Tuesday Poster Session
Category: Practice Management
P6164 - Use of a Pre-Procedural Checklist to Improve Percutaneous Endoscopic Gastrostomy (PEG) Consult Workflow
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Emily Gore, MD
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Emily Gore, MD, Edward Cytryn, MD, Emily Leven, MD, Alyssa Chen, MD, Peter Beah, MD, Allison Glasser, MBA, Sean El Haj, BS, Christopher Cao, MD, David Greenwald, MD, FACG
Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Percutaneous endoscopic gastrostomy (PEG) is used to establish long-term enteral feeding in specific circumstances. Appropriate placement requires collaboration among gastroenterology (GI), speech-language pathology, nutrition, and primary teams. Structured assessment tools may facilitate timely and appropriate PEG placement.
Methods: An electronic medical record checklist was developed and integrated into the GI consult workflow (Figure 1) at a large tertiary academic medical center to ensure patients were optimized prior to GI consult for PEG placement. The checklist (Figure 2) included PEG indications, relative contraindications, antiplatelet/anticoagulant use, clinical stability, and consent/alignment with patient goals. Primary teams were informed of the initiative via email and biweekly internal medicine (IM) resident meetings; GI fellows delivered several educational sessions on enteral feeding to residents. Data were collected on pre-procedural factors, demographics, and time from GI consult to PEG placement. Provider impressions were assessed with pre- and post-intervention surveys.
Results: From 12/2024 to 5/2025, the PEG checklist was completed for 73 patients (mean age 70.2 years, range 29-99) – 36 (49.3%) were optimized on initial GI consult per checklist criteria; 49 (67.1%) ultimately received a PEG. PEG indications included nutritional support (52.1%), neurologic dysphagia (41.1%), pulmonary aspiration risk (27.4%), and mechanical obstruction (5.5%). 60.3% of patients were on anticoagulation or antiplatelet agents. Checklist use significantly reduced the average time from GI consult to PEG placement (3.65 vs. 1.95 weekdays; p=0.046). Pre-intervention surveys of 52 primary team providers (31 IM residents, 21 IM or Critical Care advanced practice providers) indicated limited familiarity with PEG indications (55.8%) and contraindications (36.5%), with 59.6% uncomfortable preparing patients for the procedure. Post-intervention surveys (n=30) showed most providers found the checklist easy to use (90%), efficient (73.3%), and helpful in determining when to call a GI consult (73.3%).
Discussion: A standardized pre-procedural checklist improved transparency in the PEG evaluation process, enhanced primary team knowledge, and streamlined communication between primary teams and GI consultants. The checklist was associated with significantly shorter times between GI consult and PEG placement, reducing a potential source of procedural delays.
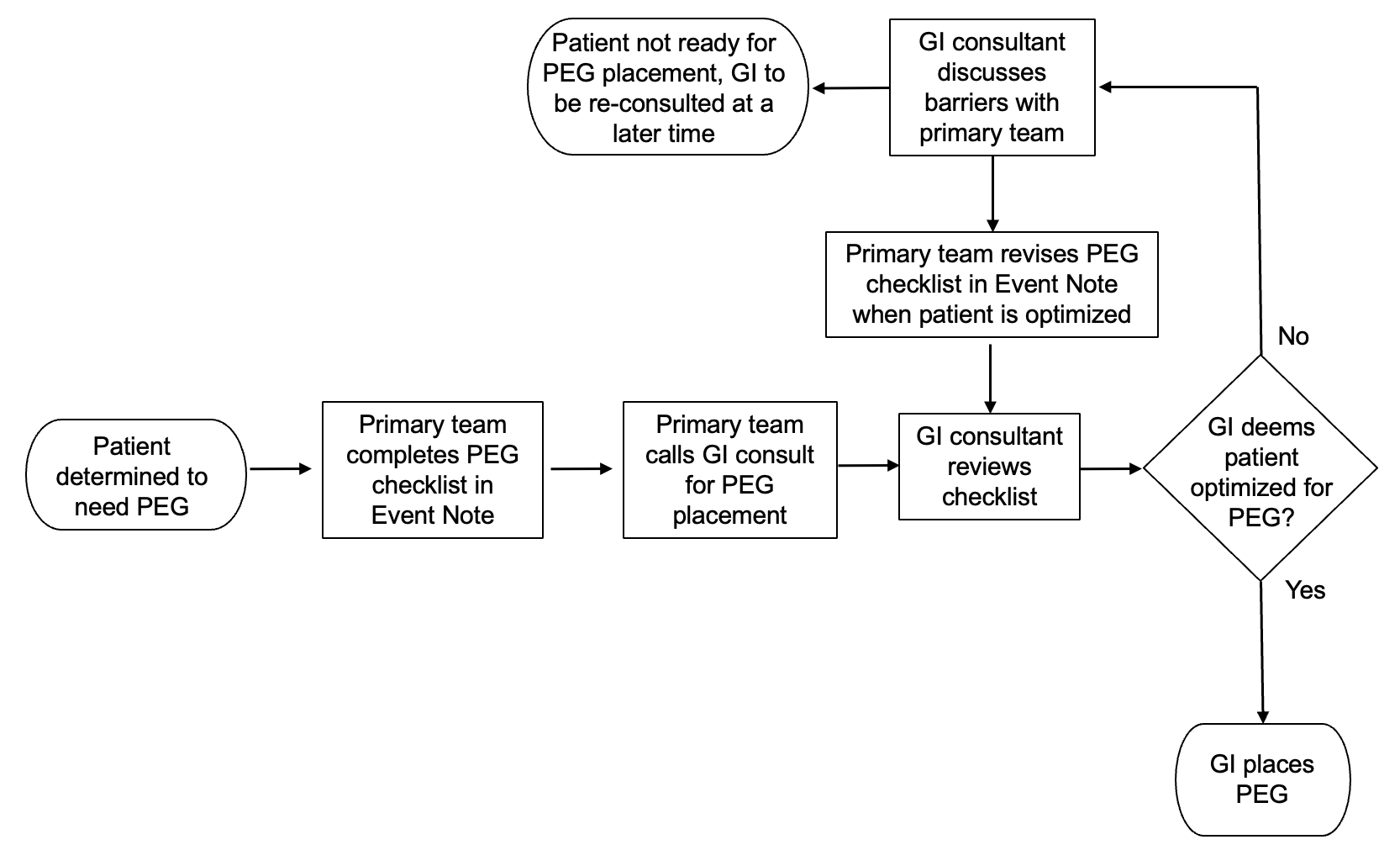
Figure: PEG consult workflow
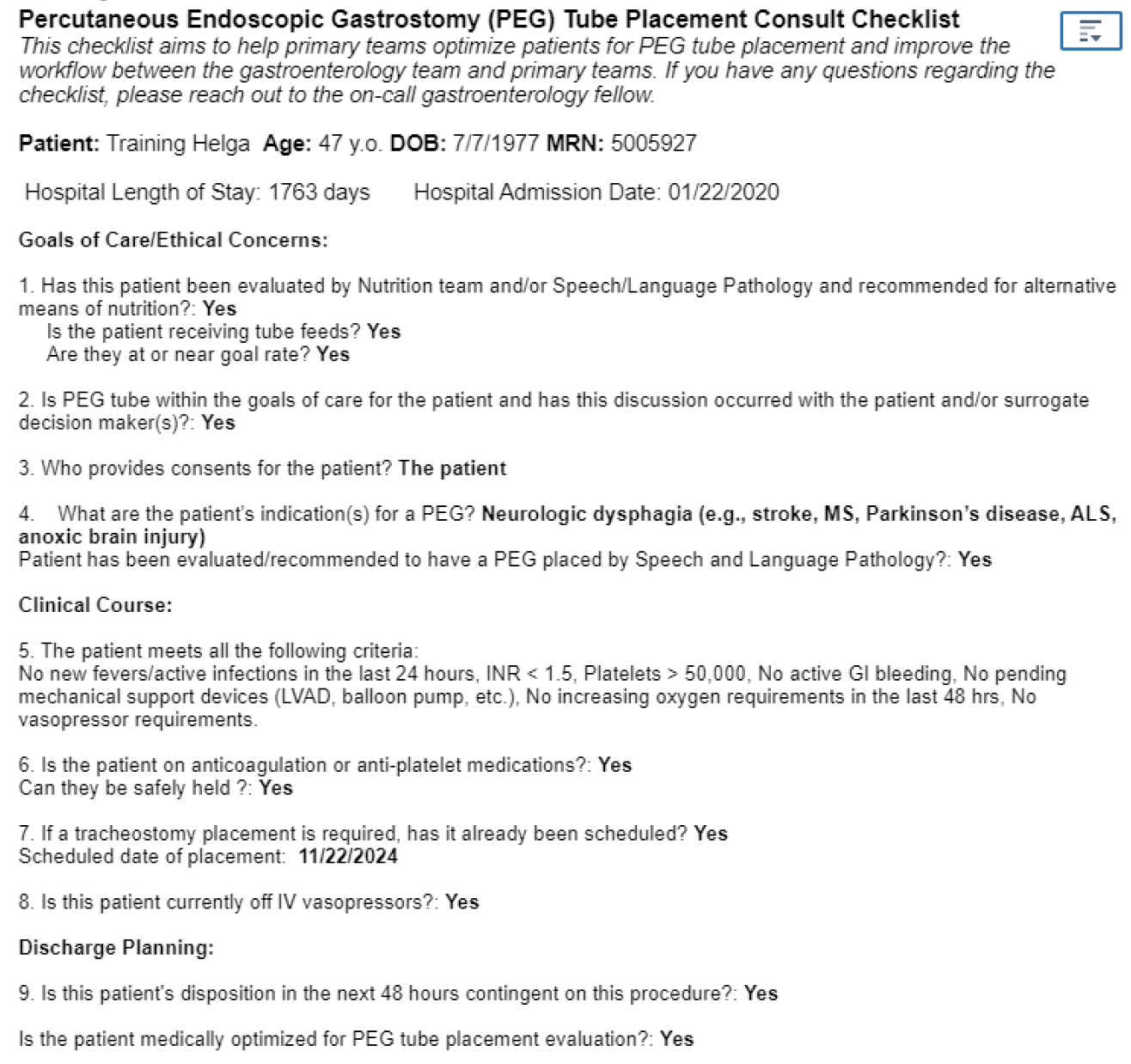
Figure: Sample completed PEG checklist
Disclosures:
Emily Gore indicated no relevant financial relationships.
Edward Cytryn indicated no relevant financial relationships.
Emily Leven indicated no relevant financial relationships.
Alyssa Chen indicated no relevant financial relationships.
Peter Beah indicated no relevant financial relationships.
Allison Glasser indicated no relevant financial relationships.
Sean El Haj indicated no relevant financial relationships.
Christopher Cao indicated no relevant financial relationships.
David Greenwald indicated no relevant financial relationships.
Emily Gore, MD, Edward Cytryn, MD, Emily Leven, MD, Alyssa Chen, MD, Peter Beah, MD, Allison Glasser, MBA, Sean El Haj, BS, Christopher Cao, MD, David Greenwald, MD, FACG. P6164 - Use of a Pre-Procedural Checklist to Improve Percutaneous Endoscopic Gastrostomy (PEG) Consult Workflow, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Percutaneous endoscopic gastrostomy (PEG) is used to establish long-term enteral feeding in specific circumstances. Appropriate placement requires collaboration among gastroenterology (GI), speech-language pathology, nutrition, and primary teams. Structured assessment tools may facilitate timely and appropriate PEG placement.
Methods: An electronic medical record checklist was developed and integrated into the GI consult workflow (Figure 1) at a large tertiary academic medical center to ensure patients were optimized prior to GI consult for PEG placement. The checklist (Figure 2) included PEG indications, relative contraindications, antiplatelet/anticoagulant use, clinical stability, and consent/alignment with patient goals. Primary teams were informed of the initiative via email and biweekly internal medicine (IM) resident meetings; GI fellows delivered several educational sessions on enteral feeding to residents. Data were collected on pre-procedural factors, demographics, and time from GI consult to PEG placement. Provider impressions were assessed with pre- and post-intervention surveys.
Results: From 12/2024 to 5/2025, the PEG checklist was completed for 73 patients (mean age 70.2 years, range 29-99) – 36 (49.3%) were optimized on initial GI consult per checklist criteria; 49 (67.1%) ultimately received a PEG. PEG indications included nutritional support (52.1%), neurologic dysphagia (41.1%), pulmonary aspiration risk (27.4%), and mechanical obstruction (5.5%). 60.3% of patients were on anticoagulation or antiplatelet agents. Checklist use significantly reduced the average time from GI consult to PEG placement (3.65 vs. 1.95 weekdays; p=0.046). Pre-intervention surveys of 52 primary team providers (31 IM residents, 21 IM or Critical Care advanced practice providers) indicated limited familiarity with PEG indications (55.8%) and contraindications (36.5%), with 59.6% uncomfortable preparing patients for the procedure. Post-intervention surveys (n=30) showed most providers found the checklist easy to use (90%), efficient (73.3%), and helpful in determining when to call a GI consult (73.3%).
Discussion: A standardized pre-procedural checklist improved transparency in the PEG evaluation process, enhanced primary team knowledge, and streamlined communication between primary teams and GI consultants. The checklist was associated with significantly shorter times between GI consult and PEG placement, reducing a potential source of procedural delays.
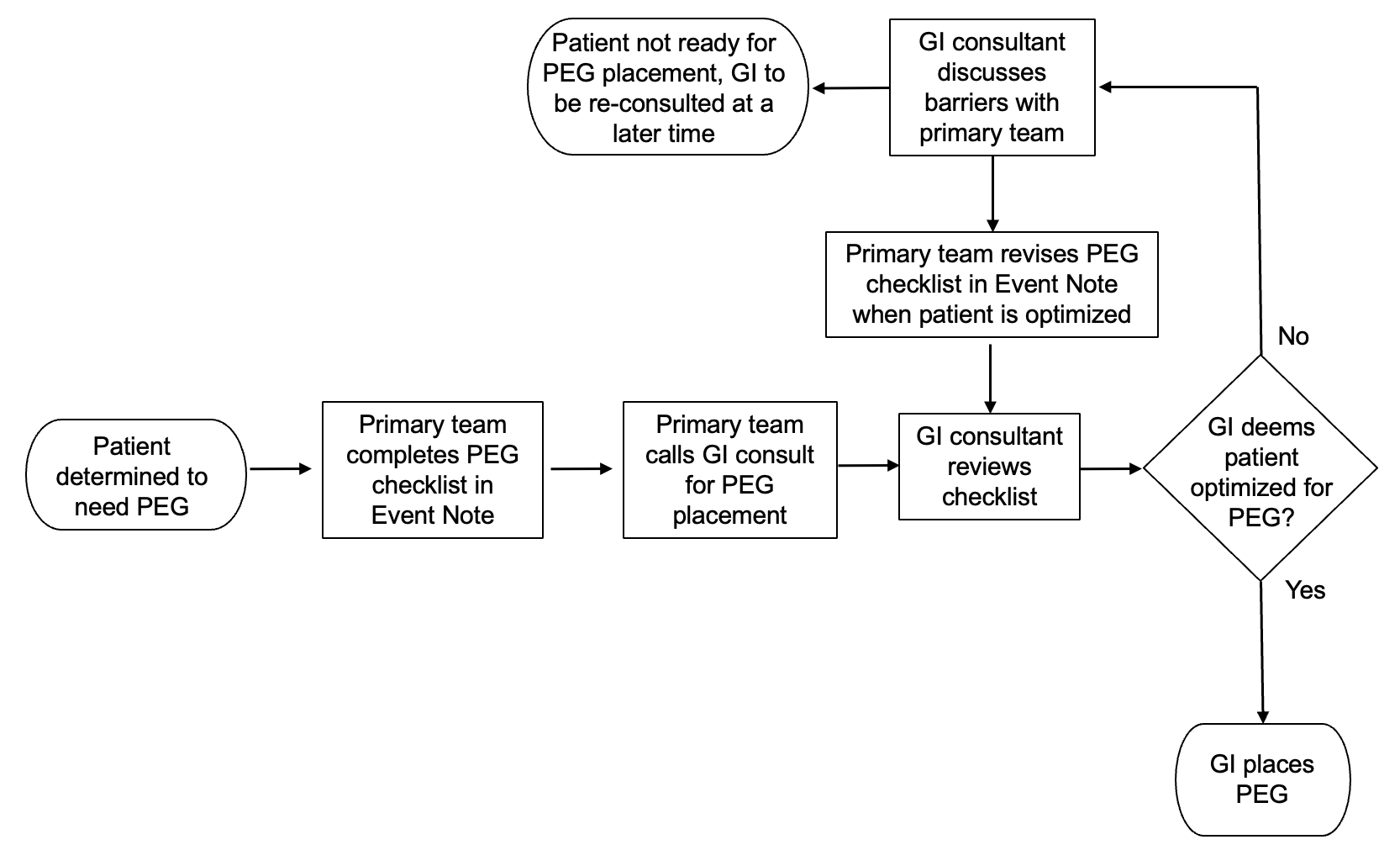
Figure: PEG consult workflow
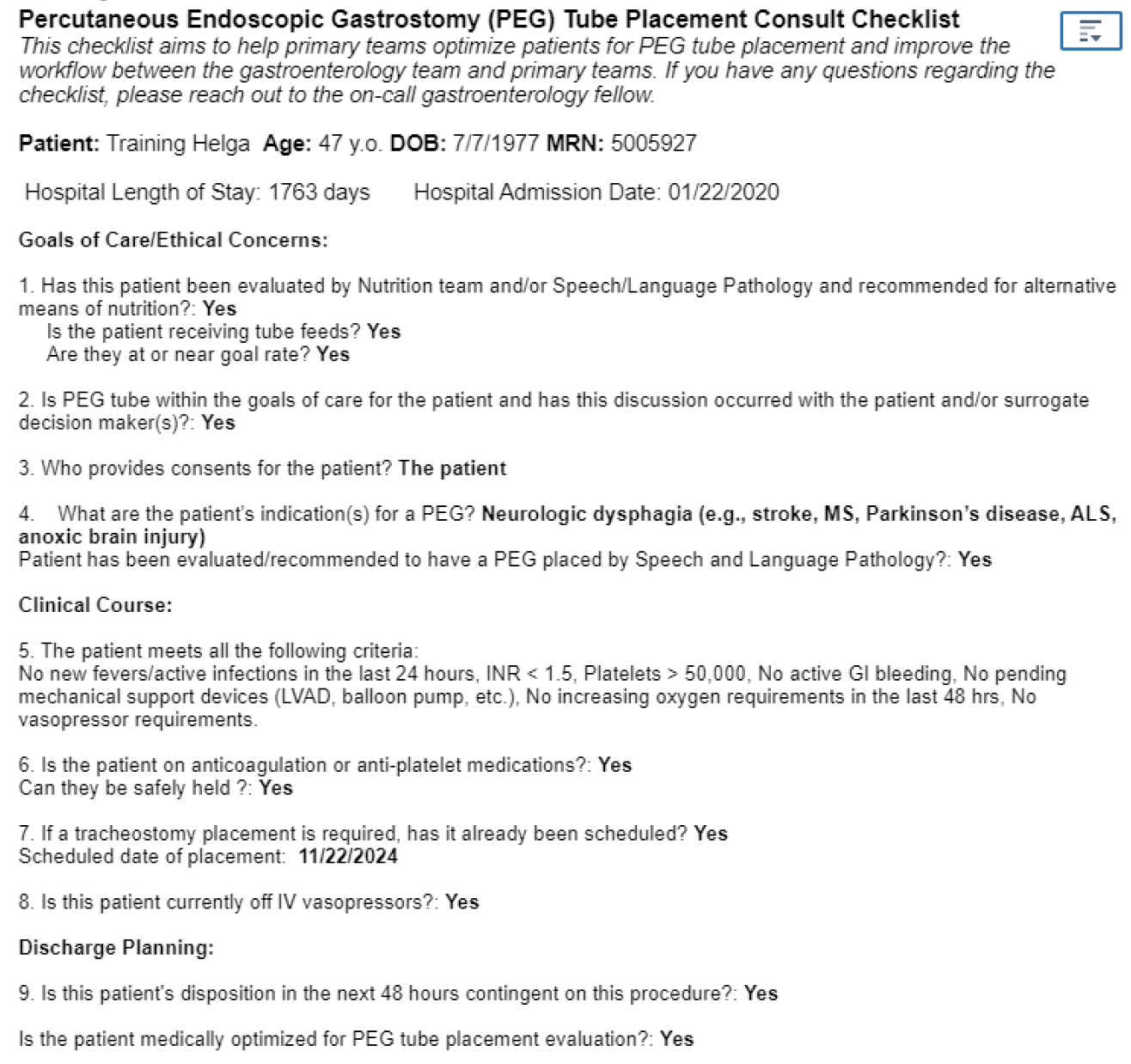
Figure: Sample completed PEG checklist
Disclosures:
Emily Gore indicated no relevant financial relationships.
Edward Cytryn indicated no relevant financial relationships.
Emily Leven indicated no relevant financial relationships.
Alyssa Chen indicated no relevant financial relationships.
Peter Beah indicated no relevant financial relationships.
Allison Glasser indicated no relevant financial relationships.
Sean El Haj indicated no relevant financial relationships.
Christopher Cao indicated no relevant financial relationships.
David Greenwald indicated no relevant financial relationships.
Emily Gore, MD, Edward Cytryn, MD, Emily Leven, MD, Alyssa Chen, MD, Peter Beah, MD, Allison Glasser, MBA, Sean El Haj, BS, Christopher Cao, MD, David Greenwald, MD, FACG. P6164 - Use of a Pre-Procedural Checklist to Improve Percutaneous Endoscopic Gastrostomy (PEG) Consult Workflow, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

