Tuesday Poster Session
Category: Liver
P6121 - The PBC Enigma: When AMA Doesn’t Tell the Whole Story
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JG
Julie Gartland, MD (she/her/hers)
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Julie Gartland, MD1, Resham Ramkissoon, MD2, Yue Xue, MD, PhD1
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2university Hospitals Cleveland Medical Center, Case Western Reserve, Cleveland, OH
Introduction: Primary biliary cholangitis (PBC) is an uncommon cause of chronic liver disease. PBC is characterized by a triad of cholestasis, antimitochondrial antibodies (AMA), and histology showing destruction of intralobular bile ducts and portal inflammation. The mainstay of treatment is ursodiol which improves transplant free survival. We present a case of AMA- negative PBC with initial diagnosis of autoimmune hepatitis (AIH) versus AIH-PBC over-lap syndrome.
Case Description/
Methods: A 77-year-old female presented to our tertiary hepatology for persistently elevated liver enzymes. Her medical history was significant for hypertension and cholecystectomy. Review of her medications and supplements were noncontributory.
She had two years of mixed pattern elevation in liver enzymes less than 5 times the upper limit of normal. A liver ultrasound showed a coarse hepatic echotexture. Labs (Table 1) were notable for positive antinuclear antibody, positive anti-smooth muscle antibody (ASMA), negative AMA, and normal immunoglobulin G. A liver biopsy was read by a referring pathologist as hepatic pattern of injury with interface hepatitis, poorly formed granulomas, plasma cell enrichment of portal tracts, and lymphocytic inflammation. She was diagnosed with AIH versus AIH-PBC overlap syndrome.
Our hepatobiliary pathologist reviewed the biopsy and noted portal inflammation with mild interface activity, ductitis, bile duct injury, bile ductular reaction, patchy lobular inflammation and granulomas in the portal tracts and lobules (Figure 1). Further studies revealed a positive anti-sp100 antibody >200, and AMA- negative PBC was diagnosed. The patient started on ursodiol 15mg/kg/day and enzymes normalized two weeks after initiation.
Discussion: PBC is a T-cell mediated autoimmune liver disease with destruction of intralobular bile ducts. A hallmark of PBC is presence of AMA a highly sensitive and specific antibody 84 and 98 percent, respectively. AMA negative PBC and AIH-PBC overlap syndrome are common variants. With high clinical suspicion but negative AMA, ANA subtypes anti-gp210 and anti-sp100 can be evaluated. Anti-gp210 has a sensitivity and specificity based off meta-analysis of 27.2% and 98.5% similar to anti-sp100 21.3% and 97.7%, respectively. AMA-negative PBC is a rare and elusive diagnosis. Understanding the required workup and syndromes PBC can mimic is important for an accurate diagnosis and treatment to reduce morbidity and mortality.
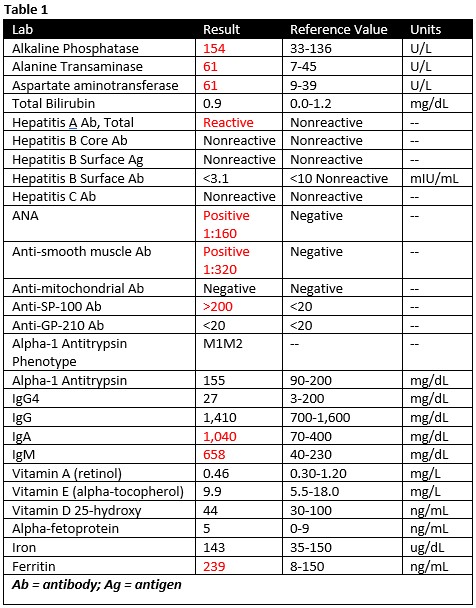
Figure: 1A 20x Magnification Trichrome stain showing bridging fibrosis
1B 40x Magnification CK7 immunostain highlighting intermediate cells, features suggestive of biliary process
1C 100x Magnification with noted Granuloma (black arrow) and portal inflammation (red arrow)
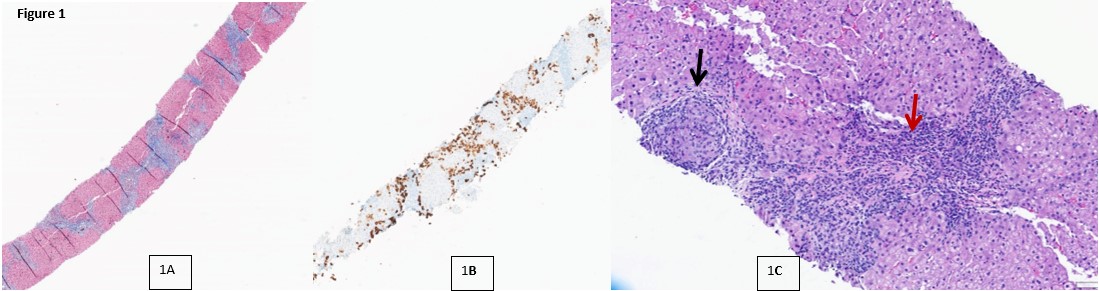
Figure: Laboratory workup with abnormal results depicted in red
Disclosures:
Julie Gartland indicated no relevant financial relationships.
Resham Ramkissoon indicated no relevant financial relationships.
Yue Xue indicated no relevant financial relationships.
Julie Gartland, MD1, Resham Ramkissoon, MD2, Yue Xue, MD, PhD1. P6121 - The PBC Enigma: When AMA Doesn’t Tell the Whole Story, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2university Hospitals Cleveland Medical Center, Case Western Reserve, Cleveland, OH
Introduction: Primary biliary cholangitis (PBC) is an uncommon cause of chronic liver disease. PBC is characterized by a triad of cholestasis, antimitochondrial antibodies (AMA), and histology showing destruction of intralobular bile ducts and portal inflammation. The mainstay of treatment is ursodiol which improves transplant free survival. We present a case of AMA- negative PBC with initial diagnosis of autoimmune hepatitis (AIH) versus AIH-PBC over-lap syndrome.
Case Description/
Methods: A 77-year-old female presented to our tertiary hepatology for persistently elevated liver enzymes. Her medical history was significant for hypertension and cholecystectomy. Review of her medications and supplements were noncontributory.
She had two years of mixed pattern elevation in liver enzymes less than 5 times the upper limit of normal. A liver ultrasound showed a coarse hepatic echotexture. Labs (Table 1) were notable for positive antinuclear antibody, positive anti-smooth muscle antibody (ASMA), negative AMA, and normal immunoglobulin G. A liver biopsy was read by a referring pathologist as hepatic pattern of injury with interface hepatitis, poorly formed granulomas, plasma cell enrichment of portal tracts, and lymphocytic inflammation. She was diagnosed with AIH versus AIH-PBC overlap syndrome.
Our hepatobiliary pathologist reviewed the biopsy and noted portal inflammation with mild interface activity, ductitis, bile duct injury, bile ductular reaction, patchy lobular inflammation and granulomas in the portal tracts and lobules (Figure 1). Further studies revealed a positive anti-sp100 antibody >200, and AMA- negative PBC was diagnosed. The patient started on ursodiol 15mg/kg/day and enzymes normalized two weeks after initiation.
Discussion: PBC is a T-cell mediated autoimmune liver disease with destruction of intralobular bile ducts. A hallmark of PBC is presence of AMA a highly sensitive and specific antibody 84 and 98 percent, respectively. AMA negative PBC and AIH-PBC overlap syndrome are common variants. With high clinical suspicion but negative AMA, ANA subtypes anti-gp210 and anti-sp100 can be evaluated. Anti-gp210 has a sensitivity and specificity based off meta-analysis of 27.2% and 98.5% similar to anti-sp100 21.3% and 97.7%, respectively. AMA-negative PBC is a rare and elusive diagnosis. Understanding the required workup and syndromes PBC can mimic is important for an accurate diagnosis and treatment to reduce morbidity and mortality.
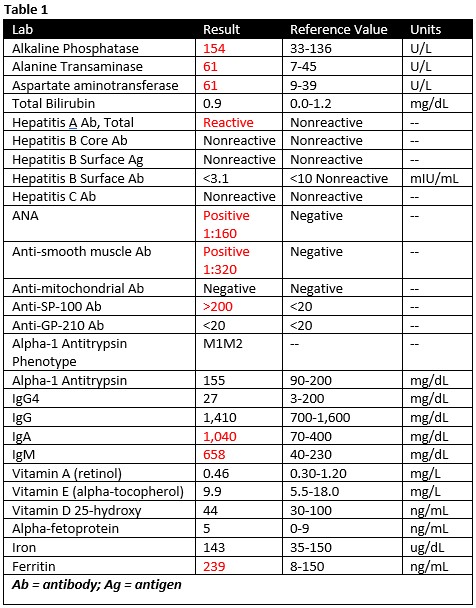
Figure: 1A 20x Magnification Trichrome stain showing bridging fibrosis
1B 40x Magnification CK7 immunostain highlighting intermediate cells, features suggestive of biliary process
1C 100x Magnification with noted Granuloma (black arrow) and portal inflammation (red arrow)
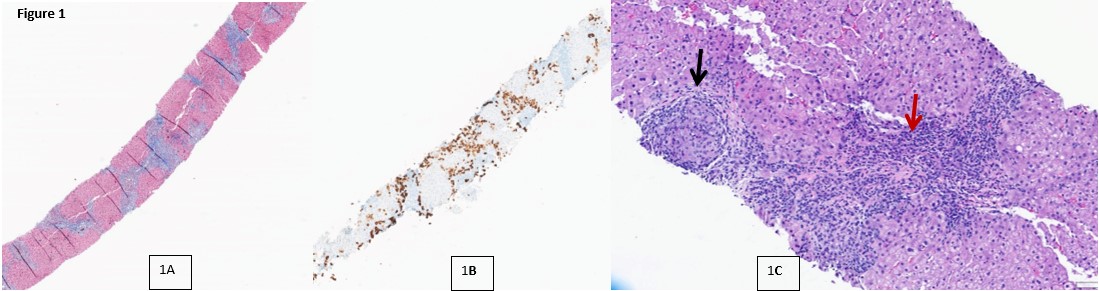
Figure: Laboratory workup with abnormal results depicted in red
Disclosures:
Julie Gartland indicated no relevant financial relationships.
Resham Ramkissoon indicated no relevant financial relationships.
Yue Xue indicated no relevant financial relationships.
Julie Gartland, MD1, Resham Ramkissoon, MD2, Yue Xue, MD, PhD1. P6121 - The PBC Enigma: When AMA Doesn’t Tell the Whole Story, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
