Tuesday Poster Session
Category: Liver
P6136 - When a Fall Turns Fatal: Massive Hematoma in the Setting of Liver Cirrhosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Panida Charnvitayapong, MD (she/her/hers)
University of Miami Miller School of Medicine at JFK Medical Center
Atlantis, FL
Presenting Author(s)
Panida Charnvitayapong, MD, Magnolia McElyea, MD, Bebika Subedi, MD
University of Miami Miller School of Medicine at JFK Medical Center, Atlantis, FL
Introduction: Complex coagulopathies commonly accompany liver cirrhosis due to impaired synthesis of clotting factors, thrombocytopenia, and altered fibrinolysis. The liver plays a key role in maintaining the balance between pro- and anticoagulant pathways, making the risk of bleeding in these patients both unpredictable and potentially catastrophic. We present a case of acute blood loss anemia from a massive hematoma after a seemingly minor fall in a patient with cirrhosis.
Case Description/
Methods: A 56-year-old male with a known history of liver cirrhosis presented with dizziness, worsening over the past two days, though his spouse reported weeks of intermittent symptoms. On the day of presentation, he suffered a fall from standing. In the ED, he was hypotensive and tachycardic. His hemoglobin had acutely dropped from 10 to 4 g/dL. Physical exam was remarkable for an extensive hematoma of the right lateral chest and flank that was swollen and tender to palpation. Imaging of the chest and abdomen revealed a large curvilinear hematoma measuring 4.7 x 17.8 cm with no acute fracture but signs of cirrhosis and moderate ascites with no intra-abdominal hematoma, respectively. Lab evaluation revealed platelets 75K, INR 3.0, ammonia 33, AST 98, ALT 31, albumin 2.2, total bilirubin 8.0, and creatinine 1.66. His spouse noted he had previously undergone therapeutic paracenteses for ascites and was not known to have low blood pressure at home. The patient was admitted to the ICU, where he received multiple blood products and medical management. Unfortunately, the patient passed during the hospital course.
Discussion: Patients with cirrhosis can demonstrate both bleeding and thrombotic tendencies. Although standard labs such as INR and platelet count often suggest bleeding risk and liver function, they do not fully reflect the complex balance of hemostasis in cirrhosis. While the overall hemostatic state in cirrhotics may be “rebalanced,” this equilibrium is vulnerable. It can be easily affected by the severity of liver disease (presence of portal hypertension), renal dysfunction, disseminated intravascular coagulation (DIC), endothelial damage/injury, and underlying comorbidities.
The need for increased vigilance in cirrhotic patients presenting after trauma, no matter how minor, as well as rapid recognition and management of bleeding complications, is critical. Further research is needed to predict bleeding risk in this population and calls for more tools in cirrhosis-related coagulopathy assessment.
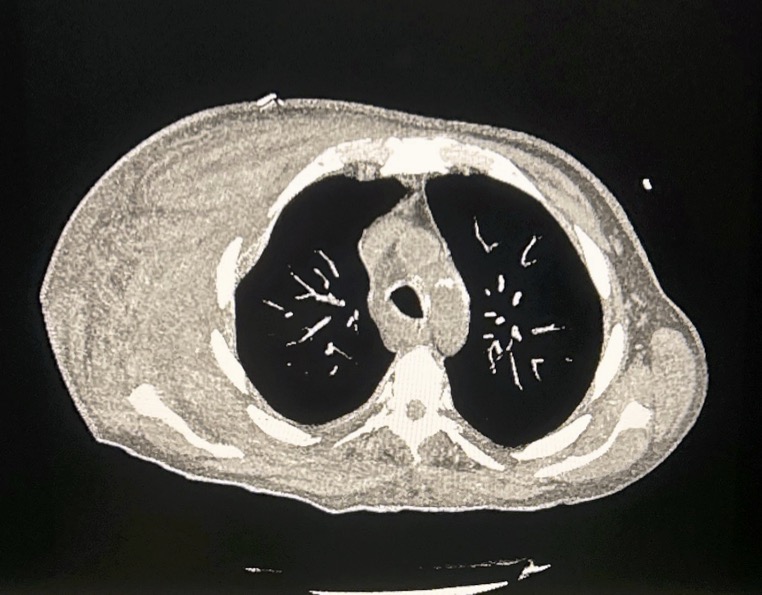
Figure: CT Thorax (axial): Large hematoma noted on patient's right
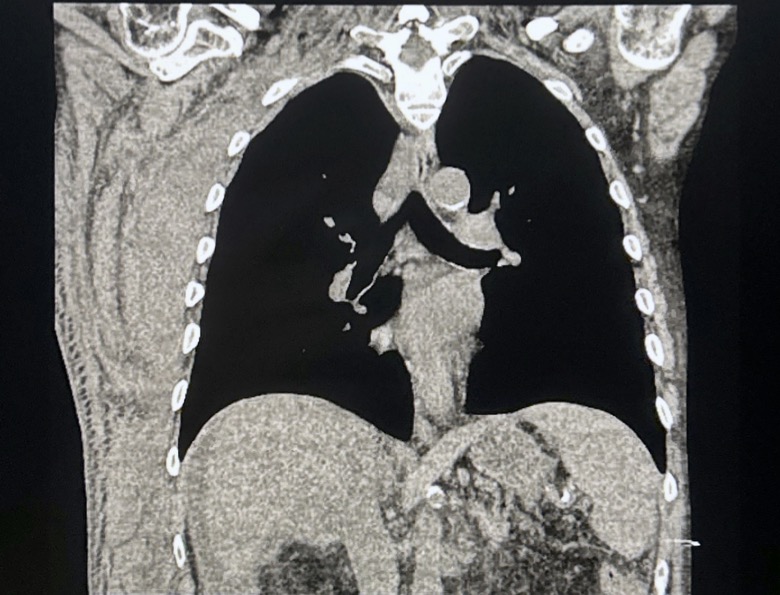
Figure: CT Thorax (Coronal): Large hematoma on patient's right
Disclosures:
Panida Charnvitayapong indicated no relevant financial relationships.
Magnolia McElyea indicated no relevant financial relationships.
Bebika Subedi indicated no relevant financial relationships.
Panida Charnvitayapong, MD, Magnolia McElyea, MD, Bebika Subedi, MD. P6136 - When a Fall Turns Fatal: Massive Hematoma in the Setting of Liver Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Miami Miller School of Medicine at JFK Medical Center, Atlantis, FL
Introduction: Complex coagulopathies commonly accompany liver cirrhosis due to impaired synthesis of clotting factors, thrombocytopenia, and altered fibrinolysis. The liver plays a key role in maintaining the balance between pro- and anticoagulant pathways, making the risk of bleeding in these patients both unpredictable and potentially catastrophic. We present a case of acute blood loss anemia from a massive hematoma after a seemingly minor fall in a patient with cirrhosis.
Case Description/
Methods: A 56-year-old male with a known history of liver cirrhosis presented with dizziness, worsening over the past two days, though his spouse reported weeks of intermittent symptoms. On the day of presentation, he suffered a fall from standing. In the ED, he was hypotensive and tachycardic. His hemoglobin had acutely dropped from 10 to 4 g/dL. Physical exam was remarkable for an extensive hematoma of the right lateral chest and flank that was swollen and tender to palpation. Imaging of the chest and abdomen revealed a large curvilinear hematoma measuring 4.7 x 17.8 cm with no acute fracture but signs of cirrhosis and moderate ascites with no intra-abdominal hematoma, respectively. Lab evaluation revealed platelets 75K, INR 3.0, ammonia 33, AST 98, ALT 31, albumin 2.2, total bilirubin 8.0, and creatinine 1.66. His spouse noted he had previously undergone therapeutic paracenteses for ascites and was not known to have low blood pressure at home. The patient was admitted to the ICU, where he received multiple blood products and medical management. Unfortunately, the patient passed during the hospital course.
Discussion: Patients with cirrhosis can demonstrate both bleeding and thrombotic tendencies. Although standard labs such as INR and platelet count often suggest bleeding risk and liver function, they do not fully reflect the complex balance of hemostasis in cirrhosis. While the overall hemostatic state in cirrhotics may be “rebalanced,” this equilibrium is vulnerable. It can be easily affected by the severity of liver disease (presence of portal hypertension), renal dysfunction, disseminated intravascular coagulation (DIC), endothelial damage/injury, and underlying comorbidities.
The need for increased vigilance in cirrhotic patients presenting after trauma, no matter how minor, as well as rapid recognition and management of bleeding complications, is critical. Further research is needed to predict bleeding risk in this population and calls for more tools in cirrhosis-related coagulopathy assessment.
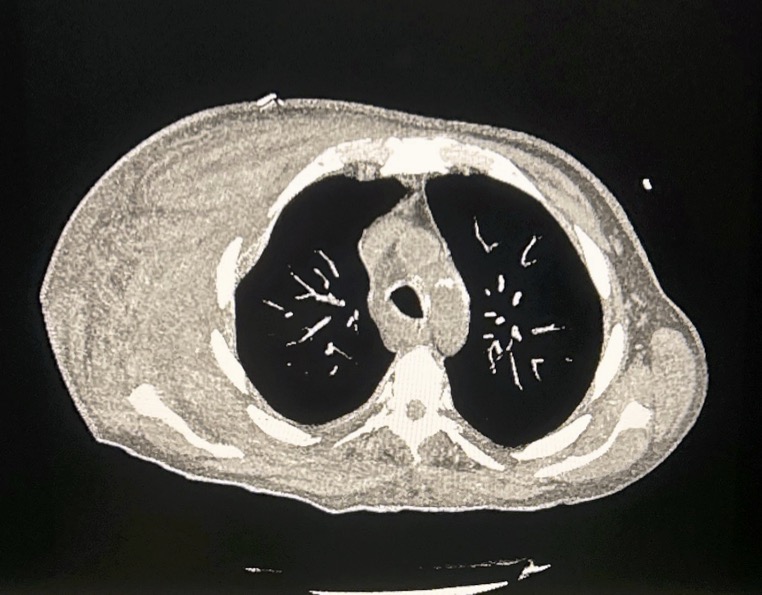
Figure: CT Thorax (axial): Large hematoma noted on patient's right
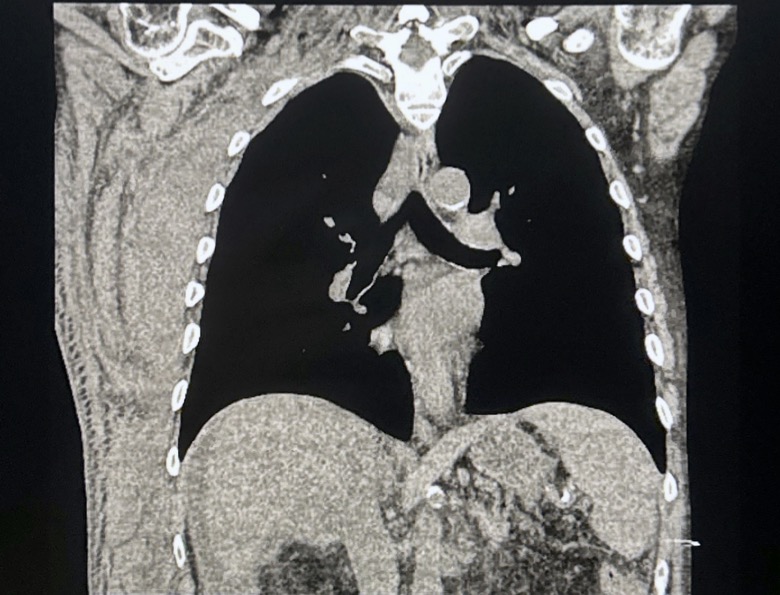
Figure: CT Thorax (Coronal): Large hematoma on patient's right
Disclosures:
Panida Charnvitayapong indicated no relevant financial relationships.
Magnolia McElyea indicated no relevant financial relationships.
Bebika Subedi indicated no relevant financial relationships.
Panida Charnvitayapong, MD, Magnolia McElyea, MD, Bebika Subedi, MD. P6136 - When a Fall Turns Fatal: Massive Hematoma in the Setting of Liver Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
