Tuesday Poster Session
Category: Small Intestine
P6284 - ARBs and Enteric Inflammation: Losartan-Induced Ileitis With Resolution on Telmisartan Reveals Intra-Class Heterogeneity
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Karan Sachdeva, MBBS, MPH
SUNY Upstate Medical University
Syracuse, NY
Presenting Author(s)
Karan Sachdeva, MBBS, MPH, Avleen Kaur, MD, Kelita Singh, MD
SUNY Upstate Medical University, Syracuse, NY
Introduction: Isolated terminal ileitis poses a diagnostic dilemma, especially in cases where it is incidentally found. Potential etiologies of ileitis include, but are not limited to Crohn’s disease, intestinal tuberculosis, malignancy, sarcoidosis, eosinophilic/lymphocytic ileitis and chronic NSAID use. A rare cause of ileitis is angiotensin receptor blockers (ARBs), but little is known about specific medications. We present a rare case of losartan-induced terminal ileitis that interestingly resolved after an in-class switch to telmisartan.
Case Description/
Methods: A 75 year old male with a history of heart failure, GERD underwent computed tomography (CT) for follow-up of gastrointestinal stromal tumor (GIST) that demonstrated segmental wall thickening of the distal ileum. The patient was asymptomatic, however was anemic with a hemoglobin of 10.5 g/dl. Due to history of malignancy, age and anemia, patient underwent a colonoscopy which revealed circumferential thickening and infiltrative changes extending 10cm into the terminal ileum (Figure 1a). Biopsy from this segment showed chronic ileitis with ulceration and fibrinopurulent exudate. Patient had been on losartan for >5 years and otherwise did not have other potential culprit medication history. He was subsequently switched to telmisartan (due to other comorbidities) and given asymptomatic status underwent colonoscopy 8 months later, which showed mildly erythematous mucosa, but overall improved appearance with multiple biopsies showing no ileitis (Figure 1b). He remains asymptomatic, and anemia improved to average of 12 g/dl.
Discussion: Olmesartan has previously demonstrated association with isolated terminal ileitis, but data is lacking regarding other ARBs. This is a novel case of terminal ileitis on losartan that surprisingly resolved after switching to telmisartan, highlighting that individual medications within the ARB class may confer varying risk. The case demonstrates that clinicians should consider ARB-induced ileitis in patients on ARBs who present with signs/symptoms of luminal gastrointestinal inflammation and consider switching the patient’s medications to a non-ARB antihypertensive vs. a different ARB (where it is a medication of choice due to comorbidities). Given the paucity of data, caution is recommended if switching within the ARB class and close follow-up with labwork and repeat endoscopy and biopsies is recommended to reassess response to change in therapy.
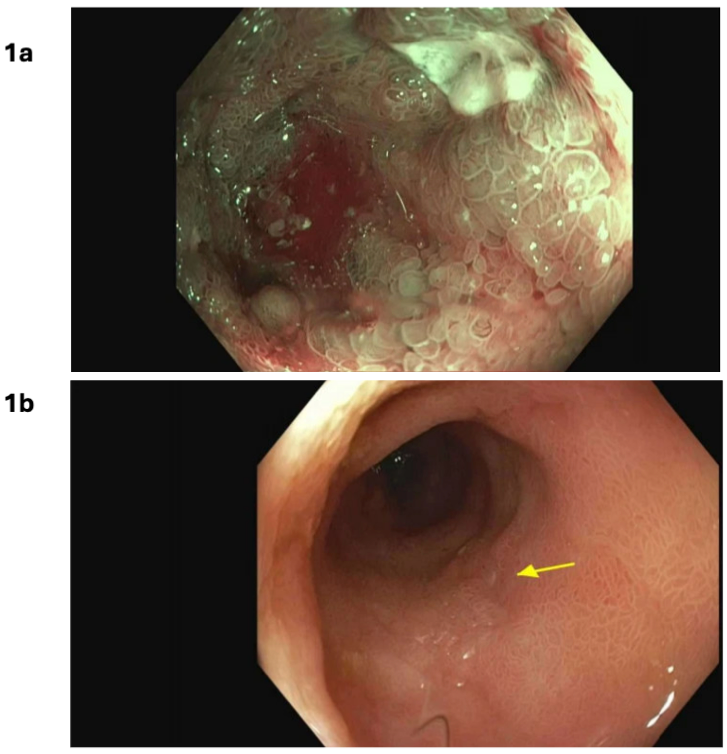
Figure: Figure 1a: Initial colonoscopy (on losartan) after CT scan showing ileal thickening; 1b. Follow up colonoscopy 8 months (on telmisartan) after CT scan showing ileal thickening
Disclosures:
Karan Sachdeva indicated no relevant financial relationships.
Avleen Kaur indicated no relevant financial relationships.
Kelita Singh indicated no relevant financial relationships.
Karan Sachdeva, MBBS, MPH, Avleen Kaur, MD, Kelita Singh, MD. P6284 - ARBs and Enteric Inflammation: Losartan-Induced Ileitis With Resolution on Telmisartan Reveals Intra-Class Heterogeneity, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
SUNY Upstate Medical University, Syracuse, NY
Introduction: Isolated terminal ileitis poses a diagnostic dilemma, especially in cases where it is incidentally found. Potential etiologies of ileitis include, but are not limited to Crohn’s disease, intestinal tuberculosis, malignancy, sarcoidosis, eosinophilic/lymphocytic ileitis and chronic NSAID use. A rare cause of ileitis is angiotensin receptor blockers (ARBs), but little is known about specific medications. We present a rare case of losartan-induced terminal ileitis that interestingly resolved after an in-class switch to telmisartan.
Case Description/
Methods: A 75 year old male with a history of heart failure, GERD underwent computed tomography (CT) for follow-up of gastrointestinal stromal tumor (GIST) that demonstrated segmental wall thickening of the distal ileum. The patient was asymptomatic, however was anemic with a hemoglobin of 10.5 g/dl. Due to history of malignancy, age and anemia, patient underwent a colonoscopy which revealed circumferential thickening and infiltrative changes extending 10cm into the terminal ileum (Figure 1a). Biopsy from this segment showed chronic ileitis with ulceration and fibrinopurulent exudate. Patient had been on losartan for >5 years and otherwise did not have other potential culprit medication history. He was subsequently switched to telmisartan (due to other comorbidities) and given asymptomatic status underwent colonoscopy 8 months later, which showed mildly erythematous mucosa, but overall improved appearance with multiple biopsies showing no ileitis (Figure 1b). He remains asymptomatic, and anemia improved to average of 12 g/dl.
Discussion: Olmesartan has previously demonstrated association with isolated terminal ileitis, but data is lacking regarding other ARBs. This is a novel case of terminal ileitis on losartan that surprisingly resolved after switching to telmisartan, highlighting that individual medications within the ARB class may confer varying risk. The case demonstrates that clinicians should consider ARB-induced ileitis in patients on ARBs who present with signs/symptoms of luminal gastrointestinal inflammation and consider switching the patient’s medications to a non-ARB antihypertensive vs. a different ARB (where it is a medication of choice due to comorbidities). Given the paucity of data, caution is recommended if switching within the ARB class and close follow-up with labwork and repeat endoscopy and biopsies is recommended to reassess response to change in therapy.
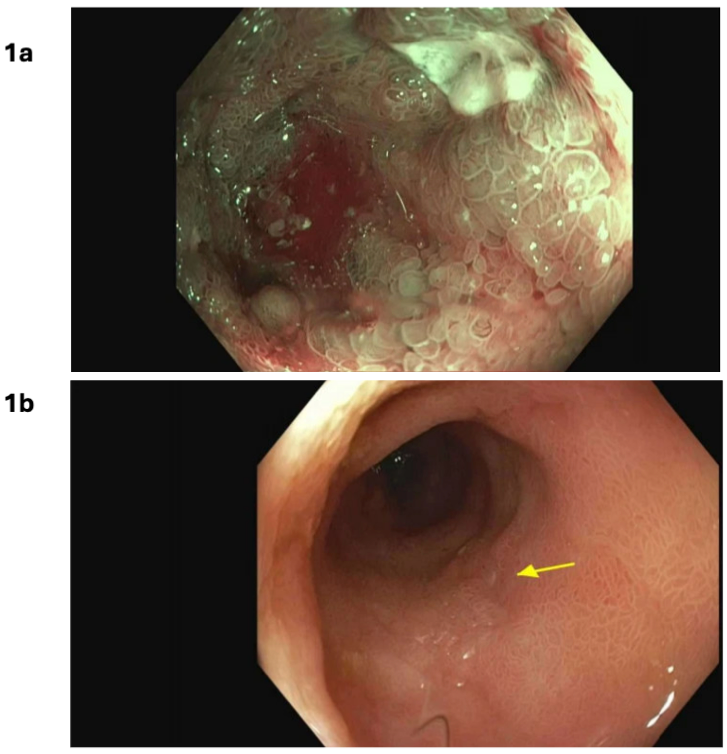
Figure: Figure 1a: Initial colonoscopy (on losartan) after CT scan showing ileal thickening; 1b. Follow up colonoscopy 8 months (on telmisartan) after CT scan showing ileal thickening
Disclosures:
Karan Sachdeva indicated no relevant financial relationships.
Avleen Kaur indicated no relevant financial relationships.
Kelita Singh indicated no relevant financial relationships.
Karan Sachdeva, MBBS, MPH, Avleen Kaur, MD, Kelita Singh, MD. P6284 - ARBs and Enteric Inflammation: Losartan-Induced Ileitis With Resolution on Telmisartan Reveals Intra-Class Heterogeneity, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
