Tuesday Poster Session
Category: Stomach and Spleen
P6325 - Cannabis and Gastroparesis: Higher Symptom Burden and Greater Healthcare Use
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ali Osman, MD, MSCI Candidate
Washington University School of Medicine in St. Louis
Ballwin, MO
Presenting Author(s)
Ali Osman, MD, MSCI Candidate1, Nur Sena Cagatay, MD2, Rbab A. Adam, 3, Thuraya Mussa, MD4, Mohamed Abdallah, MD5
1Washington University School of Medicine in St. Louis, Ballwin, MO; 2Wayne State University, Detroit, MI; 3Alyarmok university, Doha, Madinat ach Shamal, Qatar; 4Michigan State University, Lansing, MI; 5Corewell Health, Royal Oak, MI
Introduction: Cannabis use is increasingly prevalent among patients with gastrointestinal disorders, including gastroparesis. While it is often used to alleviate symptoms, its real-world impact on clinical outcomes and healthcare utilization in gastroparesis remains unclear.
Methods: We performed a retrospective cohort study using the TriNetX Global Collaborative Network, which aggregates de-identified electronic health records from 145 healthcare organizations. Adults aged ≥18 years with a diagnosis of gastroparesis were divided into two propensity score–matched cohorts: those with documented cannabis use (n=19,313) and those without (n=19,313). Cannabis exposure was defined using ICD-10 codes for cannabis use, abuse, or dependence. Patients with any malignancy or receipt of chemotherapy were excluded. Outcomes were evaluated over a 5-year follow-up period.
The primary outcome was the occurrence of emergency department visits, observation encounters, or inpatient admissions (proxy for healthcare utilization).
The secondary outcome was a composite of nausea/vomiting, abdominal pain, and malnutrition. Kaplan–Meier and risk analyses excluded patients who had the outcome prior to the index event.
Results: For the primary outcome, 27.4% of cannabis users had at least one acute care visit compared to 23.2% of non-users (Risk Ratio [RR]: 1.182; 95% CI: 1.114–1.254; p< 0.001). Time-to-event analysis demonstrated significantly earlier utilization in the cannabis group (Hazard Ratio [HR]: 1.419; 95% CI: 1.325–1.521; p< 0.001).
For the secondary outcome, 42.2% of patients in the cannabis cohort experienced symptoms versus 38.6% in the non-cannabis group (RR: 1.093; 95% CI: 1.029–1.161; p=0.005). Median symptom-free survival was shorter among cannabis users (825 vs. 1339 days; HR: 1.341; 95% CI: 1.238–1.451; p< 0.001).
Discussion: Cannabis use among patients with gastroparesis is associated with higher symptom burden and increased acute care utilization. These findings raise concern regarding the potential exacerbation of symptoms despite presumed symptom-relief use of cannabis.
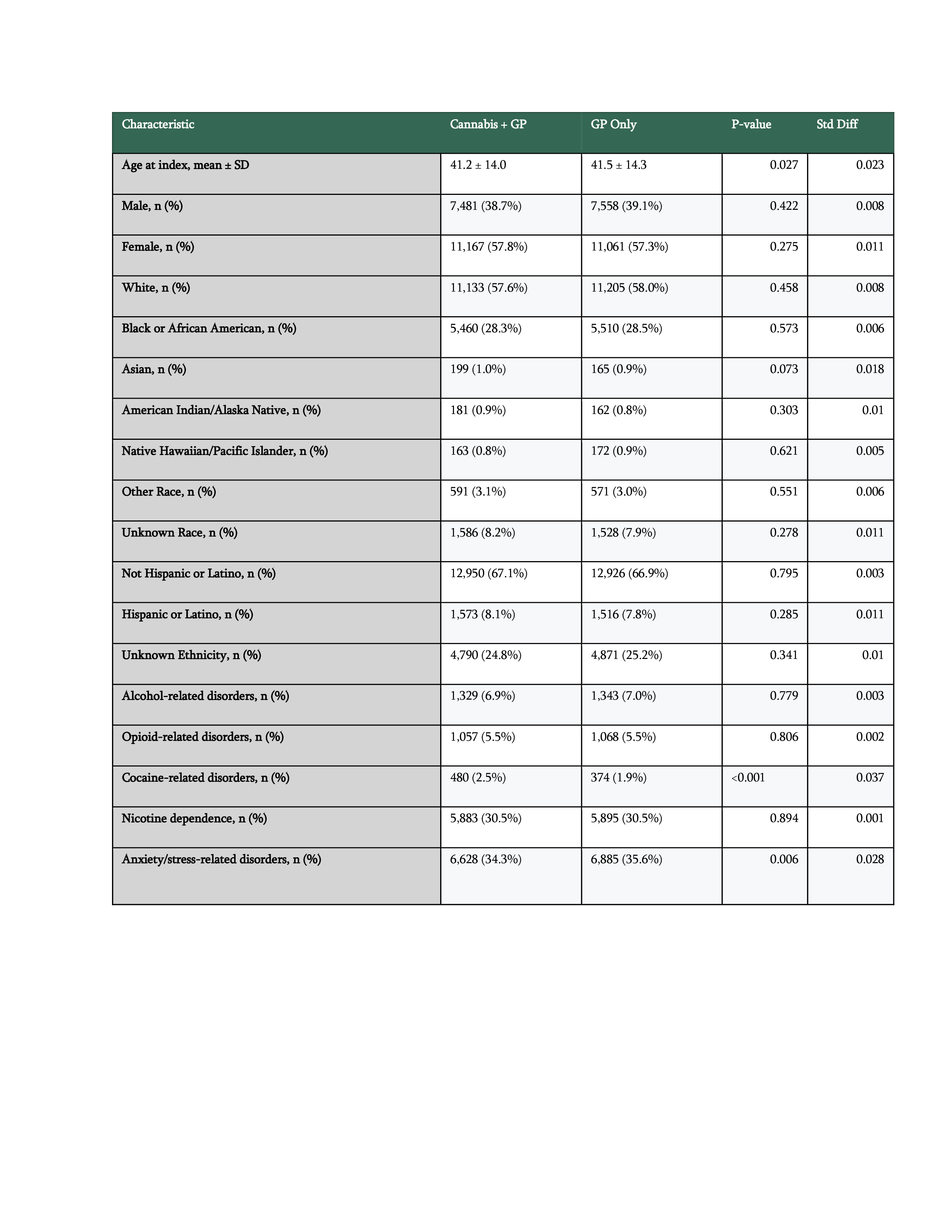
Figure: Table 1Baseline demographics and ethnicity in matched gastroparesis cohorts with and without cannabis use.

Figure: Fig-1: Risk of Symptom Burden and Healthcare Utilization
Disclosures:
Ali Osman indicated no relevant financial relationships.
Nur Sena Cagatay indicated no relevant financial relationships.
Rbab Adam indicated no relevant financial relationships.
Thuraya Mussa indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Ali Osman, MD, MSCI Candidate1, Nur Sena Cagatay, MD2, Rbab A. Adam, 3, Thuraya Mussa, MD4, Mohamed Abdallah, MD5. P6325 - Cannabis and Gastroparesis: Higher Symptom Burden and Greater Healthcare Use, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Washington University School of Medicine in St. Louis, Ballwin, MO; 2Wayne State University, Detroit, MI; 3Alyarmok university, Doha, Madinat ach Shamal, Qatar; 4Michigan State University, Lansing, MI; 5Corewell Health, Royal Oak, MI
Introduction: Cannabis use is increasingly prevalent among patients with gastrointestinal disorders, including gastroparesis. While it is often used to alleviate symptoms, its real-world impact on clinical outcomes and healthcare utilization in gastroparesis remains unclear.
Methods: We performed a retrospective cohort study using the TriNetX Global Collaborative Network, which aggregates de-identified electronic health records from 145 healthcare organizations. Adults aged ≥18 years with a diagnosis of gastroparesis were divided into two propensity score–matched cohorts: those with documented cannabis use (n=19,313) and those without (n=19,313). Cannabis exposure was defined using ICD-10 codes for cannabis use, abuse, or dependence. Patients with any malignancy or receipt of chemotherapy were excluded. Outcomes were evaluated over a 5-year follow-up period.
The primary outcome was the occurrence of emergency department visits, observation encounters, or inpatient admissions (proxy for healthcare utilization).
The secondary outcome was a composite of nausea/vomiting, abdominal pain, and malnutrition. Kaplan–Meier and risk analyses excluded patients who had the outcome prior to the index event.
Results: For the primary outcome, 27.4% of cannabis users had at least one acute care visit compared to 23.2% of non-users (Risk Ratio [RR]: 1.182; 95% CI: 1.114–1.254; p< 0.001). Time-to-event analysis demonstrated significantly earlier utilization in the cannabis group (Hazard Ratio [HR]: 1.419; 95% CI: 1.325–1.521; p< 0.001).
For the secondary outcome, 42.2% of patients in the cannabis cohort experienced symptoms versus 38.6% in the non-cannabis group (RR: 1.093; 95% CI: 1.029–1.161; p=0.005). Median symptom-free survival was shorter among cannabis users (825 vs. 1339 days; HR: 1.341; 95% CI: 1.238–1.451; p< 0.001).
Discussion: Cannabis use among patients with gastroparesis is associated with higher symptom burden and increased acute care utilization. These findings raise concern regarding the potential exacerbation of symptoms despite presumed symptom-relief use of cannabis.
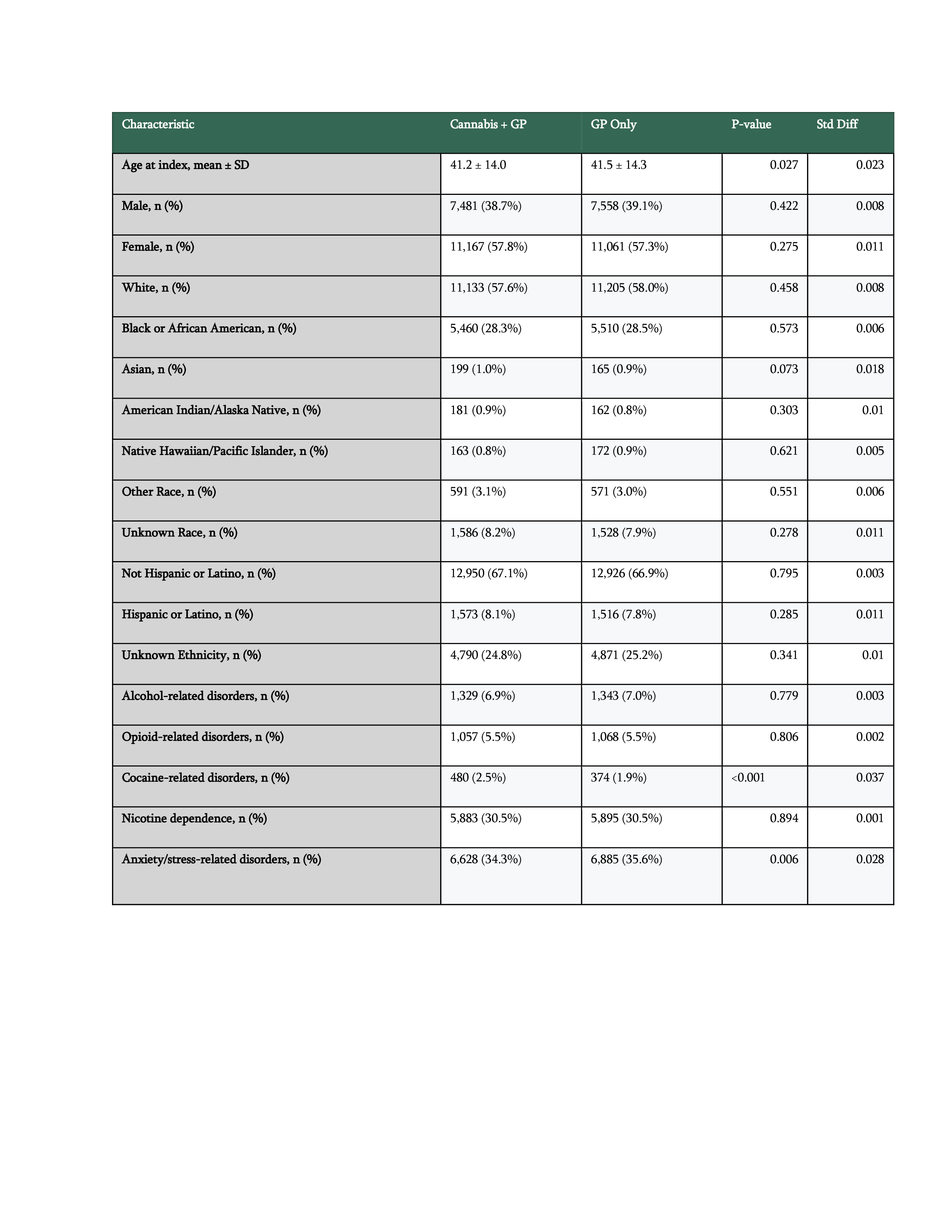
Figure: Table 1Baseline demographics and ethnicity in matched gastroparesis cohorts with and without cannabis use.

Figure: Fig-1: Risk of Symptom Burden and Healthcare Utilization
Disclosures:
Ali Osman indicated no relevant financial relationships.
Nur Sena Cagatay indicated no relevant financial relationships.
Rbab Adam indicated no relevant financial relationships.
Thuraya Mussa indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Ali Osman, MD, MSCI Candidate1, Nur Sena Cagatay, MD2, Rbab A. Adam, 3, Thuraya Mussa, MD4, Mohamed Abdallah, MD5. P6325 - Cannabis and Gastroparesis: Higher Symptom Burden and Greater Healthcare Use, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
