Tuesday Poster Session
Category: Liver
P6091 - Hemolytic Anemia and Hepatitis in the Setting of Acute Epstein-Barr Virus Infection
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SS
Sargun Singh, MBBS
Case Western Reserve University School of Medicine
Cleveland, OH
Presenting Author(s)
Sargun Singh, MBBS1, Yujie Zhang, MD, PhD2, Vu Nguyen, MD3
1Case Western Reserve University School of Medicine, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: Epstein Barr Virus (EBV) infection, common in adult population, presents as viral prodrome of fever, fatigue, lethargy, sore throat, & tender cervical lymphadenopathy (LAD). Acute infection can induce hepatitis. Rarely, hemolytic anemia is reported. We describe case of a young man presenting with hemolytic anemia & hepatitis in the setting of acute EBV infection.
Case Description/
Methods: A 21-year-old Caucasian man without notable past medical history presented with jaundice, fever, joint pain, rash, dark urine. Physical examination was significant for scleral icterus, jaundice, pharyngeal erythema, tender cervical LAD, patches of petechial rash on right upper limb.
Elevated total bilirubin with indirect bilirubinemia & transaminitis were noted (Table 1). High lactate dehydrogenase, low haptoglobin, mildly increased reticulocyte count (2.7%) with immature retic fraction at 19.2% indicated hemolysis. EBV DNA PCR was 867 IU/ml. Immunoglobulin (Ig) M antibodies against viral capsid antigen (VCA) were positive, IgG was negative. Infectious etiologies like babesia, rickettsia, histoplasma, blastomycoses, viruses like varicella, CMV, HSV, parvovirus, hepatitis B/C, HIV were ruled out. Antibodies for autoimmune disease, acute toxicology panel, & blood culture were normal. Peripheral smear showed reactive lymphocytes. Abdominal ultrasound revealed splenomegaly, normal liver.
Over hospital course, arthralgia, rash, tender LAD resolved. Bilirubin trended down but AST/ALT increased (Table 1). Albumin, INR, prothrombin time were normal, indicative of intact synthetic liver function. Ultrasound-guided liver biopsy (bx) showed lymphocytic infiltrates in sinusoids & portal tracts, consistent with EBV hepatitis. Lobular architecture was preserved with evidence of lobular inflammation, focal acidophil bodies (hepatocyte apoptosis), scattered mitotic figures (Figure 1).
Labs, liver bx with clinical picture suggested acute EBV infection with hepatocellular pattern of liver injury & hemolytic anemia, managed with supportive treatment/monitoring.
Discussion: Hemolytic anemia in acute EBV is rare & mostly immune-mediated. Hepatitis is self-limiting, rarely results in liver failure. Uncommonly, splenic rupture occurs. A viral prodrome of non-specific symptoms with jaundice & lab findings suggestive of hemolysis in young patients should warrant testing for EBV to avoid complications. Early EBV determination, initiation of supportive care carry favorable prognosis.
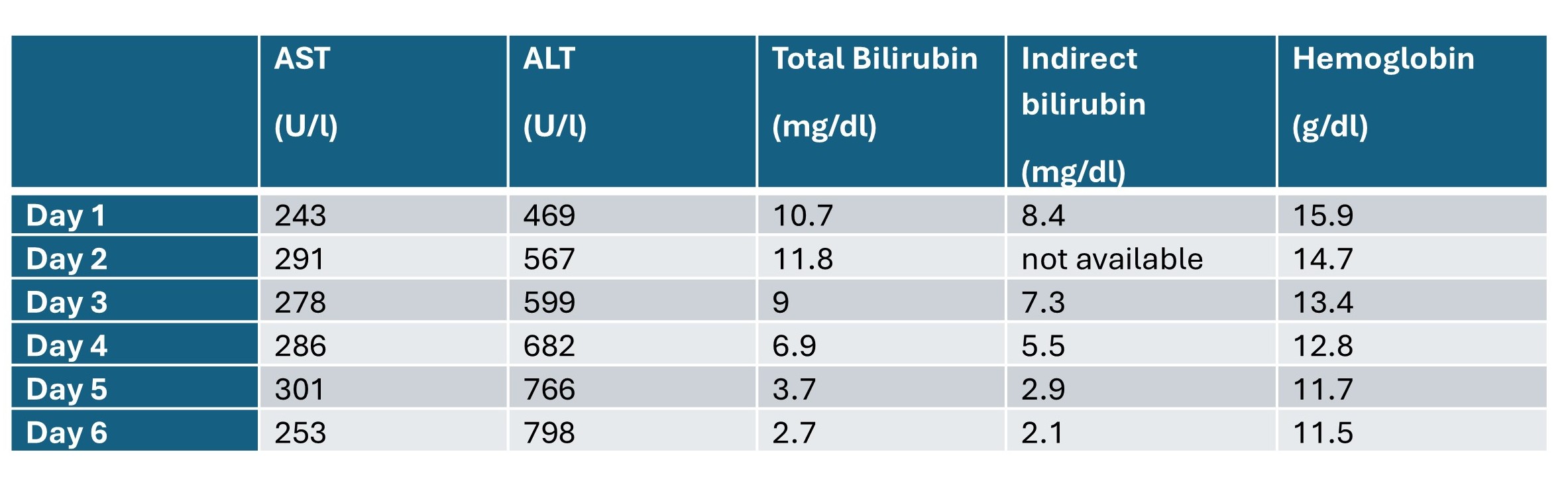
Figure: Table 1: Liver enzyme and hemoglobin trends over the course of hospitalization
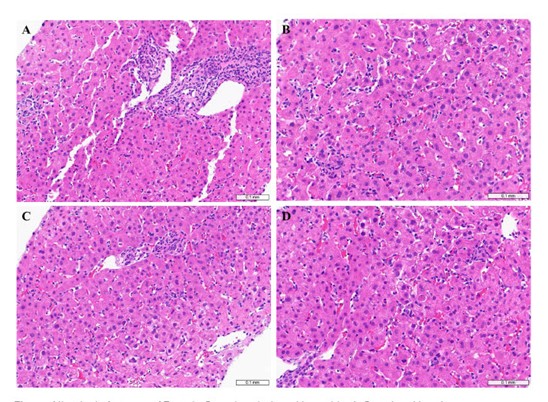
Figure: Figure 1: Histologic features of Epstein-Barr virus-induced hepatitis. A. Portal and locular lymphocytic inflammation. B. Sinusoidal lymphocytic infiltrates. C. Scattered mitotic figures. D. Rare acidophil bodies.
Disclosures:
Sargun Singh indicated no relevant financial relationships.
Yujie Zhang indicated no relevant financial relationships.
Vu Nguyen: AbbVie – Consultant, Speakers Bureau. Johnson & Johnson – Consultant, Speakers Bureau.
Sargun Singh, MBBS1, Yujie Zhang, MD, PhD2, Vu Nguyen, MD3. P6091 - Hemolytic Anemia and Hepatitis in the Setting of Acute Epstein-Barr Virus Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Case Western Reserve University School of Medicine, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Cleveland, OH; 3University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: Epstein Barr Virus (EBV) infection, common in adult population, presents as viral prodrome of fever, fatigue, lethargy, sore throat, & tender cervical lymphadenopathy (LAD). Acute infection can induce hepatitis. Rarely, hemolytic anemia is reported. We describe case of a young man presenting with hemolytic anemia & hepatitis in the setting of acute EBV infection.
Case Description/
Methods: A 21-year-old Caucasian man without notable past medical history presented with jaundice, fever, joint pain, rash, dark urine. Physical examination was significant for scleral icterus, jaundice, pharyngeal erythema, tender cervical LAD, patches of petechial rash on right upper limb.
Elevated total bilirubin with indirect bilirubinemia & transaminitis were noted (Table 1). High lactate dehydrogenase, low haptoglobin, mildly increased reticulocyte count (2.7%) with immature retic fraction at 19.2% indicated hemolysis. EBV DNA PCR was 867 IU/ml. Immunoglobulin (Ig) M antibodies against viral capsid antigen (VCA) were positive, IgG was negative. Infectious etiologies like babesia, rickettsia, histoplasma, blastomycoses, viruses like varicella, CMV, HSV, parvovirus, hepatitis B/C, HIV were ruled out. Antibodies for autoimmune disease, acute toxicology panel, & blood culture were normal. Peripheral smear showed reactive lymphocytes. Abdominal ultrasound revealed splenomegaly, normal liver.
Over hospital course, arthralgia, rash, tender LAD resolved. Bilirubin trended down but AST/ALT increased (Table 1). Albumin, INR, prothrombin time were normal, indicative of intact synthetic liver function. Ultrasound-guided liver biopsy (bx) showed lymphocytic infiltrates in sinusoids & portal tracts, consistent with EBV hepatitis. Lobular architecture was preserved with evidence of lobular inflammation, focal acidophil bodies (hepatocyte apoptosis), scattered mitotic figures (Figure 1).
Labs, liver bx with clinical picture suggested acute EBV infection with hepatocellular pattern of liver injury & hemolytic anemia, managed with supportive treatment/monitoring.
Discussion: Hemolytic anemia in acute EBV is rare & mostly immune-mediated. Hepatitis is self-limiting, rarely results in liver failure. Uncommonly, splenic rupture occurs. A viral prodrome of non-specific symptoms with jaundice & lab findings suggestive of hemolysis in young patients should warrant testing for EBV to avoid complications. Early EBV determination, initiation of supportive care carry favorable prognosis.
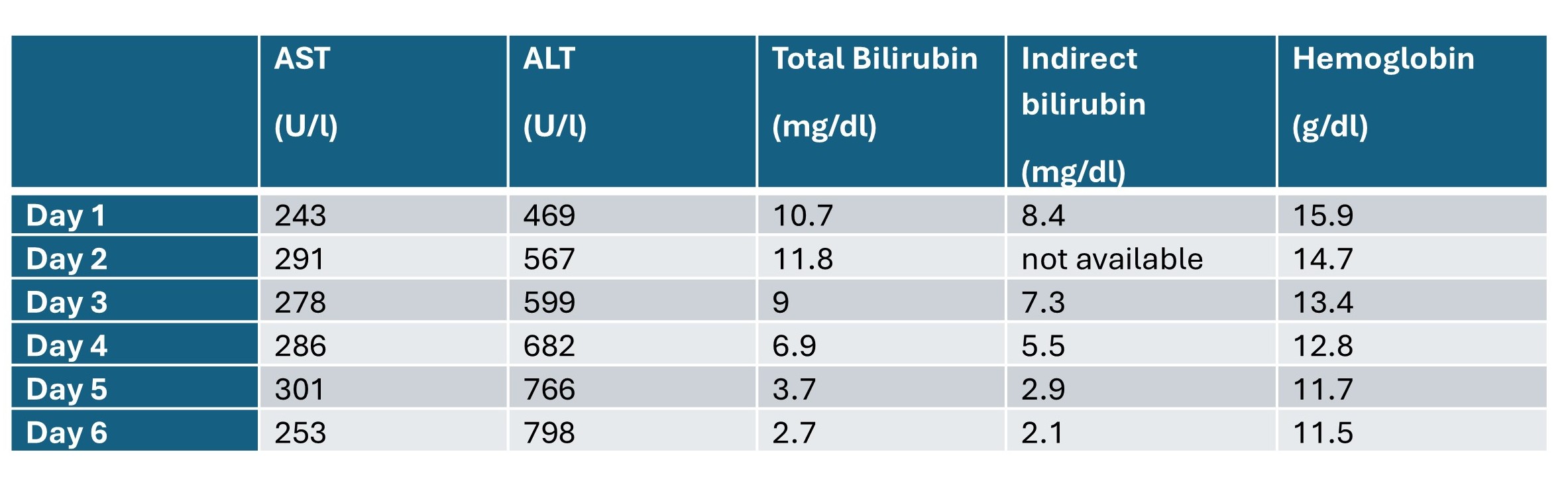
Figure: Table 1: Liver enzyme and hemoglobin trends over the course of hospitalization
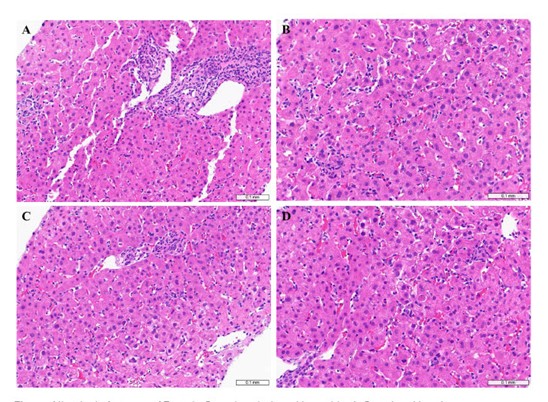
Figure: Figure 1: Histologic features of Epstein-Barr virus-induced hepatitis. A. Portal and locular lymphocytic inflammation. B. Sinusoidal lymphocytic infiltrates. C. Scattered mitotic figures. D. Rare acidophil bodies.
Disclosures:
Sargun Singh indicated no relevant financial relationships.
Yujie Zhang indicated no relevant financial relationships.
Vu Nguyen: AbbVie – Consultant, Speakers Bureau. Johnson & Johnson – Consultant, Speakers Bureau.
Sargun Singh, MBBS1, Yujie Zhang, MD, PhD2, Vu Nguyen, MD3. P6091 - Hemolytic Anemia and Hepatitis in the Setting of Acute Epstein-Barr Virus Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
