Tuesday Poster Session
Category: Small Intestine
P6281 - Treatment Failure for Recurrent Venous Thromboembolism in a Patient With Celiac Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jade Pace, MD (she/her/hers)
North Shore University Hospital - Northwell Health
Manhasset, NY
Presenting Author(s)
Jade Pace, MD1, Christopher Dorizas, MD2, Kishan Patel, MD3
1North Shore University Hospital - Northwell Health, Manhasset, NY; 2North Shore University Hospital/Zucker School of Medicine at Hofstra University, Garden City, NY; 3Long Island Jewish Medical Center - Northwell Health, Queens, NY
Introduction: Venous thromboembolism (VTE) is a rare and conflicting extra-intestinal manifestation of celiac disease. The mechanism is likely multifactorial including deficiencies due to malabsorption, but the exact pathophysiology is unknown. Moreover, reported cases of recurrent VTE are scarce. We present a case of a young male with uncontrolled celiac disease who presented with recurrent deep vein thrombosis (DVT) despite anticoagulation.
Case Description/
Methods: A 27‐year‐old male with a history of alcohol use disorder, recurrent pancreatitis, and unprovoked DVT/pulmonary embolism two months prior presented to the ED for malaise, severe protein-calorie malnutrition with 30 lb weight loss, steatorrhea, and leg swelling. Patient had prior positive celiac serologies (transglutaminase IgG 14.7 and IgA > 100 U/mL) but was non-compliant with diet. However, he was compliant with Eliquis from his prior admission.
The patient’s vitals were stable. Physical exam was significant for bilateral lower extremity edema and rash. Labs showed profound hypoalbuminemia (1.5 g/dL), microcytic anemia (hemoglobin 6.2 g/dL), possible hemolysis (haptoglobin < 20 mg/dL, lactate dehydrogenase 407 U/L), and iron studies suggestive of iron deficiency. Doppler identified acute DVTs in the right peroneal (prior location) and posterior tibial (new) veins (Figure 1).
The hypercoagulability panel was negative, but the patient had nutritional deficiencies (Table 1). The severe protein loss secondary to uncontrolled celiac disease in conjunction with pancreatic insufficiency likely contributed to deficiencies in clotting regulatory proteins, predisposing the patient to thrombotic events. The patient’s anemia was thought to be mixed autoimmune hemolytic anemia and iron deficiency secondary to celiac disease. The rash was attributed to dermatitis herpetiformis. Management included heparin for the acute DVT, strict gluten-free diet, and nutritional supplementation. Factor Xa level was within range, ruling out failure due to malabsorption, and patient was continued on Eliquis outpatient.
Discussion: This case exemplifies the multifaceted complications that arise from uncontrolled celiac disease, particularly with gluten-free diet non-compliance. The relevance of this case is underscored in that although the VTE was treated on first admission, the underlying etiology was not. Given the increasing prevalence of celiac disease, clinicians must maintain a high index of suspicion for such atypical complications and emphasize dietary adherence.
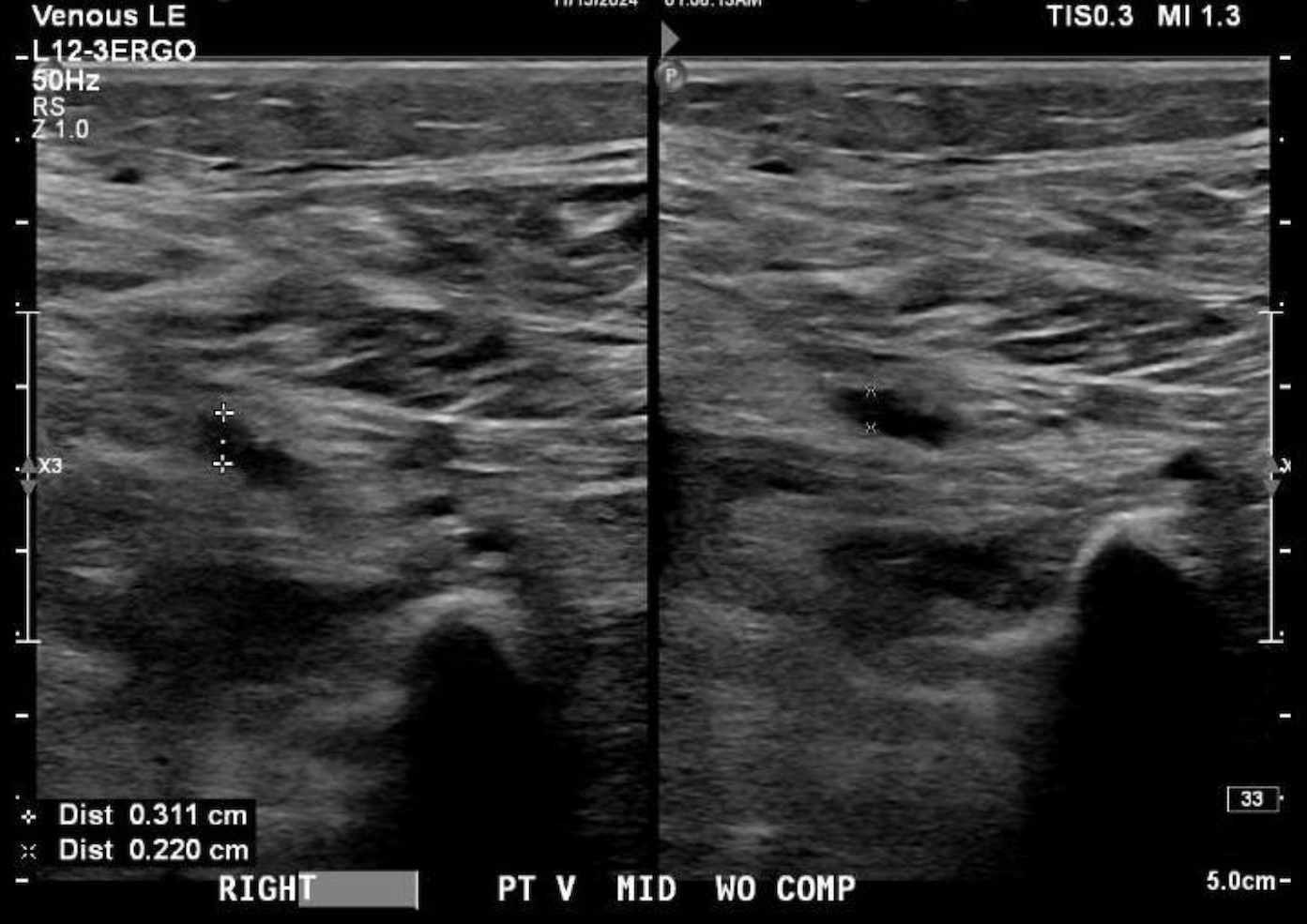
Figure: Figure 1. Right lower extremity duplex demonstrating a non-compressible posterior tibial vein.
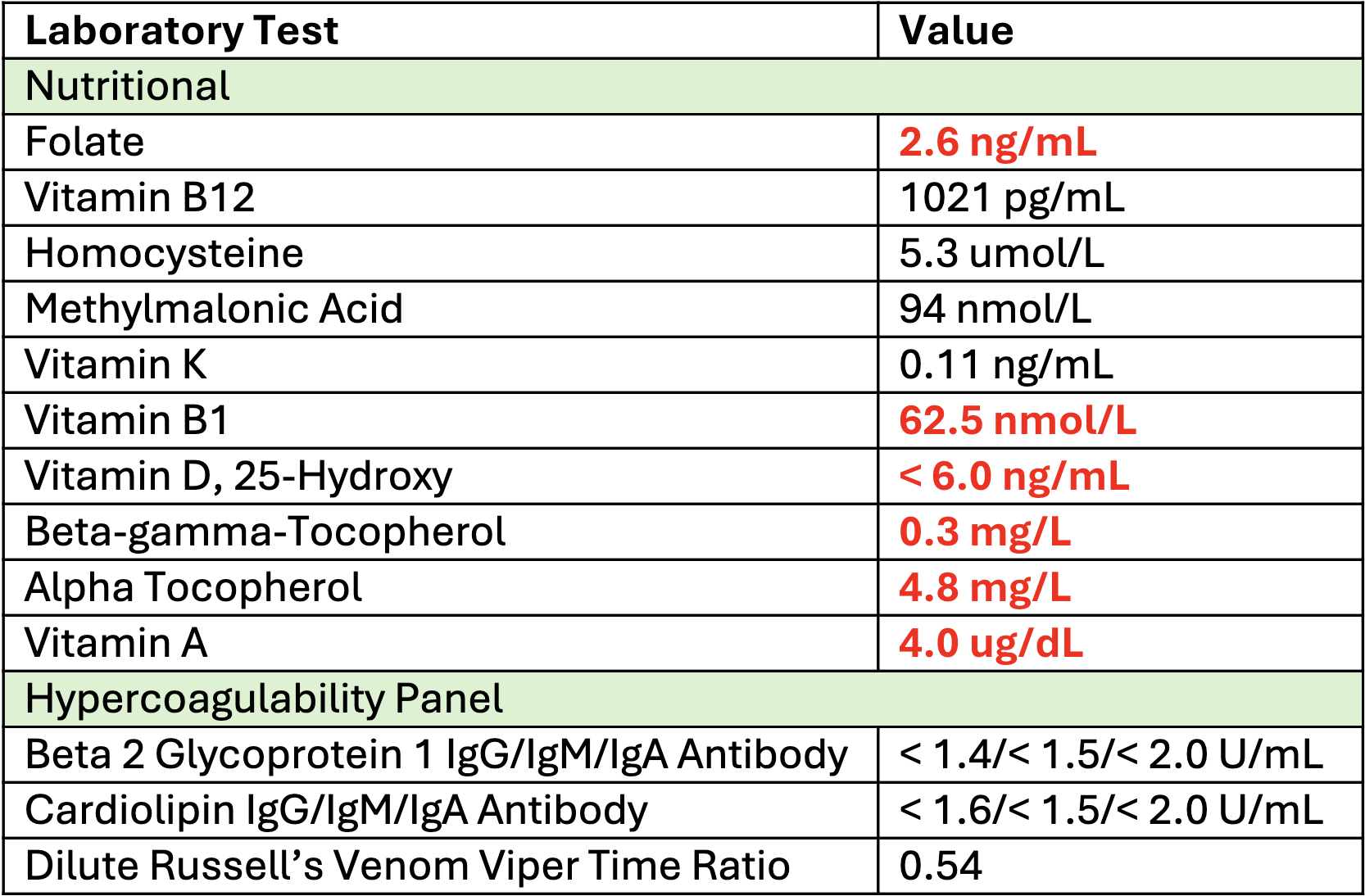
Figure: Table 1. Summary of nutritional and hypercoagulable workup. Abnormally low values indicated in red.
Disclosures:
Jade Pace indicated no relevant financial relationships.
Christopher Dorizas indicated no relevant financial relationships.
Kishan Patel indicated no relevant financial relationships.
Jade Pace, MD1, Christopher Dorizas, MD2, Kishan Patel, MD3. P6281 - Treatment Failure for Recurrent Venous Thromboembolism in a Patient With Celiac Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1North Shore University Hospital - Northwell Health, Manhasset, NY; 2North Shore University Hospital/Zucker School of Medicine at Hofstra University, Garden City, NY; 3Long Island Jewish Medical Center - Northwell Health, Queens, NY
Introduction: Venous thromboembolism (VTE) is a rare and conflicting extra-intestinal manifestation of celiac disease. The mechanism is likely multifactorial including deficiencies due to malabsorption, but the exact pathophysiology is unknown. Moreover, reported cases of recurrent VTE are scarce. We present a case of a young male with uncontrolled celiac disease who presented with recurrent deep vein thrombosis (DVT) despite anticoagulation.
Case Description/
Methods: A 27‐year‐old male with a history of alcohol use disorder, recurrent pancreatitis, and unprovoked DVT/pulmonary embolism two months prior presented to the ED for malaise, severe protein-calorie malnutrition with 30 lb weight loss, steatorrhea, and leg swelling. Patient had prior positive celiac serologies (transglutaminase IgG 14.7 and IgA > 100 U/mL) but was non-compliant with diet. However, he was compliant with Eliquis from his prior admission.
The patient’s vitals were stable. Physical exam was significant for bilateral lower extremity edema and rash. Labs showed profound hypoalbuminemia (1.5 g/dL), microcytic anemia (hemoglobin 6.2 g/dL), possible hemolysis (haptoglobin < 20 mg/dL, lactate dehydrogenase 407 U/L), and iron studies suggestive of iron deficiency. Doppler identified acute DVTs in the right peroneal (prior location) and posterior tibial (new) veins (Figure 1).
The hypercoagulability panel was negative, but the patient had nutritional deficiencies (Table 1). The severe protein loss secondary to uncontrolled celiac disease in conjunction with pancreatic insufficiency likely contributed to deficiencies in clotting regulatory proteins, predisposing the patient to thrombotic events. The patient’s anemia was thought to be mixed autoimmune hemolytic anemia and iron deficiency secondary to celiac disease. The rash was attributed to dermatitis herpetiformis. Management included heparin for the acute DVT, strict gluten-free diet, and nutritional supplementation. Factor Xa level was within range, ruling out failure due to malabsorption, and patient was continued on Eliquis outpatient.
Discussion: This case exemplifies the multifaceted complications that arise from uncontrolled celiac disease, particularly with gluten-free diet non-compliance. The relevance of this case is underscored in that although the VTE was treated on first admission, the underlying etiology was not. Given the increasing prevalence of celiac disease, clinicians must maintain a high index of suspicion for such atypical complications and emphasize dietary adherence.
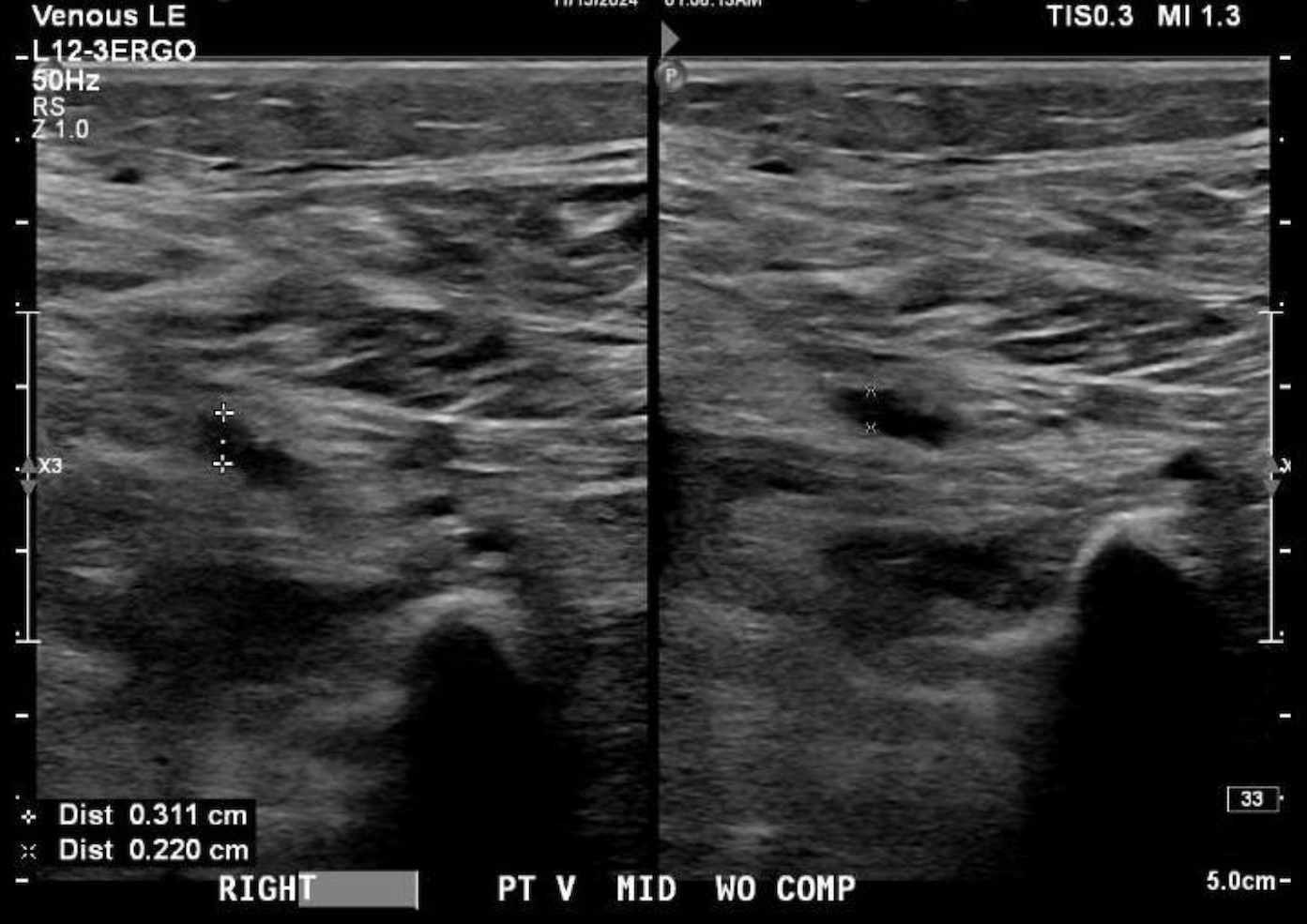
Figure: Figure 1. Right lower extremity duplex demonstrating a non-compressible posterior tibial vein.
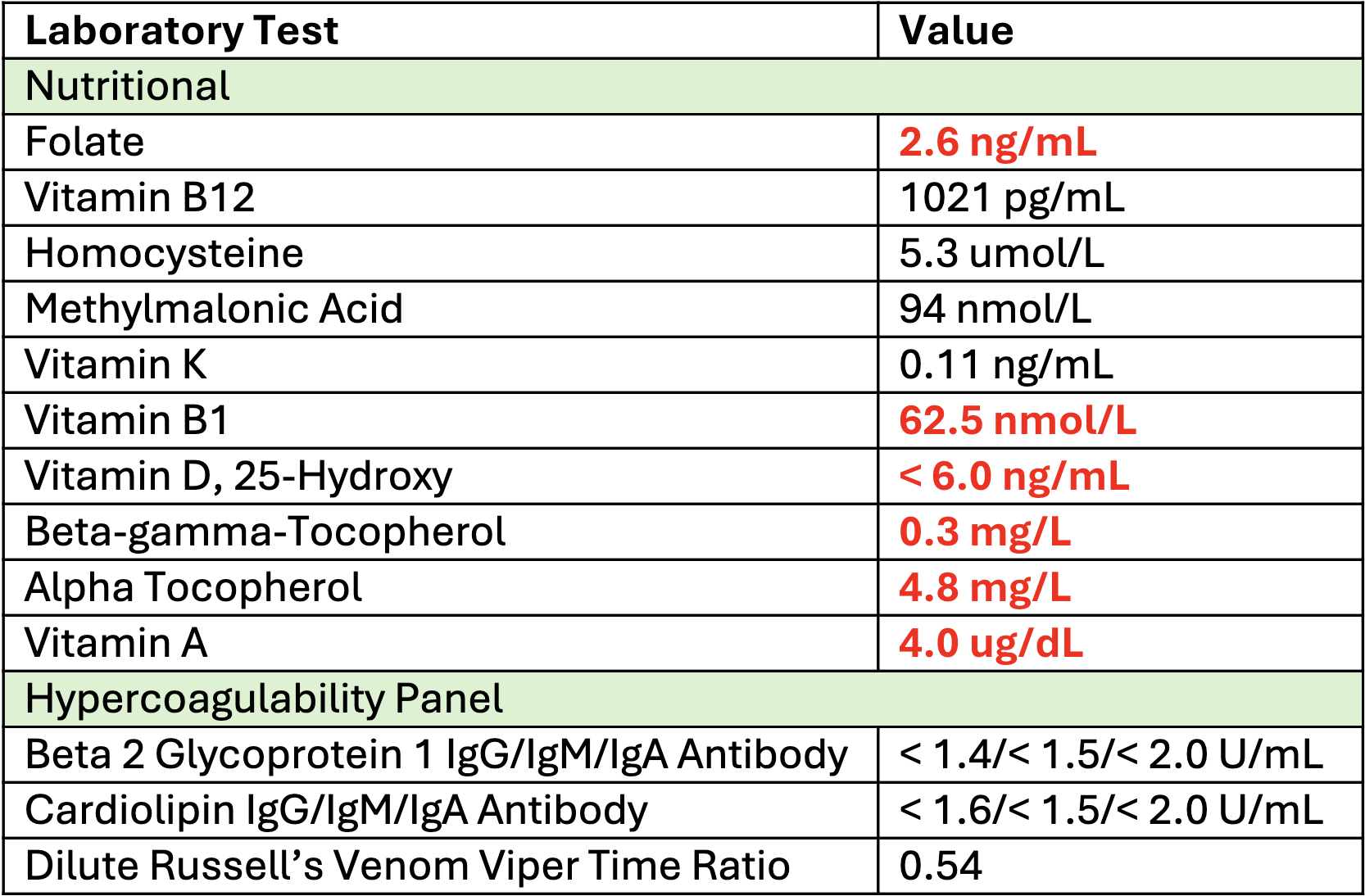
Figure: Table 1. Summary of nutritional and hypercoagulable workup. Abnormally low values indicated in red.
Disclosures:
Jade Pace indicated no relevant financial relationships.
Christopher Dorizas indicated no relevant financial relationships.
Kishan Patel indicated no relevant financial relationships.
Jade Pace, MD1, Christopher Dorizas, MD2, Kishan Patel, MD3. P6281 - Treatment Failure for Recurrent Venous Thromboembolism in a Patient With Celiac Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
