Tuesday Poster Session
Category: Stomach and Spleen
P6332 - Trends of Recent Years With Future Forecasting of Peptic Ulcer Mortality in the United States (1999-2035)
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Amine Rakab, MD (he/him/his)
Division of Medical Education, Weill Cornell Medicine
Doha, Ad Dawhah, Qatar
Presenting Author(s)
Muhammad Umar, MD1, Syeda Simrah Shah, MD2, Amna Anwar, MD3, Bisher Sawaf, MD4, Amin Abu Hejleh, MD5, Anchit Chauhan, 6, Amine Rakab, MD7, Ayesha Hidayat, MD8
1Khairpur Medical College, Khairpur Mirs, Islamabad, Islamabad, Pakistan; 2Dow Medical College, Islamabad, Islamabad, Pakistan; 3federal medical and dental college Islamabad, Islamabad, Islamabad, Pakistan; 4University of Toledo Medical Center, Toledo, OH; 5Mohammed Bin Rashid University of Medicine and Health Sciences, Dubai, Dubai, United Arab Emirates; 6Maulana Azad Medical College, New Delhi, Delhi, India; 7Division of Medical Education, Weill Cornell Medicine, Doha, Ad Dawhah, Qatar; 8peoples university of medical and health sciences, Islamabad, Islamabad, Pakistan
Introduction: Peptic ulcer disease (PUD) remains a notable health concern in the U.S., with shifting mortality trends across regions and demographics. Despite treatment advances, ongoing surveillance and targeted interventions are essential.
Methods: Data from the Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) were analyzed for peptic ulcer disease ICD-10 codes K25-K26) in adults aged over 25 years from 1999 to 2023. Age-adjusted mortality trends were assessed using Joinpoint regression, and future rates were forecasted using an optimal Autoregressive Integrated Moving Average (ARIMA) model.
Results: From 1999–2023, peptic ulcer disease (PUD) caused 116,669 deaths in the U.S., with age-adjusted mortality rates (AAMRs) declining from 3.2 to 2.18 per million (AAPC: –1.68%; p = –0.76). Forecasts using an ARIMA model showed a slower decline (AAPC: –0.18%; p = 0.06), with rates rising from –0.475 in 2024 to 0.015 by 2035. Age-specific analysis was limited due to unreliable data.
Male AAMRs declined from 4.1 to 2.69 (AAPC: –1.65%; p = 0.00) and female from 2.61 to 1.77 (AAPC: –1.76%; p = 0.01). All races showed declining AAMRs except American Indian/Alaska Native, which rose from 1.89 to 2.22 (AAPC: –3.00%; p = 0.66). White and Black populations saw declines, with Whites showing the highest increase in APC (–6.76% to 3.26%).
All U.S. regions had declining AAMRs: Northeast (2.76–1.72), Midwest (3.32–2.21), South (2.94–2.00), and West (4.1–2.82), with the Northeast showing the largest APC increase. In 2020, AAMRs were higher in non-metropolitan areas (4.9) than in metropolitan areas (3.9).
States with the highest mortality included California, D.C., Oregon, and others; Massachusetts had the lowest. Most deaths occurred in inpatient facilities (66,877), followed by homes (13,053).
Discussion: From 1999–2023, PUD mortality trends varied across groups, with notable increases among males, American Indians, and those in the Northeast. Deaths rose in both urban and rural areas, especially in the Northeast and Midwest. Most occurred in inpatient settings, underscoring the need for improved access and targeted interventions to reduce mortality in high-risk groups.
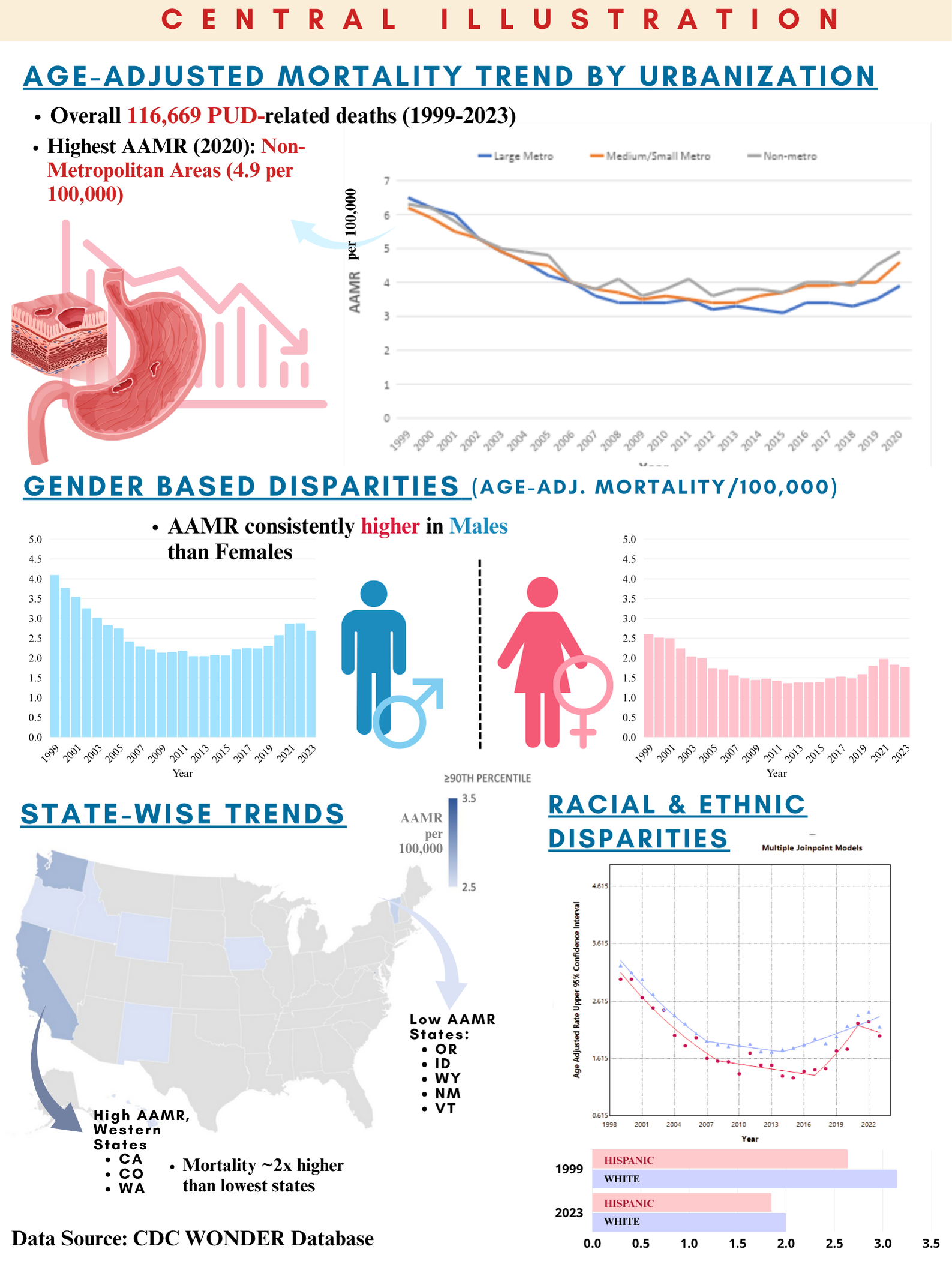
Figure: Figure1. Age-Adjusted Mortality Rate (AAMR) Trends and ARIMA Forecast of Mortality, 1999–2023
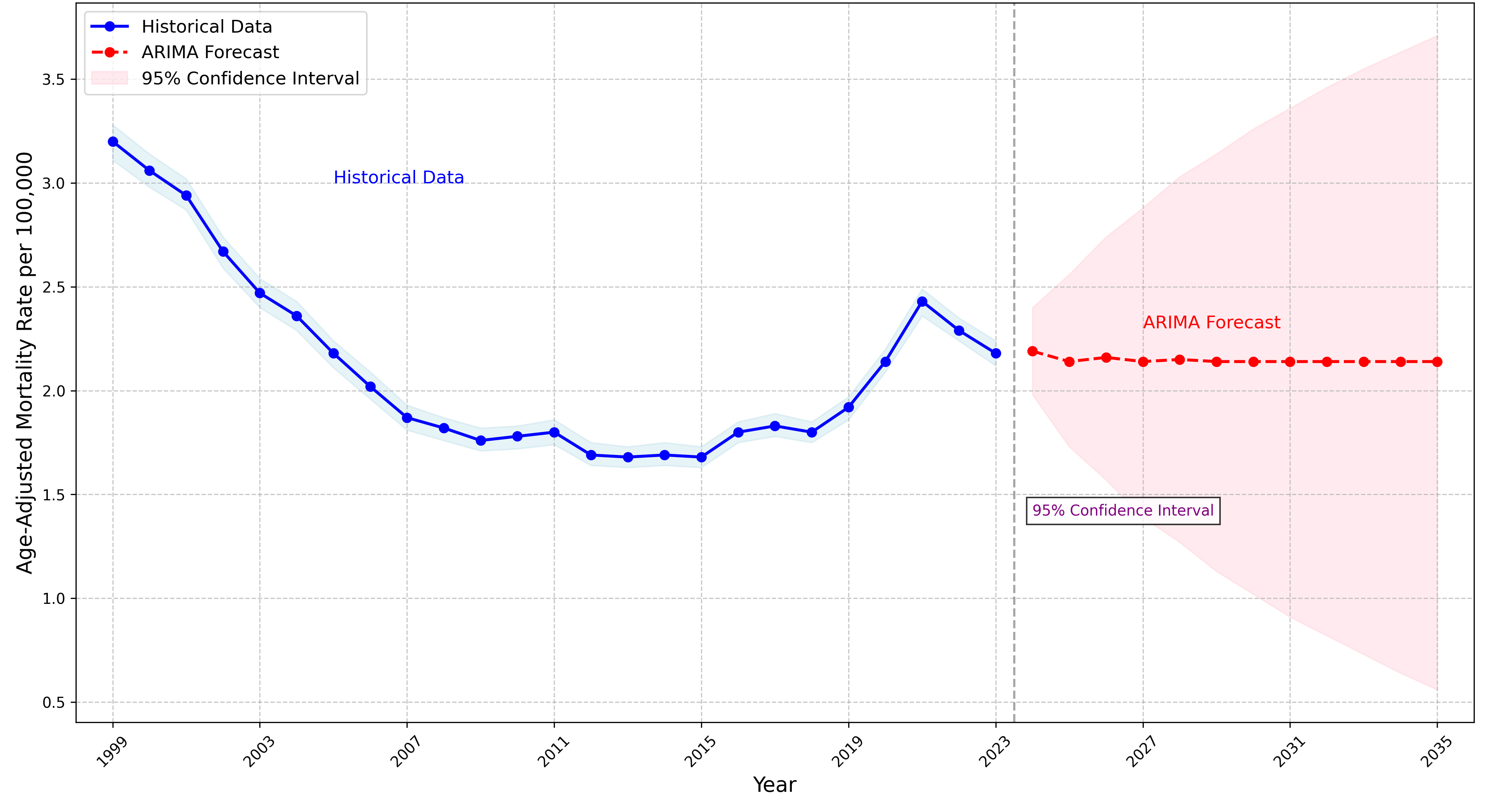
Figure: Figure 2. Changing Landscape of Peptic Ulcer Disease Mortality in the United States, 1999–2023
Disclosures:
Muhammad Umar indicated no relevant financial relationships.
Syeda Simrah Shah indicated no relevant financial relationships.
Amna Anwar indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Amin Abu Hejleh indicated no relevant financial relationships.
Anchit Chauhan indicated no relevant financial relationships.
Amine Rakab indicated no relevant financial relationships.
Ayesha Hidayat indicated no relevant financial relationships.
Muhammad Umar, MD1, Syeda Simrah Shah, MD2, Amna Anwar, MD3, Bisher Sawaf, MD4, Amin Abu Hejleh, MD5, Anchit Chauhan, 6, Amine Rakab, MD7, Ayesha Hidayat, MD8. P6332 - Trends of Recent Years With Future Forecasting of Peptic Ulcer Mortality in the United States (1999-2035), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Khairpur Medical College, Khairpur Mirs, Islamabad, Islamabad, Pakistan; 2Dow Medical College, Islamabad, Islamabad, Pakistan; 3federal medical and dental college Islamabad, Islamabad, Islamabad, Pakistan; 4University of Toledo Medical Center, Toledo, OH; 5Mohammed Bin Rashid University of Medicine and Health Sciences, Dubai, Dubai, United Arab Emirates; 6Maulana Azad Medical College, New Delhi, Delhi, India; 7Division of Medical Education, Weill Cornell Medicine, Doha, Ad Dawhah, Qatar; 8peoples university of medical and health sciences, Islamabad, Islamabad, Pakistan
Introduction: Peptic ulcer disease (PUD) remains a notable health concern in the U.S., with shifting mortality trends across regions and demographics. Despite treatment advances, ongoing surveillance and targeted interventions are essential.
Methods: Data from the Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) were analyzed for peptic ulcer disease ICD-10 codes K25-K26) in adults aged over 25 years from 1999 to 2023. Age-adjusted mortality trends were assessed using Joinpoint regression, and future rates were forecasted using an optimal Autoregressive Integrated Moving Average (ARIMA) model.
Results: From 1999–2023, peptic ulcer disease (PUD) caused 116,669 deaths in the U.S., with age-adjusted mortality rates (AAMRs) declining from 3.2 to 2.18 per million (AAPC: –1.68%; p = –0.76). Forecasts using an ARIMA model showed a slower decline (AAPC: –0.18%; p = 0.06), with rates rising from –0.475 in 2024 to 0.015 by 2035. Age-specific analysis was limited due to unreliable data.
Male AAMRs declined from 4.1 to 2.69 (AAPC: –1.65%; p = 0.00) and female from 2.61 to 1.77 (AAPC: –1.76%; p = 0.01). All races showed declining AAMRs except American Indian/Alaska Native, which rose from 1.89 to 2.22 (AAPC: –3.00%; p = 0.66). White and Black populations saw declines, with Whites showing the highest increase in APC (–6.76% to 3.26%).
All U.S. regions had declining AAMRs: Northeast (2.76–1.72), Midwest (3.32–2.21), South (2.94–2.00), and West (4.1–2.82), with the Northeast showing the largest APC increase. In 2020, AAMRs were higher in non-metropolitan areas (4.9) than in metropolitan areas (3.9).
States with the highest mortality included California, D.C., Oregon, and others; Massachusetts had the lowest. Most deaths occurred in inpatient facilities (66,877), followed by homes (13,053).
Discussion: From 1999–2023, PUD mortality trends varied across groups, with notable increases among males, American Indians, and those in the Northeast. Deaths rose in both urban and rural areas, especially in the Northeast and Midwest. Most occurred in inpatient settings, underscoring the need for improved access and targeted interventions to reduce mortality in high-risk groups.
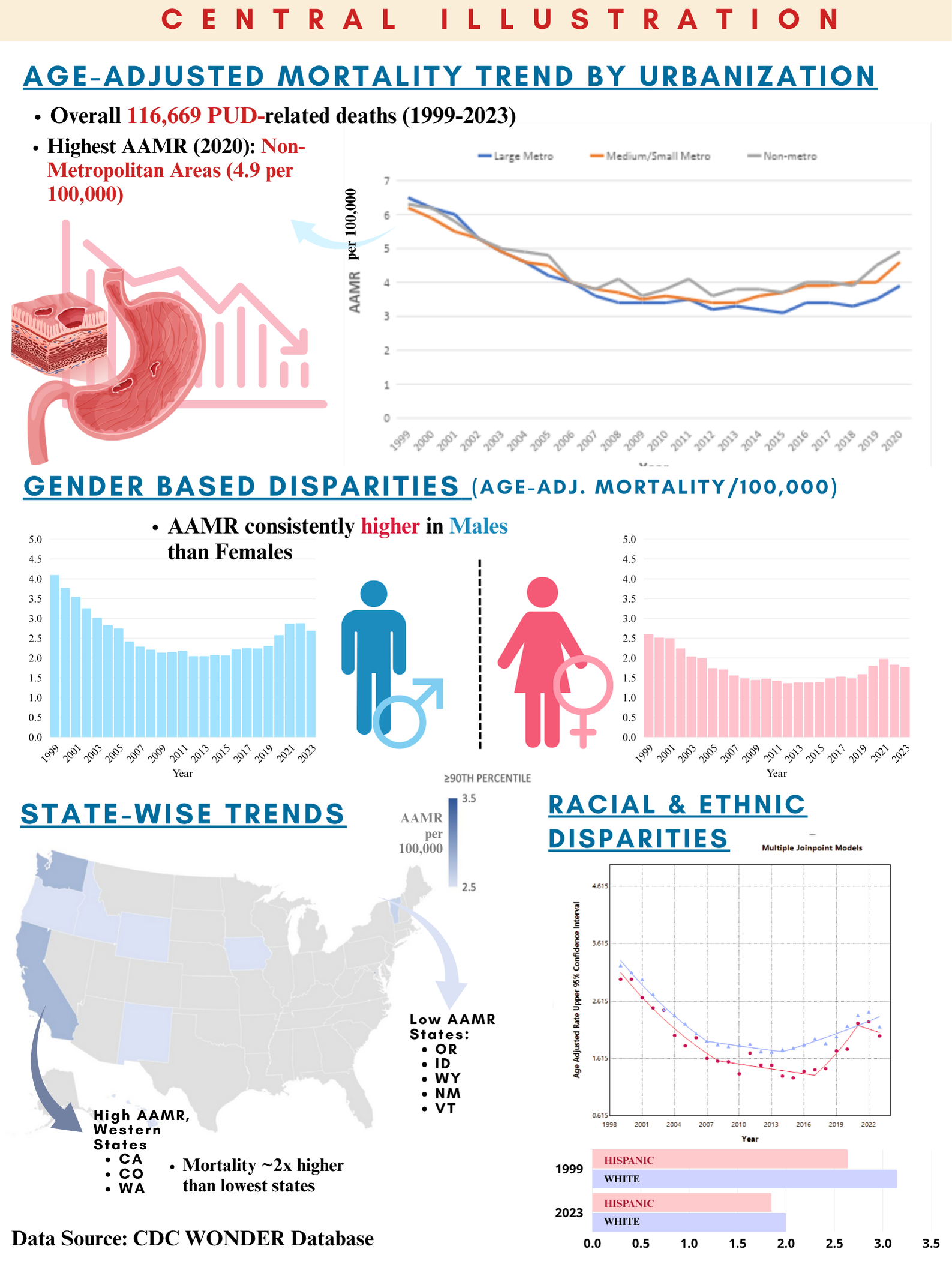
Figure: Figure1. Age-Adjusted Mortality Rate (AAMR) Trends and ARIMA Forecast of Mortality, 1999–2023
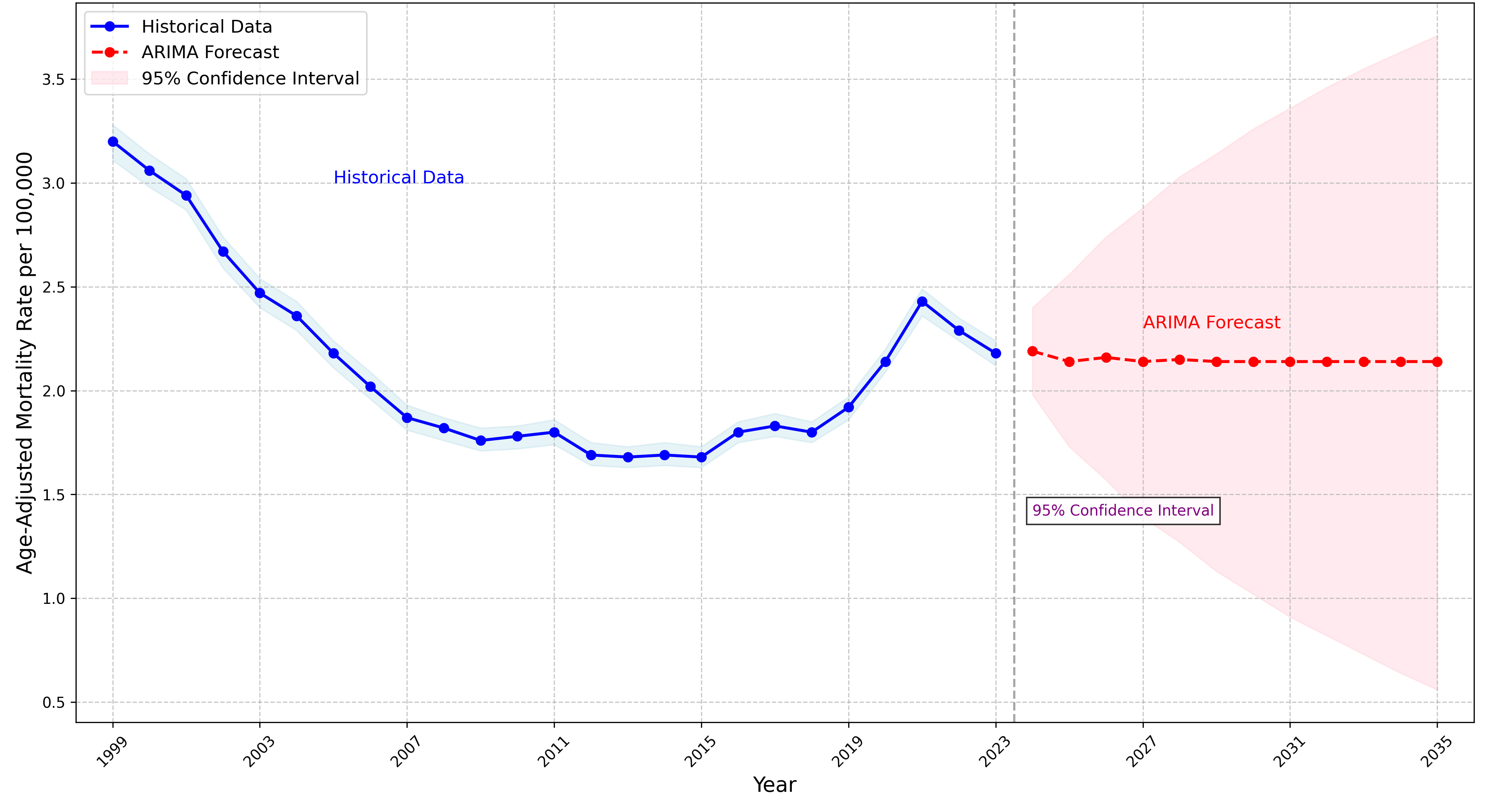
Figure: Figure 2. Changing Landscape of Peptic Ulcer Disease Mortality in the United States, 1999–2023
Disclosures:
Muhammad Umar indicated no relevant financial relationships.
Syeda Simrah Shah indicated no relevant financial relationships.
Amna Anwar indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Amin Abu Hejleh indicated no relevant financial relationships.
Anchit Chauhan indicated no relevant financial relationships.
Amine Rakab indicated no relevant financial relationships.
Ayesha Hidayat indicated no relevant financial relationships.
Muhammad Umar, MD1, Syeda Simrah Shah, MD2, Amna Anwar, MD3, Bisher Sawaf, MD4, Amin Abu Hejleh, MD5, Anchit Chauhan, 6, Amine Rakab, MD7, Ayesha Hidayat, MD8. P6332 - Trends of Recent Years With Future Forecasting of Peptic Ulcer Mortality in the United States (1999-2035), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
