Tuesday Poster Session
Category: Liver
P6124 - Paracentesis-Induced Circulatory Dysfunction Leading to Motor Vehicle Accident: The Case for an Individualized Approach for Albumin Administration
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Omar Zuhdi, MD
Lakeland Regional Health Medical Center
Lakeland, FL
Presenting Author(s)
Award: ACG Presidential Poster Award
Omar Zuhdi, MD, Kayla Hernandez, MD, Zein Barakat, DO, Lauren Martinez, DO
Lakeland Regional Health Medical Center, Lakeland, FL
Introduction: Albumin administration following large volume paracentesis is routinely performed to prevent paracentesis-induced circulatory dysfunction. There is consensus on the benefits of albumin administration, however, there is variation in the recommended cutoff of the volume of fluid removed requiring albumin administration. While it is often recommended that albumin be administered after 5 L of fluid removal, we present a case of a patient with paracentesis-induced circulatory dysfunction leading to a motor vehicle accident after 4.7 L of fluid were removed during a paracentesis.
Case Description/
Methods: The patient is a 72-year-old female with a history of liver cirrhosis secondary to metabolic-associated steatohepatitis who presented as a trauma code following a motor vehicle accident. She had a syncopal episode and found herself in a ditch on the drive home following a routine paracentesis in which 4.7 L of fluid were removed, without administration of albumin. She routinely has had paracenteses in which 8-9 L of fluid were removed without previous complications. On physical examination, there were numerous skin abrasions, lacerations, and significant abdominal distention. CT abdomen and pelvis showed an acute compression fracture of the lumbar spine and evidence of moderate to severe abdominal ascites. Patient was found to have hypoalbuminemia at 2.79 g/dL, which was replenished. A syncopal workup was performed including EKG, echocardiogram, CT head, and carotid ultrasound which were all unremarkable. The syncopal episode leading to the motor vehicle accident was attributed to paracentesis-induced circulatory dysfunction due to lack of albumin administration.
Discussion: There is not a full consensus regarding the indications for albumin administration following paracentesis. However, albumin administration is generally recommended for large-volume paracentesis with greater than 5 L of fluid removed. However, patients may still present with paracentesis-induced circulatory dysfunction when less than 5 L are removed. The need for albumin should be adjusted based on factors including body habitus, renal dysfunction, and hypoalbuminemia. This can prevent adverse events following paracentesis while also avoiding unnecessary and futile administration of albumin. Individualized patient assessment is crucial in deciding albumin administration to prevent the use of albumin in unnecessary or futile instances, while also optimizing patient outcomes and preventing adverse events following paracentesis.
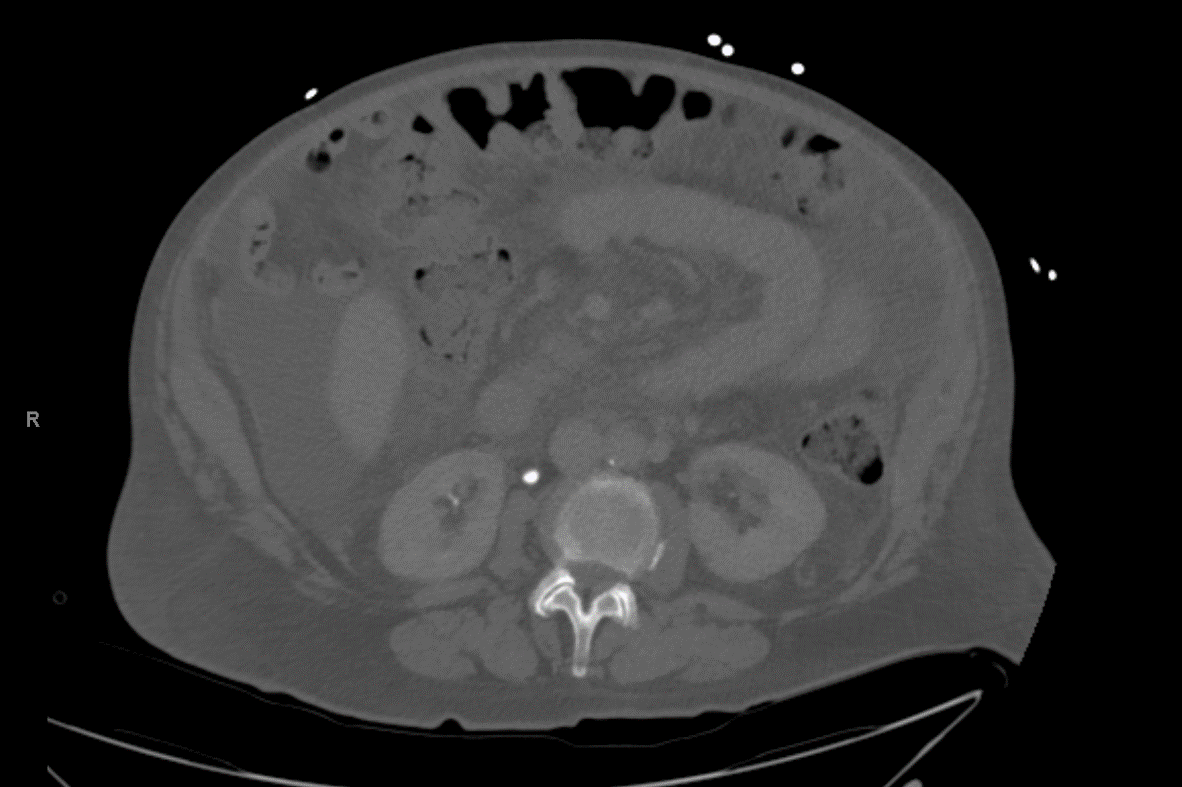
Figure: CT abdomen showed moderate to large amount of abdominal and pelvic ascites.

Figure: Acute compression fracture of L1 vertebrae noted with healing fracture of L2, L3, and L4.
Disclosures:
Omar Zuhdi indicated no relevant financial relationships.
Kayla Hernandez indicated no relevant financial relationships.
Zein Barakat indicated no relevant financial relationships.
Lauren Martinez indicated no relevant financial relationships.
Omar Zuhdi, MD, Kayla Hernandez, MD, Zein Barakat, DO, Lauren Martinez, DO. P6124 - Paracentesis-Induced Circulatory Dysfunction Leading to Motor Vehicle Accident: The Case for an Individualized Approach for Albumin Administration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Omar Zuhdi, MD, Kayla Hernandez, MD, Zein Barakat, DO, Lauren Martinez, DO
Lakeland Regional Health Medical Center, Lakeland, FL
Introduction: Albumin administration following large volume paracentesis is routinely performed to prevent paracentesis-induced circulatory dysfunction. There is consensus on the benefits of albumin administration, however, there is variation in the recommended cutoff of the volume of fluid removed requiring albumin administration. While it is often recommended that albumin be administered after 5 L of fluid removal, we present a case of a patient with paracentesis-induced circulatory dysfunction leading to a motor vehicle accident after 4.7 L of fluid were removed during a paracentesis.
Case Description/
Methods: The patient is a 72-year-old female with a history of liver cirrhosis secondary to metabolic-associated steatohepatitis who presented as a trauma code following a motor vehicle accident. She had a syncopal episode and found herself in a ditch on the drive home following a routine paracentesis in which 4.7 L of fluid were removed, without administration of albumin. She routinely has had paracenteses in which 8-9 L of fluid were removed without previous complications. On physical examination, there were numerous skin abrasions, lacerations, and significant abdominal distention. CT abdomen and pelvis showed an acute compression fracture of the lumbar spine and evidence of moderate to severe abdominal ascites. Patient was found to have hypoalbuminemia at 2.79 g/dL, which was replenished. A syncopal workup was performed including EKG, echocardiogram, CT head, and carotid ultrasound which were all unremarkable. The syncopal episode leading to the motor vehicle accident was attributed to paracentesis-induced circulatory dysfunction due to lack of albumin administration.
Discussion: There is not a full consensus regarding the indications for albumin administration following paracentesis. However, albumin administration is generally recommended for large-volume paracentesis with greater than 5 L of fluid removed. However, patients may still present with paracentesis-induced circulatory dysfunction when less than 5 L are removed. The need for albumin should be adjusted based on factors including body habitus, renal dysfunction, and hypoalbuminemia. This can prevent adverse events following paracentesis while also avoiding unnecessary and futile administration of albumin. Individualized patient assessment is crucial in deciding albumin administration to prevent the use of albumin in unnecessary or futile instances, while also optimizing patient outcomes and preventing adverse events following paracentesis.
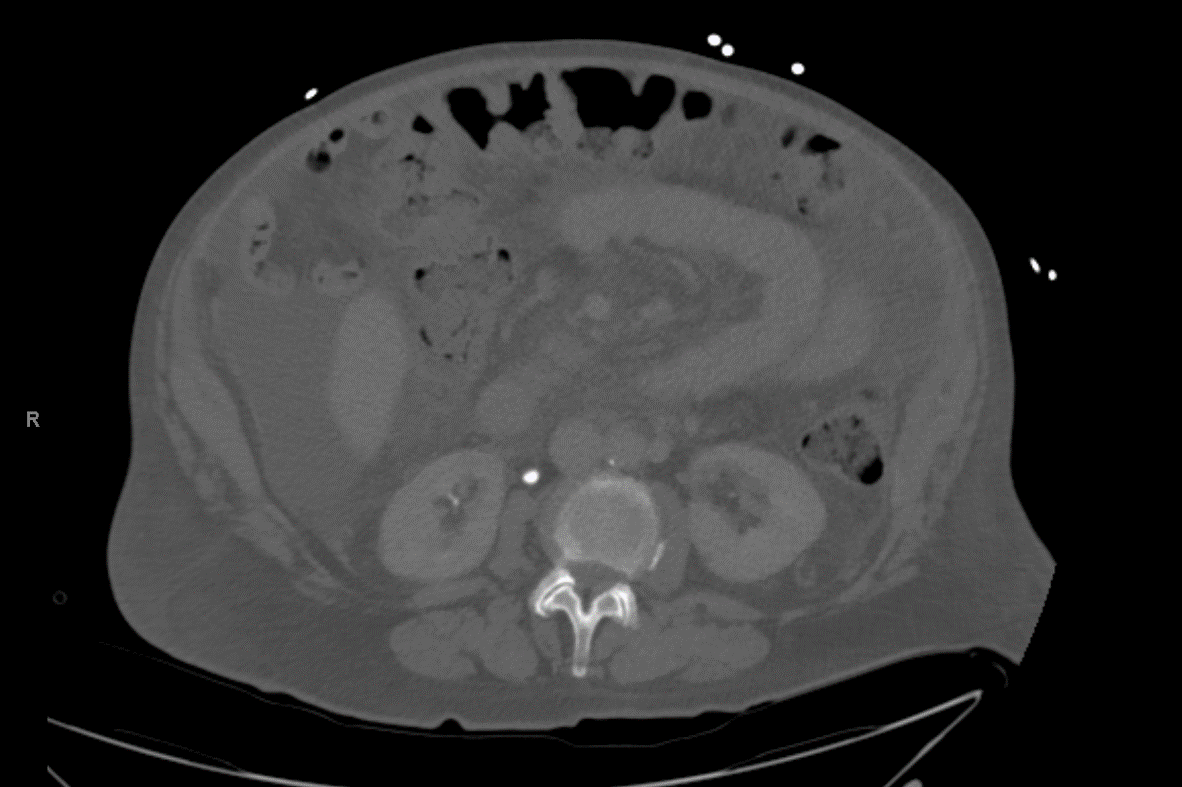
Figure: CT abdomen showed moderate to large amount of abdominal and pelvic ascites.

Figure: Acute compression fracture of L1 vertebrae noted with healing fracture of L2, L3, and L4.
Disclosures:
Omar Zuhdi indicated no relevant financial relationships.
Kayla Hernandez indicated no relevant financial relationships.
Zein Barakat indicated no relevant financial relationships.
Lauren Martinez indicated no relevant financial relationships.
Omar Zuhdi, MD, Kayla Hernandez, MD, Zein Barakat, DO, Lauren Martinez, DO. P6124 - Paracentesis-Induced Circulatory Dysfunction Leading to Motor Vehicle Accident: The Case for an Individualized Approach for Albumin Administration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

