Tuesday Poster Session
Category: Stomach and Spleen
P6322 - Comparative Outcomes of Gastrostomy Tube Placement: A Nationwide Analysis of Surgical, Endoscopic, and Interventional Radiology Approaches
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RV
Renuka Verma, MD (she/her/hers)
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
Renuka Verma, MD1, Kaitlyn Gernhard, DO2, Himsikhar Khataniar, MD3, Leandro Sierra, MD4, Sunny Kumar, MD5, Kamleshun Ramphul, MD6, Nikki Duong, MD7
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Allegheny Health Network Medicine Institute, Pittsburgh, PA; 3Allegheny General Hospital, Pittsburgh, PA; 4Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 5Wright Center for Graduate Medical Education, Scranton, PA; 6Independent researcher, Las Vegas, NV; 7Stanford University, Stanford, CA
Introduction: Gastrostomy tube (G-tube) insertions are performed in patients requiring long-term enteral nutrition and can be performed via a surgical, endoscopic, or interventional radiology (IR) approach. This study aims to compare the differences in demographics and clinical outcomes across these approaches and to evaluate the associated 30-day readmission rates.
Methods: Using the Nationwide Readmissions Database (NRD, 2020-2022), we generated a sample of hospitalized adults (excluding COVID-19 cases) who underwent G-tube insertion. Adjusted odds ratios for mortality during the index hospitalization were calculated, and demographics were compared between each group. We also assessed 30-day readmission rates and adjusted hazard ratios (HRs) for readmission.
Results: Among 123,557 patients, 4.82% underwent surgical placement, 90.31% IR-guided placement, and 4.87% via endoscopic approach. The overall mean age of all patients was 70.07 years, with the IR group containing the oldest patients. Across all cohorts, most were male and Medicare-insured. The surgical approach group included the most patients with cancer and had the highest rates of gastrostomy infection and in-hospital mortality. Although the surgical approach cohort had the highest 30-day readmission rate, it was not statistically significant [Hazard ratio(HR) in IR: 0.99, 95% CI 0.93-1.06, p=0.82 and HR in endoscopic: 0.94, 95% CI 0.85-1.03, p=0.17]. Time to first readmission was similar across all groups.
Discussion: This study suggests that interventional radiology may be the safest approach for gastrostomy tube placement, particularly in terms of reducing the risk of site infection, even among older patient cohorts. In contrast, the surgical approach was associated with the highest risk, including increased rates of G-tube site infection, cancer prevalence, and ICU admissions. Future research should focus on developing prognostic and risk-stratification tools to better guide the selection of G-tube placement methods tailored to individual patient profiles.
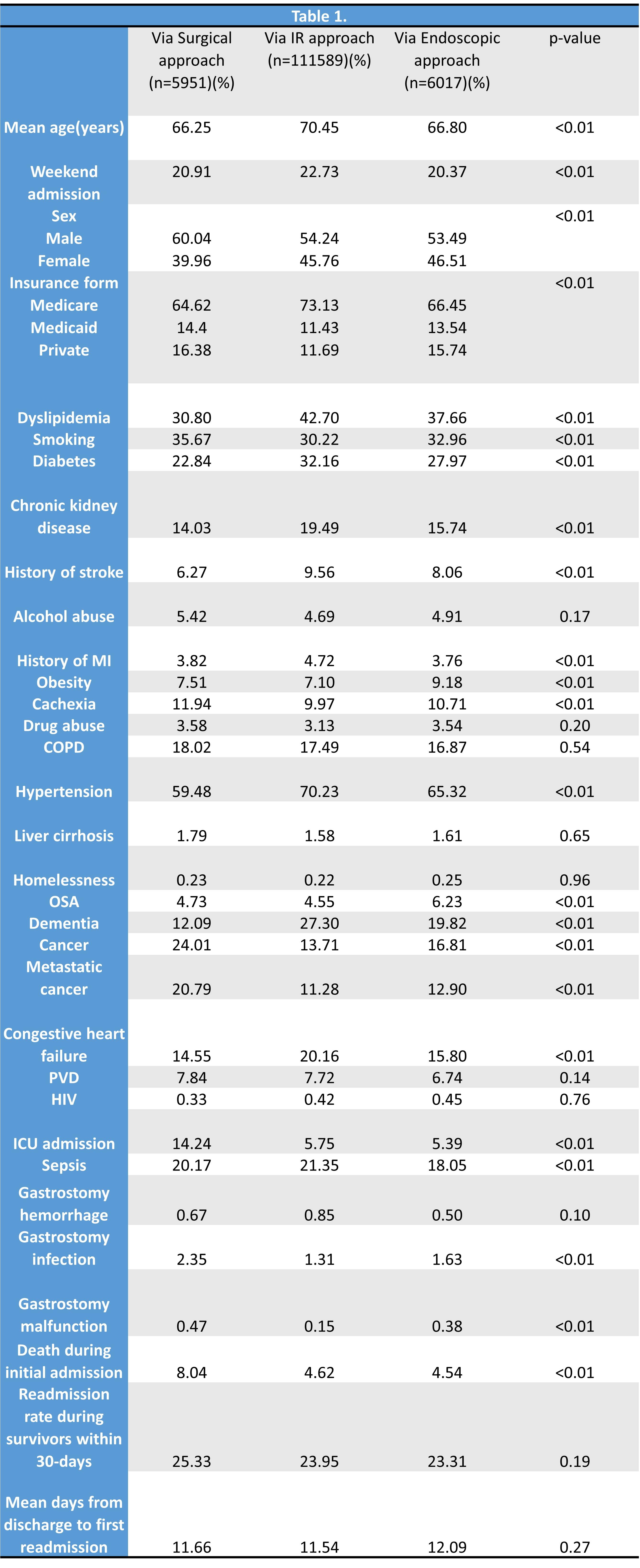
Figure: Table 1 - Demographics and outcomes in patients undergoing Gastrostomy tube placement
Disclosures:
Renuka Verma indicated no relevant financial relationships.
Kaitlyn Gernhard indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Leandro Sierra indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Kamleshun Ramphul indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Renuka Verma, MD1, Kaitlyn Gernhard, DO2, Himsikhar Khataniar, MD3, Leandro Sierra, MD4, Sunny Kumar, MD5, Kamleshun Ramphul, MD6, Nikki Duong, MD7. P6322 - Comparative Outcomes of Gastrostomy Tube Placement: A Nationwide Analysis of Surgical, Endoscopic, and Interventional Radiology Approaches, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Allegheny Health Network Medicine Institute, Pittsburgh, PA; 3Allegheny General Hospital, Pittsburgh, PA; 4Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 5Wright Center for Graduate Medical Education, Scranton, PA; 6Independent researcher, Las Vegas, NV; 7Stanford University, Stanford, CA
Introduction: Gastrostomy tube (G-tube) insertions are performed in patients requiring long-term enteral nutrition and can be performed via a surgical, endoscopic, or interventional radiology (IR) approach. This study aims to compare the differences in demographics and clinical outcomes across these approaches and to evaluate the associated 30-day readmission rates.
Methods: Using the Nationwide Readmissions Database (NRD, 2020-2022), we generated a sample of hospitalized adults (excluding COVID-19 cases) who underwent G-tube insertion. Adjusted odds ratios for mortality during the index hospitalization were calculated, and demographics were compared between each group. We also assessed 30-day readmission rates and adjusted hazard ratios (HRs) for readmission.
Results: Among 123,557 patients, 4.82% underwent surgical placement, 90.31% IR-guided placement, and 4.87% via endoscopic approach. The overall mean age of all patients was 70.07 years, with the IR group containing the oldest patients. Across all cohorts, most were male and Medicare-insured. The surgical approach group included the most patients with cancer and had the highest rates of gastrostomy infection and in-hospital mortality. Although the surgical approach cohort had the highest 30-day readmission rate, it was not statistically significant [Hazard ratio(HR) in IR: 0.99, 95% CI 0.93-1.06, p=0.82 and HR in endoscopic: 0.94, 95% CI 0.85-1.03, p=0.17]. Time to first readmission was similar across all groups.
Discussion: This study suggests that interventional radiology may be the safest approach for gastrostomy tube placement, particularly in terms of reducing the risk of site infection, even among older patient cohorts. In contrast, the surgical approach was associated with the highest risk, including increased rates of G-tube site infection, cancer prevalence, and ICU admissions. Future research should focus on developing prognostic and risk-stratification tools to better guide the selection of G-tube placement methods tailored to individual patient profiles.
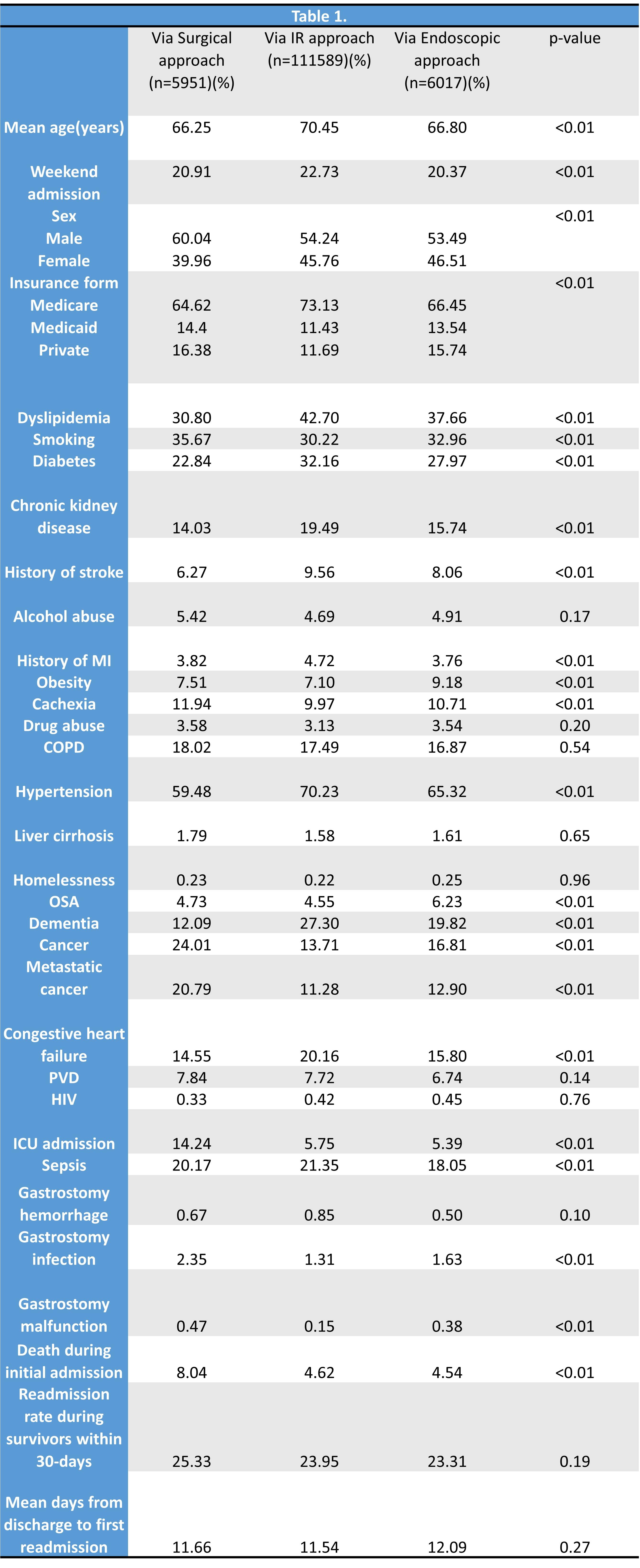
Figure: Table 1 - Demographics and outcomes in patients undergoing Gastrostomy tube placement
Disclosures:
Renuka Verma indicated no relevant financial relationships.
Kaitlyn Gernhard indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Leandro Sierra indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Kamleshun Ramphul indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Renuka Verma, MD1, Kaitlyn Gernhard, DO2, Himsikhar Khataniar, MD3, Leandro Sierra, MD4, Sunny Kumar, MD5, Kamleshun Ramphul, MD6, Nikki Duong, MD7. P6322 - Comparative Outcomes of Gastrostomy Tube Placement: A Nationwide Analysis of Surgical, Endoscopic, and Interventional Radiology Approaches, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
