2. P6214 - Combined Oral Contraceptives Are Associated With Increased Risk of Developing Small Intestinal Bacterial Overgrowth in Pre-Menopausal Women, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2Case Western Reserve University/Metro Health, Cleveland, OH
Introduction: SIBO disproportionately affects women. Sex hormones may influence the higher prevalence of SIBO in females. This study investigated the effects of combined oral contraceptives (COC) on SIBO and its related symptoms, medication use, and diagnostic testing in pre-menopausal women.
Methods: Utilizing the TriNetX platform, we conducted a large population-based cohort study involving pre-menopausal women aged 18-49, with and without COC (estrogen and progesterone). 1:1 propensity score matching was performed to adjust for age, race, and ethnicity. Exclusion criteria included ICD codes for menopause, UC, Crohn’s, diabetes, IBS, PPI usage, gastroparesis, lactose intolerance, functional dyspepsia, pancreatic insufficiency, liver disease, intestinal pseudo-obstruction, adhesions, connective tissue disorders, opiate use, intestinal malignant neoplasms, bariatric and surgical procedures. Odds ratios with 95% confidence intervals were calculated.
Results: After applying exclusion criteria, we identified 1,443,477 pre-menopausal women prescribed COC and 11,929,503 not prescribed COC. Post-propensity matching, each cohort comprised 1,421,461 patients. 239 pre-menopausal women prescribed COC developed SIBO at least 30 days after being prescribed COC compared to 96 pre-menopausal women not prescribed COC (OR=2.49, 95% CI [1.96-3.15]). These associations persisted in sensitivity analysis over 3 years (OR=1.56 95% CI [1.16-2.28]). COC were associated with increased GI symptoms including abdominal pain (OR=2.11 95% CI [2.06-2.16]), gas pain (OR=2.98 95% CI [2.79-3.18]), abdominal distention (OR=3.02 95% CI [2.93-3.12]), flatulence (OR=2.84 95% CI [2.67-3.03]), intestinal malabsorption (OR=1.94 95% CI [1.85-2.04]), abnormal weight loss (OR=2.92 95% CI [2.83-3.01]), diarrhea (OR=2.21 95% CI [2.17-2.25]), and b12 deficiency (OR=2.16 95% CI [1.97-2.37]). Medications including rifaximin (OR=3.53 95% CI [3.12-4.01]) and neomycin (OR=2.25 95% CI [2.19-2.32]) were more likely to be prescribed in pre-menopausal women on COC. Colonoscopy (OR=2.28 95% CI[1.65-3.15]), and hydrogen/methane breath test (OR 1.79 95% CI [1.58-2.02]) were more likely to be performed in pre-menopausal women prescribed COC.
Discussion: Our study reveals a compelling association between COC and an increased risk of developing SIBO, which persists overtime. Additionally, COC are correlated with elevated gastrointestinal symptoms, augmented medication utilization, and heightened diagnostic testing commonly seen in patients with SIBO.
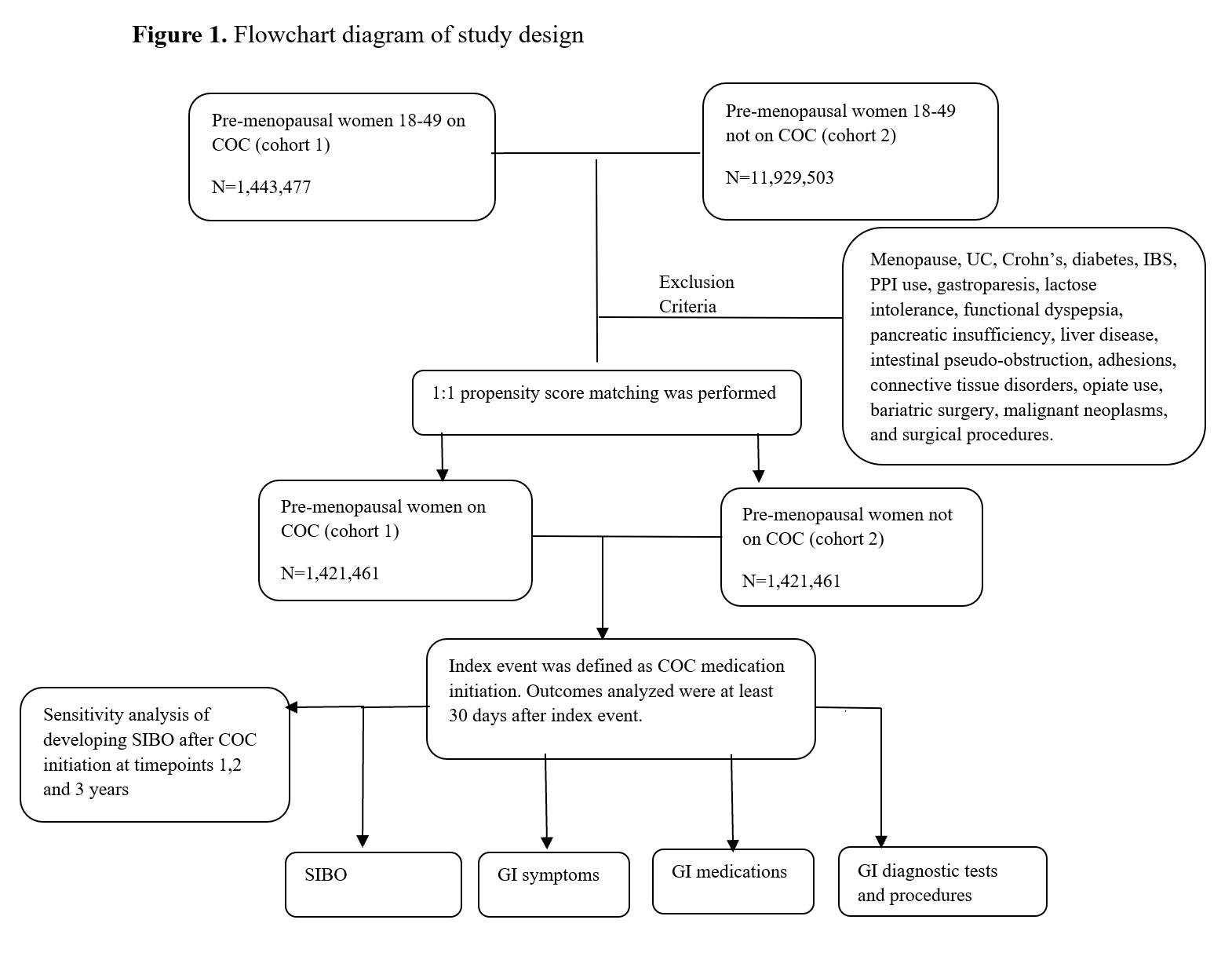
Figure: Flowchart Diagram of Study Design
Disclosures:
Jacqueline Khalil indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Kaynat Khalid indicated no relevant financial relationships.
Jacqueline Khalil, DO, MS1, Gengqing Song, MD, PhD2, Kaynat Khalid, DO2. P6214 - Combined Oral Contraceptives Are Associated With Increased Risk of Developing Small Intestinal Bacterial Overgrowth in Pre-Menopausal Women, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
