Tuesday Poster Session
Category: Liver
P6086 - A Diagnostic Challenge: Metastatic Melanoma Presenting as Acute Liver Injury With Gastrointestinal Involvement
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Danzhu Zhao, DO
University of Connecticut Health Center
Farmington, CT
Presenting Author(s)
Danzhu Zhao, DO1, Aaron Kahlam, MD2, Rishabh Sachdev, MD2
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut Health, Farmington, CT
Introduction: The fifth most common cancer in the United States, malignant melanoma, can frequently metastasize to the liver and the gastrointestinal (GI) tract. We present a case of a woman with a history of cutaneous melanoma who developed severe right upper quadrant abdominal pain and anorexia in association with an acute liver injury in the setting of biopsy proven metastatic melanoma.
Case Description/
Methods: A 55-year-old woman with diabetes, obesity, MASLD, cutaneous melanoma (stage 1B) status post wide local excision with negative sentinel lymph node biopsies in 9/2024 presented in late 4/2025 with ten days of worsening right upper quadrant pain, anorexia, and loose stools. Six months prior, a PET scan showed non-specific uptake without definitive evidence of recurrence. An ultrasound in 4/2025 showed innumerable hypodense hepatic lesions. A subsequent MRI revealed regenerative nodules.
On presentation, she was tachycardic with abdominal tenderness and guarding. Laboratory studies showed a predominantly cholestatic liver injury (Table 1). Lactate dehydrogenase (LDH) was elevated (4993 U/L). Alpha-fetoprotein and iron levels were normal. Infectious and autoimmune evaluation were unremarkable. CT angiogram was negative for mesenteric ischemia and notable for hepatosplenomegaly with hypodense splenic lesions.
Endoscopic (EGD) evaluation demonstrated an ulcerated melanotic nodule along the greater curvature of the gastric body and hyperpigmented spots in the duodenum (Figure 1). Biopsies showed foci of malignant melanoma. A percutaneous liver biopsy revealed metastatic malignant melanoma arising in a background of steatohepatitis. The patient declined further staging or treatment and transitioned to hospice, expiring two days later.
Discussion: Melanoma may metastasize to any organ including the liver and less commonly the GI tract, favoring the small intestine followed by the stomach and colon. Diagnosis of GI tract metastases may be challenging or delayed until autopsy given its nonspecific symptoms and ability to occur at any time. Distinguishing metastatic melanoma as a cause for ALI from other more common causes such as drug induced liver injury and viral hepatitis can be challenging, though LDH has been used as a marker of tumor involvement and a predictor of liver failure. In this case, frequent imaging and lab work in the months prior to presentation did not demonstrate evidence of recurrent or metastatic disease highlighting the complexity in establishing this diagnosis.
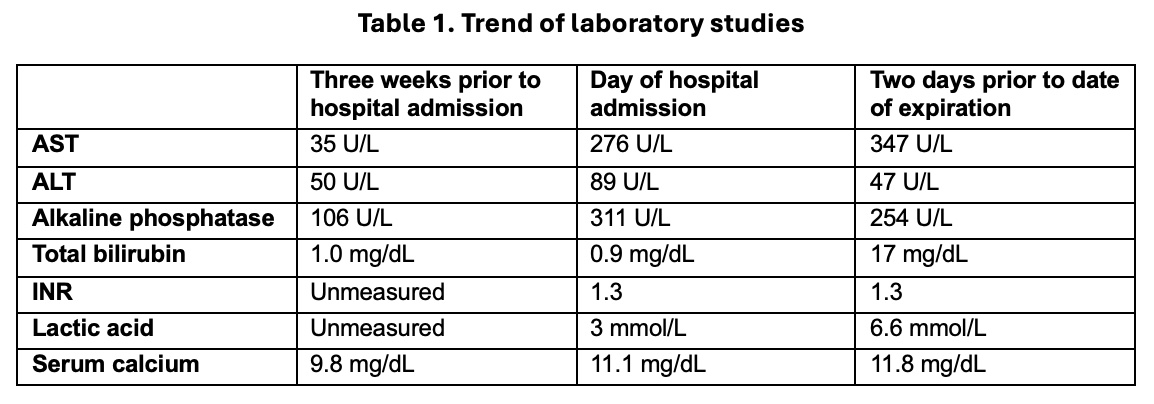
Figure: Table 1. Progression of laboratory studies from three weeks prior to this hospital admission to the day the patient transitioned to hospice care two days prior to her expiration, suggestive of ALI.
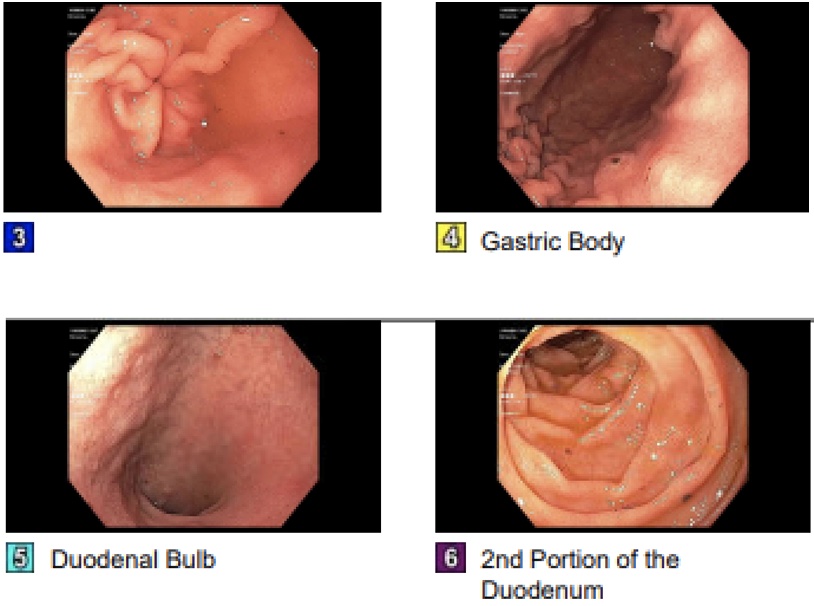
Figure: Figure 1. Melanotic ulcerated nodule along the greater curvature of the gastric body was seen on upper endoscopy. There was a normal appearing duodenum bulb. The 2nd portion of the duodenum revealed hyperpigmented melanotic spots.
Disclosures:
Danzhu Zhao indicated no relevant financial relationships.
Aaron Kahlam indicated no relevant financial relationships.
Rishabh Sachdev indicated no relevant financial relationships.
Danzhu Zhao, DO1, Aaron Kahlam, MD2, Rishabh Sachdev, MD2. P6086 - A Diagnostic Challenge: Metastatic Melanoma Presenting as Acute Liver Injury With Gastrointestinal Involvement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut Health, Farmington, CT
Introduction: The fifth most common cancer in the United States, malignant melanoma, can frequently metastasize to the liver and the gastrointestinal (GI) tract. We present a case of a woman with a history of cutaneous melanoma who developed severe right upper quadrant abdominal pain and anorexia in association with an acute liver injury in the setting of biopsy proven metastatic melanoma.
Case Description/
Methods: A 55-year-old woman with diabetes, obesity, MASLD, cutaneous melanoma (stage 1B) status post wide local excision with negative sentinel lymph node biopsies in 9/2024 presented in late 4/2025 with ten days of worsening right upper quadrant pain, anorexia, and loose stools. Six months prior, a PET scan showed non-specific uptake without definitive evidence of recurrence. An ultrasound in 4/2025 showed innumerable hypodense hepatic lesions. A subsequent MRI revealed regenerative nodules.
On presentation, she was tachycardic with abdominal tenderness and guarding. Laboratory studies showed a predominantly cholestatic liver injury (Table 1). Lactate dehydrogenase (LDH) was elevated (4993 U/L). Alpha-fetoprotein and iron levels were normal. Infectious and autoimmune evaluation were unremarkable. CT angiogram was negative for mesenteric ischemia and notable for hepatosplenomegaly with hypodense splenic lesions.
Endoscopic (EGD) evaluation demonstrated an ulcerated melanotic nodule along the greater curvature of the gastric body and hyperpigmented spots in the duodenum (Figure 1). Biopsies showed foci of malignant melanoma. A percutaneous liver biopsy revealed metastatic malignant melanoma arising in a background of steatohepatitis. The patient declined further staging or treatment and transitioned to hospice, expiring two days later.
Discussion: Melanoma may metastasize to any organ including the liver and less commonly the GI tract, favoring the small intestine followed by the stomach and colon. Diagnosis of GI tract metastases may be challenging or delayed until autopsy given its nonspecific symptoms and ability to occur at any time. Distinguishing metastatic melanoma as a cause for ALI from other more common causes such as drug induced liver injury and viral hepatitis can be challenging, though LDH has been used as a marker of tumor involvement and a predictor of liver failure. In this case, frequent imaging and lab work in the months prior to presentation did not demonstrate evidence of recurrent or metastatic disease highlighting the complexity in establishing this diagnosis.
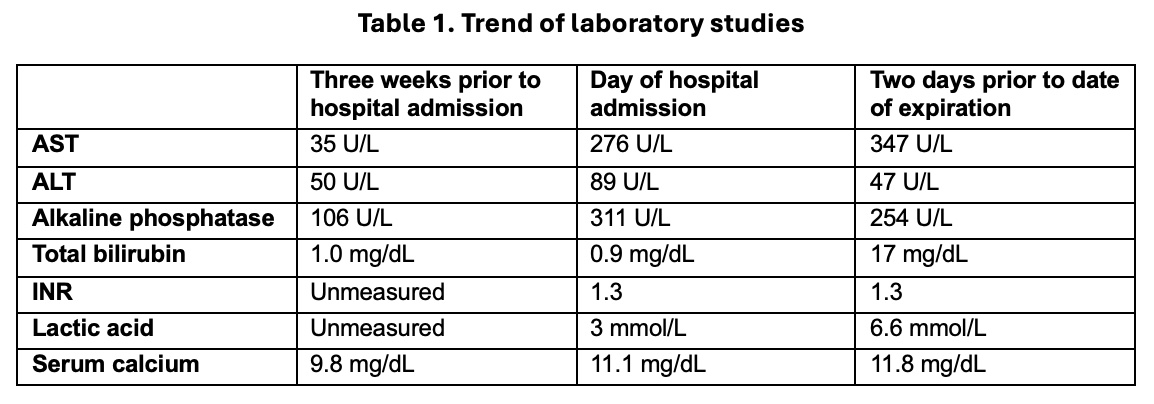
Figure: Table 1. Progression of laboratory studies from three weeks prior to this hospital admission to the day the patient transitioned to hospice care two days prior to her expiration, suggestive of ALI.
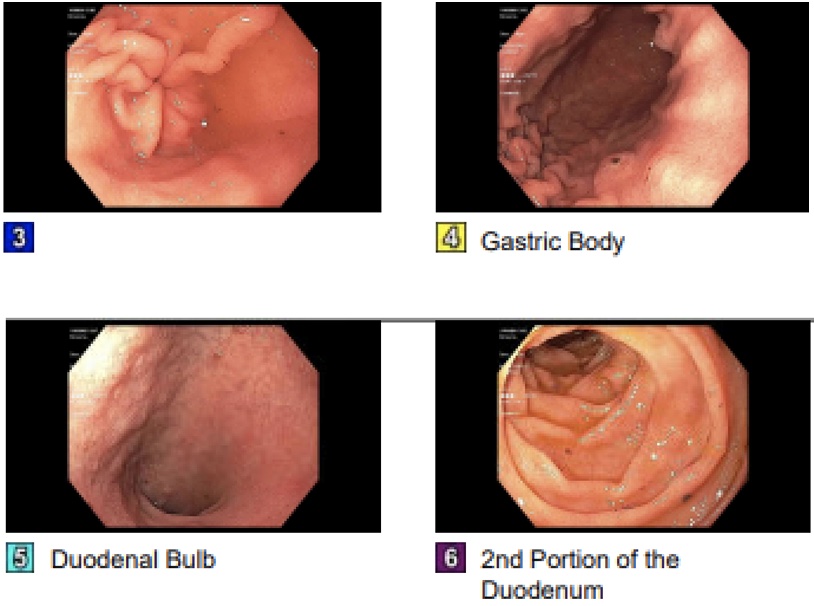
Figure: Figure 1. Melanotic ulcerated nodule along the greater curvature of the gastric body was seen on upper endoscopy. There was a normal appearing duodenum bulb. The 2nd portion of the duodenum revealed hyperpigmented melanotic spots.
Disclosures:
Danzhu Zhao indicated no relevant financial relationships.
Aaron Kahlam indicated no relevant financial relationships.
Rishabh Sachdev indicated no relevant financial relationships.
Danzhu Zhao, DO1, Aaron Kahlam, MD2, Rishabh Sachdev, MD2. P6086 - A Diagnostic Challenge: Metastatic Melanoma Presenting as Acute Liver Injury With Gastrointestinal Involvement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
