Tuesday Poster Session
Category: Stomach and Spleen
P6324 - Impact of Concomitant Clopidogrel and Proton Pump Inhibitor Use on Cardiovascular Outcomes in Acute Coronary Syndrome and Post-Revascularization Patients: A Matched Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Yahya Alhalalmeh, MD
New York Medical College - Saint Michael's Medical Center
Newark, NJ
Presenting Author(s)
Yahya Alhalalmeh, MD1, Omar Al Ta’ani, MD2, Ismail Althunibat, MD1, Murad Qirem, MD3, Mohammad Nabil Rayad, MD1, Mohamed Eldesouki, MD4, Yatinder Bains, MD1
1New York Medical College - Saint Michael's Medical Center, Newark, NJ; 2Department of Internal Medicine, Allegheny Health Network, Pittsburgh, Pennsylvania, USA, Pittsburgh, PA; 3New York Medical College - Saint Michael's Medical Center, West Orange, NJ; 4Saint Michael's Medical Center, New York Medical College, Newark, NJ
Introduction: Coronary artery disease remains a leading cause of mortality, with clopidogrel being a key therapy post-acute coronary syndrome (ACS) and coronary revascularization to prevent thrombotic events. However, its concurrent use with proton pump inhibitors (PPIs) for gastrointestinal protection is controversial, given potential interactions affecting clopidogrel's efficacy. This study examines the impact of this combination on major adverse cardiac events (MACE), stent thrombosis, and all-cause mortality.
Methods: This retrospective cohort study used the TriNetX database to identify patients >18 who had a first acute coronary syndrome (ACS) or coronary revascularization—either Percutaneous Coronary Intervention (PCI) or Coronary Artery Bypass Grafting (CABG)—between January 1, 2010, and December 31, 2023. Patients were divided into two groups: those treated with clopidogrel plus PPI and those with clopidogrel alone. Propensity score matching (1:1) balanced baseline factors including age, sex, comorbidities, labs, and medications (Figure 1). Cox proportional hazards models estimated hazard ratios (HRs) with 95% confidence intervals (CIs) for MACE, defined as unstable angina, myocardial infarction, coronary revascularization, cardiac arrest of cardiac origin, stent thrombosis, and all-cause mortality at 1- and 3-year follow-up.
Results: After propensity score matching, 124,341 patients were included in each group. At 1-year, patients on clopidogrel with PPIs exhibited increased risks compared to those on clopidogrel without PPI: MACE occurred with an HR of 1.16 (95% CI: 1.14–1.17, p < 0.01); stent thrombosis doubled in risk with an HR of 2.094 (95% CI: 1.83–2.40, p < 0.01); and all-cause mortality also showed an increase in risk with an HR of 1.38 (95% CI: 1.34–1.41, p < 0.01). At 3 years, the risks continued to be elevated with HRs of 1.17 (95% CI: 1.16–1.19, p < 0.01) for MACE, 1.94 (95% CI: 1.74–2.18, p < 0.01) for stent thrombosis, and 1.36 (95% CI: 1.33–1.39, p < 0.01) for all-cause mortality, as shown in Figure 2.
Discussion: The concurrent use of clopidogrel and PPIs in patients post-ACS and coronary revascularization is associated with significantly higher risks of MACE, stent thrombosis, and all-cause mortality compared to clopidogrel alone. These findings highlight the need for careful therapeutic planning to balance gastrointestinal protection with cardiovascular safety and support further studies to confirm these associations and optimize treatment strategies for affected patients.
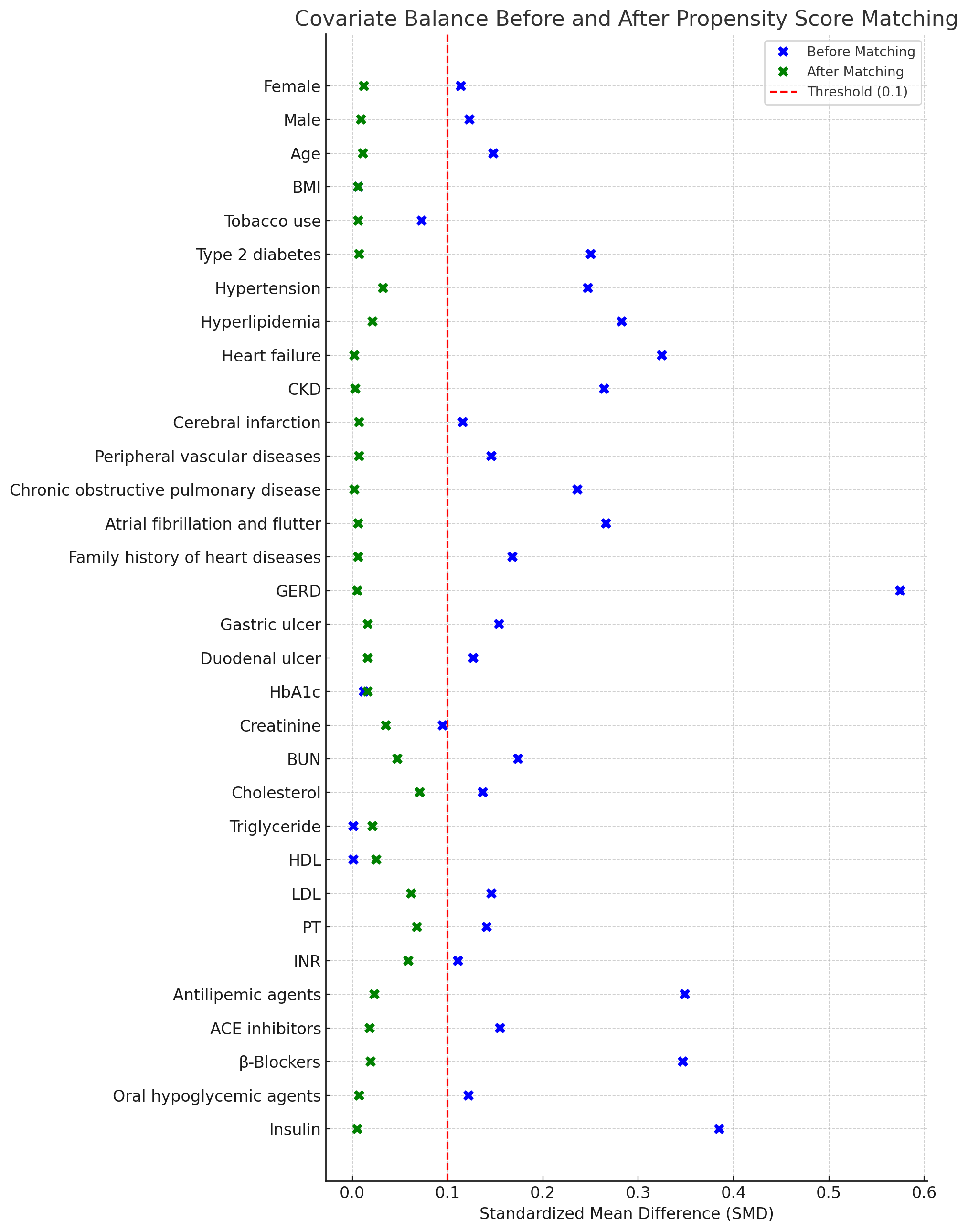
Figure: Figure 1
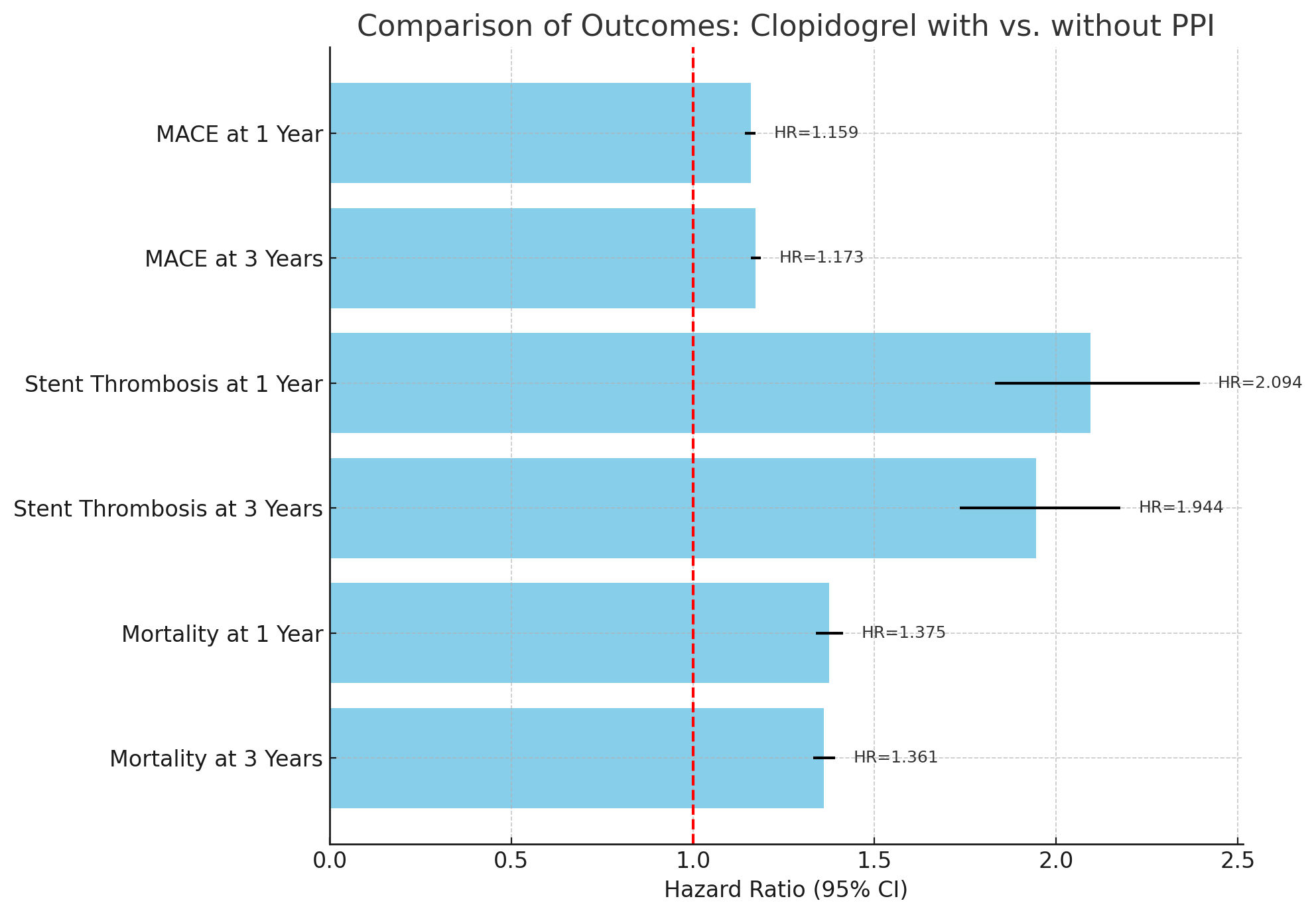
Figure: Figure 2
Disclosures:
Yahya Alhalalmeh indicated no relevant financial relationships.
Omar Al Ta’ani indicated no relevant financial relationships.
Ismail Althunibat indicated no relevant financial relationships.
Murad Qirem indicated no relevant financial relationships.
Mohammad Nabil Rayad indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Yatinder Bains indicated no relevant financial relationships.
Yahya Alhalalmeh, MD1, Omar Al Ta’ani, MD2, Ismail Althunibat, MD1, Murad Qirem, MD3, Mohammad Nabil Rayad, MD1, Mohamed Eldesouki, MD4, Yatinder Bains, MD1. P6324 - Impact of Concomitant Clopidogrel and Proton Pump Inhibitor Use on Cardiovascular Outcomes in Acute Coronary Syndrome and Post-Revascularization Patients: A Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1New York Medical College - Saint Michael's Medical Center, Newark, NJ; 2Department of Internal Medicine, Allegheny Health Network, Pittsburgh, Pennsylvania, USA, Pittsburgh, PA; 3New York Medical College - Saint Michael's Medical Center, West Orange, NJ; 4Saint Michael's Medical Center, New York Medical College, Newark, NJ
Introduction: Coronary artery disease remains a leading cause of mortality, with clopidogrel being a key therapy post-acute coronary syndrome (ACS) and coronary revascularization to prevent thrombotic events. However, its concurrent use with proton pump inhibitors (PPIs) for gastrointestinal protection is controversial, given potential interactions affecting clopidogrel's efficacy. This study examines the impact of this combination on major adverse cardiac events (MACE), stent thrombosis, and all-cause mortality.
Methods: This retrospective cohort study used the TriNetX database to identify patients >18 who had a first acute coronary syndrome (ACS) or coronary revascularization—either Percutaneous Coronary Intervention (PCI) or Coronary Artery Bypass Grafting (CABG)—between January 1, 2010, and December 31, 2023. Patients were divided into two groups: those treated with clopidogrel plus PPI and those with clopidogrel alone. Propensity score matching (1:1) balanced baseline factors including age, sex, comorbidities, labs, and medications (Figure 1). Cox proportional hazards models estimated hazard ratios (HRs) with 95% confidence intervals (CIs) for MACE, defined as unstable angina, myocardial infarction, coronary revascularization, cardiac arrest of cardiac origin, stent thrombosis, and all-cause mortality at 1- and 3-year follow-up.
Results: After propensity score matching, 124,341 patients were included in each group. At 1-year, patients on clopidogrel with PPIs exhibited increased risks compared to those on clopidogrel without PPI: MACE occurred with an HR of 1.16 (95% CI: 1.14–1.17, p < 0.01); stent thrombosis doubled in risk with an HR of 2.094 (95% CI: 1.83–2.40, p < 0.01); and all-cause mortality also showed an increase in risk with an HR of 1.38 (95% CI: 1.34–1.41, p < 0.01). At 3 years, the risks continued to be elevated with HRs of 1.17 (95% CI: 1.16–1.19, p < 0.01) for MACE, 1.94 (95% CI: 1.74–2.18, p < 0.01) for stent thrombosis, and 1.36 (95% CI: 1.33–1.39, p < 0.01) for all-cause mortality, as shown in Figure 2.
Discussion: The concurrent use of clopidogrel and PPIs in patients post-ACS and coronary revascularization is associated with significantly higher risks of MACE, stent thrombosis, and all-cause mortality compared to clopidogrel alone. These findings highlight the need for careful therapeutic planning to balance gastrointestinal protection with cardiovascular safety and support further studies to confirm these associations and optimize treatment strategies for affected patients.
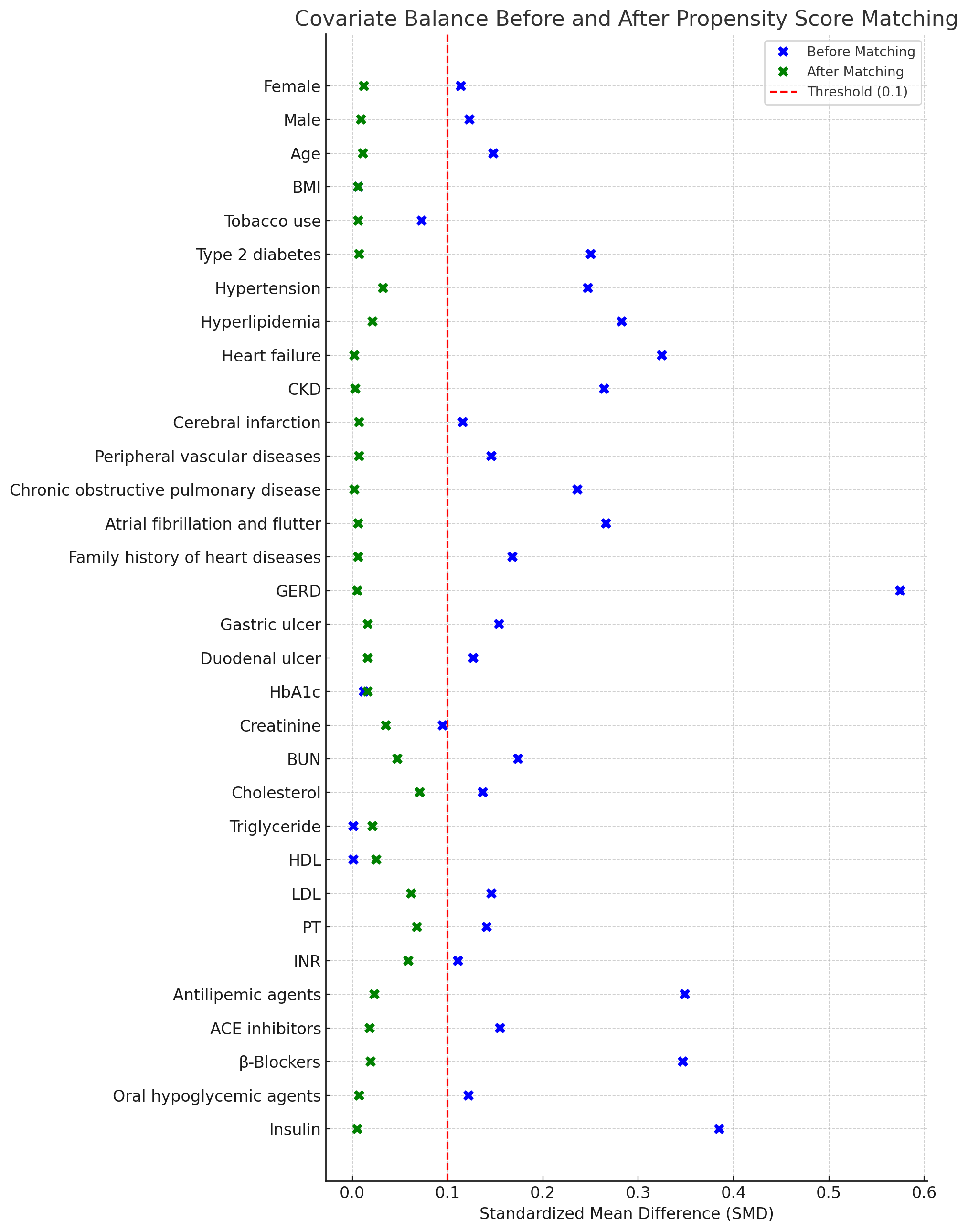
Figure: Figure 1
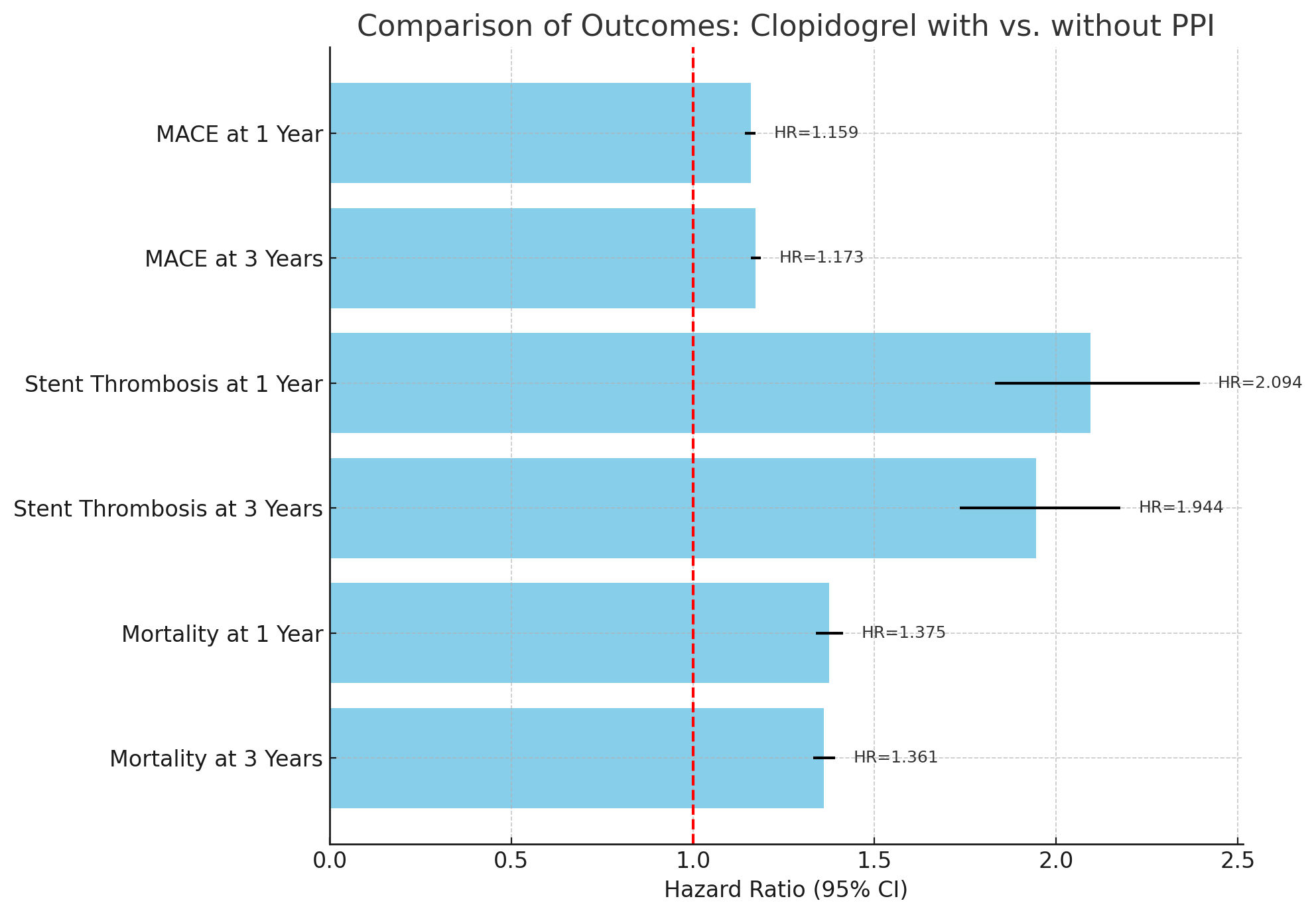
Figure: Figure 2
Disclosures:
Yahya Alhalalmeh indicated no relevant financial relationships.
Omar Al Ta’ani indicated no relevant financial relationships.
Ismail Althunibat indicated no relevant financial relationships.
Murad Qirem indicated no relevant financial relationships.
Mohammad Nabil Rayad indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Yatinder Bains indicated no relevant financial relationships.
Yahya Alhalalmeh, MD1, Omar Al Ta’ani, MD2, Ismail Althunibat, MD1, Murad Qirem, MD3, Mohammad Nabil Rayad, MD1, Mohamed Eldesouki, MD4, Yatinder Bains, MD1. P6324 - Impact of Concomitant Clopidogrel and Proton Pump Inhibitor Use on Cardiovascular Outcomes in Acute Coronary Syndrome and Post-Revascularization Patients: A Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
