Tuesday Poster Session
Category: Liver
P6095 - Non-Diabetic Ketoacidosis Following Empagliflozin Initiation in a Patient With Alcohol-Associated Liver Disease: A Cautionary Tale
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sudheer Dhoop, MD
University of Toledo College Medicine and Life Sciences
Toledo, Ohio
Presenting Author(s)
Sudheer Dhoop, MD1, Sana Rabeeah, MD2, Luke Roberts, BS1, Keith Burns, MD1, Thomas Sodeman, MD3
1University of Toledo College Medicine and Life Sciences, Toledo, OH; 2The University of Toledo, Toledo, OH; 3University of Toledo College of Medicine and Life Sciences, Toledo, OH
Introduction: Sodium-glucose cotransporter-2 inhibitors (SGLT2Is) are increasingly used as guideline-directed therapy for congestive heart failure (CHF) and are being investigated for managing refractory ascites in cirrhosis as a diuretic. Their benefits extend to patients with metabolic-associated steatotic liver disease (MASLD), now a leading cause of cirrhosis. While SGLT2Is are associated with diabetic ketoacidosis (DKA), including euglycemic DKA (eDKA), data on their safety in advanced liver disease—particularly among those with active alcohol use—are limited. We present the first reported case of non-diabetic ketoacidosis (NDKA) following empagliflozin initiation in a patient with alcohol-associated liver disease.
Case Description/
Methods: A 67-year-old man with HFimpEF and decompensated alcohol-associated liver disease presented with dyspnea and peripheral edema. After inpatient diuresis, empagliflozin was initiated for CHF management and he was discharged. Four days later, he re-presented with abdominal pain, nausea, and fatigue. Labs showed an acidemia (pH=7.23), high anion gap metabolic acidosis (gap 28), elevated beta-hydroxybutyrate (8.2 mmol/L), hypoglycemia (69 mg/dL), and normal HbA1c (4.9%) (see Table 1). Imaging revealed hepatomegaly, a nodular liver, and small-volume ascites. He denied changes in alcohol intake (1–2 beers/day) or diet. Empagliflozin was discontinued, and symptoms rapidly resolved with IV dextrose and thiamine. His electrolyte panel 2 weeks post-discharge was normal and his creatinine was 0.4 lower than when empagliflozin was initiated (see Table 1) suggesting an early, unrecognized acute kidney injury (AKI) at that time.
Discussion: This case illustrates a perfect storm of an advanced liver disease state, active alcohol use, and SGLT2I initiation leading to NDKA. Alcohol metabolism increases ketogenesis, and patients with liver disease—even when abstinent—exhibit heightened ketone production under stress. Sarcopenia in cirrhosis may obscure AKI by falsely lowering serum creatinine. Although trials support SGLT2I safety in cirrhosis, they excluded patients with active alcohol use. Phosphatidylethanol (PEth) testing may help identify high-risk patients prior to initiation of SGLT2Is in these patients. Caution is warranted when prescribing these agents in advanced liver disease despite their potential benefits in heart failure, refractory ascites, and MASLD.
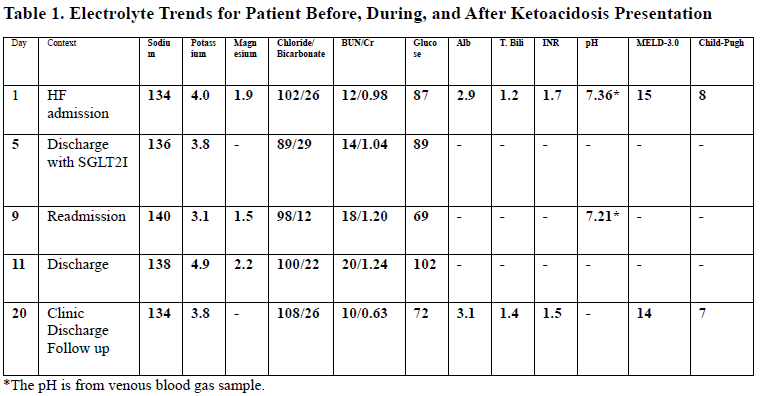
Figure: Table 1. Electrolyte Trends for Patient Before, During, and After Ketoacidosis Presentation
Disclosures:
Sudheer Dhoop indicated no relevant financial relationships.
Sana Rabeeah indicated no relevant financial relationships.
Luke Roberts indicated no relevant financial relationships.
Keith Burns indicated no relevant financial relationships.
Thomas Sodeman indicated no relevant financial relationships.
Sudheer Dhoop, MD1, Sana Rabeeah, MD2, Luke Roberts, BS1, Keith Burns, MD1, Thomas Sodeman, MD3. P6095 - Non-Diabetic Ketoacidosis Following Empagliflozin Initiation in a Patient With Alcohol-Associated Liver Disease: A Cautionary Tale, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Toledo College Medicine and Life Sciences, Toledo, OH; 2The University of Toledo, Toledo, OH; 3University of Toledo College of Medicine and Life Sciences, Toledo, OH
Introduction: Sodium-glucose cotransporter-2 inhibitors (SGLT2Is) are increasingly used as guideline-directed therapy for congestive heart failure (CHF) and are being investigated for managing refractory ascites in cirrhosis as a diuretic. Their benefits extend to patients with metabolic-associated steatotic liver disease (MASLD), now a leading cause of cirrhosis. While SGLT2Is are associated with diabetic ketoacidosis (DKA), including euglycemic DKA (eDKA), data on their safety in advanced liver disease—particularly among those with active alcohol use—are limited. We present the first reported case of non-diabetic ketoacidosis (NDKA) following empagliflozin initiation in a patient with alcohol-associated liver disease.
Case Description/
Methods: A 67-year-old man with HFimpEF and decompensated alcohol-associated liver disease presented with dyspnea and peripheral edema. After inpatient diuresis, empagliflozin was initiated for CHF management and he was discharged. Four days later, he re-presented with abdominal pain, nausea, and fatigue. Labs showed an acidemia (pH=7.23), high anion gap metabolic acidosis (gap 28), elevated beta-hydroxybutyrate (8.2 mmol/L), hypoglycemia (69 mg/dL), and normal HbA1c (4.9%) (see Table 1). Imaging revealed hepatomegaly, a nodular liver, and small-volume ascites. He denied changes in alcohol intake (1–2 beers/day) or diet. Empagliflozin was discontinued, and symptoms rapidly resolved with IV dextrose and thiamine. His electrolyte panel 2 weeks post-discharge was normal and his creatinine was 0.4 lower than when empagliflozin was initiated (see Table 1) suggesting an early, unrecognized acute kidney injury (AKI) at that time.
Discussion: This case illustrates a perfect storm of an advanced liver disease state, active alcohol use, and SGLT2I initiation leading to NDKA. Alcohol metabolism increases ketogenesis, and patients with liver disease—even when abstinent—exhibit heightened ketone production under stress. Sarcopenia in cirrhosis may obscure AKI by falsely lowering serum creatinine. Although trials support SGLT2I safety in cirrhosis, they excluded patients with active alcohol use. Phosphatidylethanol (PEth) testing may help identify high-risk patients prior to initiation of SGLT2Is in these patients. Caution is warranted when prescribing these agents in advanced liver disease despite their potential benefits in heart failure, refractory ascites, and MASLD.
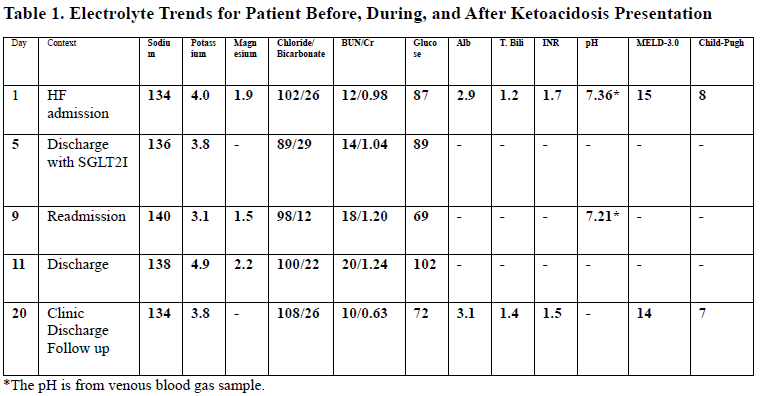
Figure: Table 1. Electrolyte Trends for Patient Before, During, and After Ketoacidosis Presentation
Disclosures:
Sudheer Dhoop indicated no relevant financial relationships.
Sana Rabeeah indicated no relevant financial relationships.
Luke Roberts indicated no relevant financial relationships.
Keith Burns indicated no relevant financial relationships.
Thomas Sodeman indicated no relevant financial relationships.
Sudheer Dhoop, MD1, Sana Rabeeah, MD2, Luke Roberts, BS1, Keith Burns, MD1, Thomas Sodeman, MD3. P6095 - Non-Diabetic Ketoacidosis Following Empagliflozin Initiation in a Patient With Alcohol-Associated Liver Disease: A Cautionary Tale, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
