Tuesday Poster Session
Category: Practice Management
P6173 - Gastroenterology Patients’ Understanding of Their Inpatient Care and Treatment Team
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nisha R. Sanghani, DO
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Nisha R. Sanghani, DO1, Monica Dzwonkowski, DO1, Emilie S. Kim, MD2, Het Patel, DO3, Ryan Lee, BS3, Renata Carneiro, PhD1, Berhanu Geme, MD4, Noel Martins, MD5, Kimberly J. Chaput, DO6
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Hospital, Bethlehem, PA; 3St. Luke's Hospital, Bethlehem, PA; 4St Luke’s University Health Network, Center Valley, PA; 5St. Luke's University Health Network, Center Valley, PA; 6St Luke's Gastroenterology, Center Valley, PA
Introduction: Patients’ knowledge of their inpatient treatment team and plan is essential for the delivery of safe and effective care as well as increased patient satisfaction. Patients’ understanding of their medical conditions is influenced by age, gender, and education. Prior studies demonstrate that many admitted patients do not know their management plan and are unable to identify their physicians. This may lead to decreased patient satisfaction, poor follow up, less active patient participation in shared decision-making, and ultimately worse patient outcomes. This study aims to identify gaps in patients’ understanding of their gastrointestinal (GI) care to eventually implement strategies to improve patient satisfaction and outcomes.
Methods: A prospective survey study was administered to adult patients admitted at St. Luke’s Bethlehem Hospital with gastroenterology consultation. Patients with altered mentation or dementia were excluded. Data was summarized using frequencies and percentages. Analysis was done through Chi-square, Fisher’s Exact test, and univariate logistic regression using Stata.
Results: Of the 47 patients surveyed, 88% of patients stated their gastroenterologist introduced themselves, but only 41% knew the difference between residents, fellows, and attendings and 38% forgot their physicians’ identities after introduction. Interestingly, female patients knew the plan significantly more frequently than male patients did (OR= 3.95 95% CI 1.13-13.71, p=0.031; Table 1). 82% of patients did not have an attire preference for physicians. 100% of patients aged 18-64 years followed up outpatient while only 77% of patients aged 65 years and older did (p=0.042; Table 2).
Discussion: While previous studies have indicated that patients have an attire preference, specifically white coats with formal clothing, we found that 82% of patients do not factor in attire with their satisfaction with their GI care. Additionally, prior studies have shown that females have higher health literacy and seek out medical knowledge more frequently than their male counterparts. Our study supports this existing literature, as females were significantly more knowledgeable about their GI treatment plan. Finally, there are gaps in physician recognition and elderly patient follow up. Future studies could target improving GI health education in our male population, providing business cards to help with physician identification, and promoting outpatient follow up for our elderly patients through scheduled reminders.
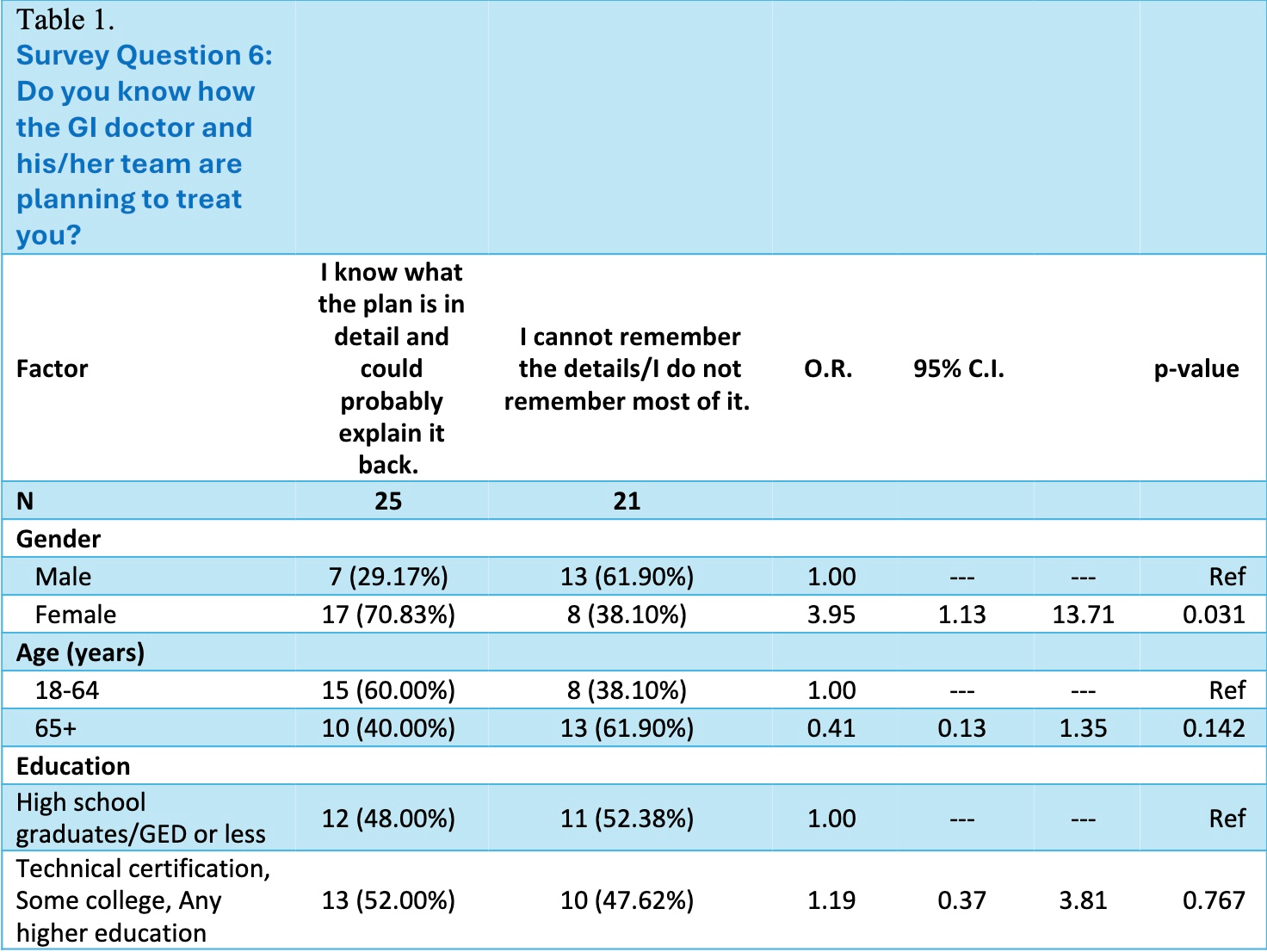
Figure: How patients' demographics impact their knowledge of their treatment plan
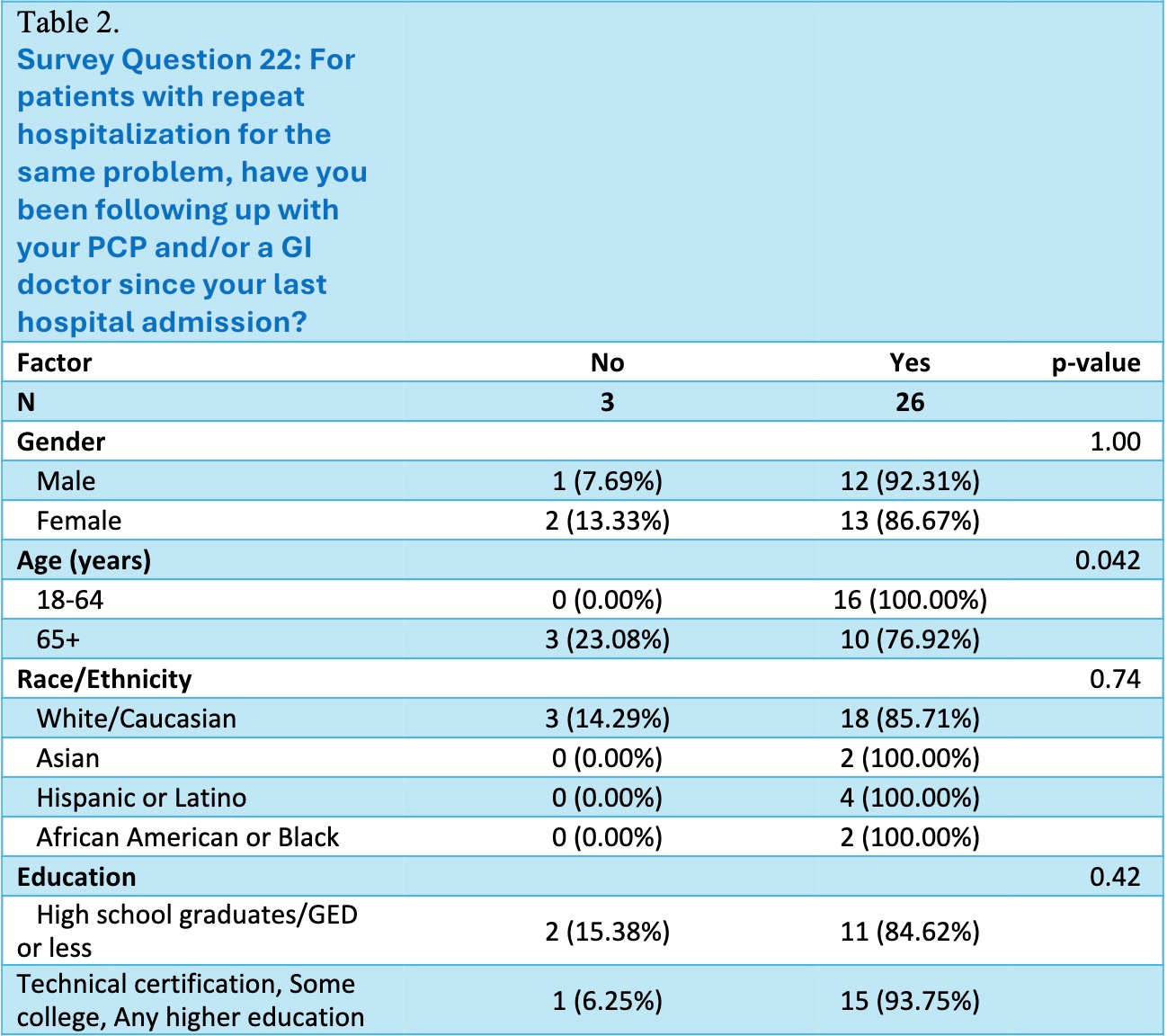
Figure: Influence of demographics on patient follow up in the outpatient setting.
Disclosures:
Nisha Sanghani indicated no relevant financial relationships.
Monica Dzwonkowski indicated no relevant financial relationships.
Emilie Kim indicated no relevant financial relationships.
Het Patel indicated no relevant financial relationships.
Ryan Lee indicated no relevant financial relationships.
Renata Carneiro indicated no relevant financial relationships.
Berhanu Geme indicated no relevant financial relationships.
Noel Martins indicated no relevant financial relationships.
Kimberly Chaput indicated no relevant financial relationships.
Nisha R. Sanghani, DO1, Monica Dzwonkowski, DO1, Emilie S. Kim, MD2, Het Patel, DO3, Ryan Lee, BS3, Renata Carneiro, PhD1, Berhanu Geme, MD4, Noel Martins, MD5, Kimberly J. Chaput, DO6. P6173 - Gastroenterology Patients’ Understanding of Their Inpatient Care and Treatment Team, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Hospital, Bethlehem, PA; 3St. Luke's Hospital, Bethlehem, PA; 4St Luke’s University Health Network, Center Valley, PA; 5St. Luke's University Health Network, Center Valley, PA; 6St Luke's Gastroenterology, Center Valley, PA
Introduction: Patients’ knowledge of their inpatient treatment team and plan is essential for the delivery of safe and effective care as well as increased patient satisfaction. Patients’ understanding of their medical conditions is influenced by age, gender, and education. Prior studies demonstrate that many admitted patients do not know their management plan and are unable to identify their physicians. This may lead to decreased patient satisfaction, poor follow up, less active patient participation in shared decision-making, and ultimately worse patient outcomes. This study aims to identify gaps in patients’ understanding of their gastrointestinal (GI) care to eventually implement strategies to improve patient satisfaction and outcomes.
Methods: A prospective survey study was administered to adult patients admitted at St. Luke’s Bethlehem Hospital with gastroenterology consultation. Patients with altered mentation or dementia were excluded. Data was summarized using frequencies and percentages. Analysis was done through Chi-square, Fisher’s Exact test, and univariate logistic regression using Stata.
Results: Of the 47 patients surveyed, 88% of patients stated their gastroenterologist introduced themselves, but only 41% knew the difference between residents, fellows, and attendings and 38% forgot their physicians’ identities after introduction. Interestingly, female patients knew the plan significantly more frequently than male patients did (OR= 3.95 95% CI 1.13-13.71, p=0.031; Table 1). 82% of patients did not have an attire preference for physicians. 100% of patients aged 18-64 years followed up outpatient while only 77% of patients aged 65 years and older did (p=0.042; Table 2).
Discussion: While previous studies have indicated that patients have an attire preference, specifically white coats with formal clothing, we found that 82% of patients do not factor in attire with their satisfaction with their GI care. Additionally, prior studies have shown that females have higher health literacy and seek out medical knowledge more frequently than their male counterparts. Our study supports this existing literature, as females were significantly more knowledgeable about their GI treatment plan. Finally, there are gaps in physician recognition and elderly patient follow up. Future studies could target improving GI health education in our male population, providing business cards to help with physician identification, and promoting outpatient follow up for our elderly patients through scheduled reminders.
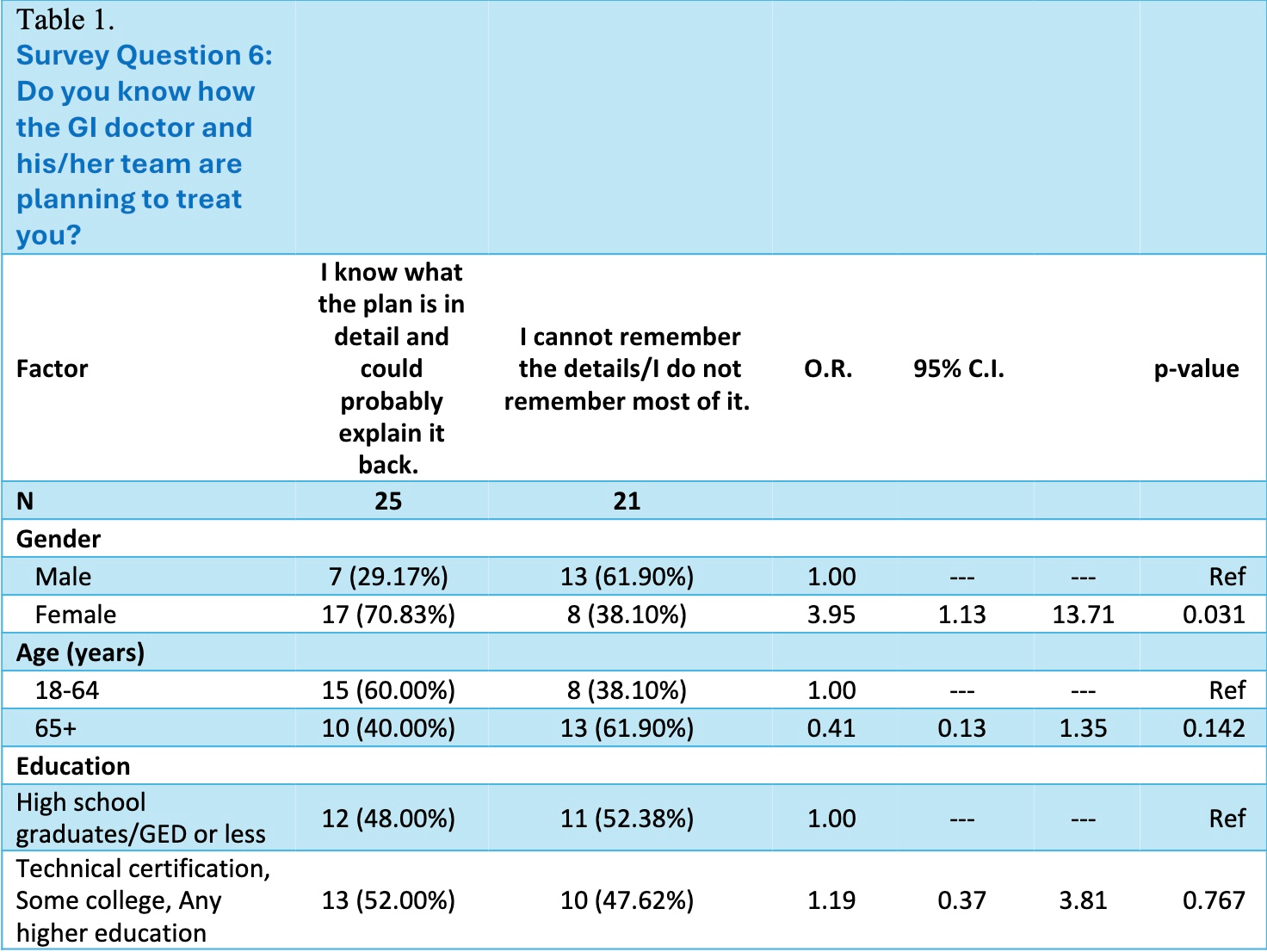
Figure: How patients' demographics impact their knowledge of their treatment plan
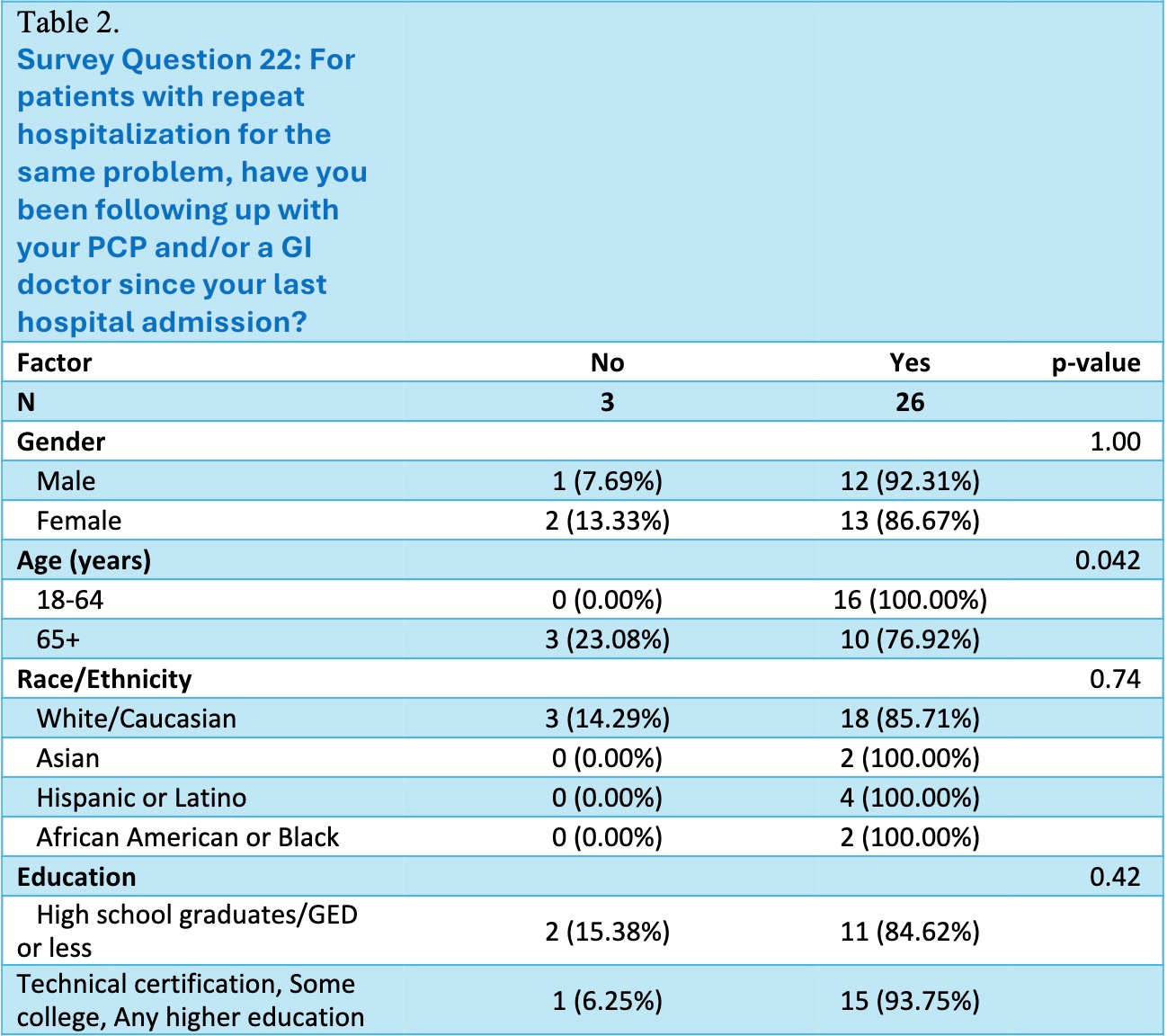
Figure: Influence of demographics on patient follow up in the outpatient setting.
Disclosures:
Nisha Sanghani indicated no relevant financial relationships.
Monica Dzwonkowski indicated no relevant financial relationships.
Emilie Kim indicated no relevant financial relationships.
Het Patel indicated no relevant financial relationships.
Ryan Lee indicated no relevant financial relationships.
Renata Carneiro indicated no relevant financial relationships.
Berhanu Geme indicated no relevant financial relationships.
Noel Martins indicated no relevant financial relationships.
Kimberly Chaput indicated no relevant financial relationships.
Nisha R. Sanghani, DO1, Monica Dzwonkowski, DO1, Emilie S. Kim, MD2, Het Patel, DO3, Ryan Lee, BS3, Renata Carneiro, PhD1, Berhanu Geme, MD4, Noel Martins, MD5, Kimberly J. Chaput, DO6. P6173 - Gastroenterology Patients’ Understanding of Their Inpatient Care and Treatment Team, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
