Tuesday Poster Session
Category: Liver
P6078 - Hepatic Neuroendocrine Tumors: Searching for the Source
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- HA
Hassan Abidali, BS
Midwestern University Arizona College of Osteopathic Medicine
Glendale, AZ
Presenting Author(s)
Hassan Abidali, BS1, Ahmed Abidali, DO2, Samier Deen, DO3, Harneet Grewal, MD4, Ava M. Koehler De Celaya, BS5, Khushbir Bath, MD6
1Midwestern University Arizona College of Osteopathic Medicine, Glendale, AZ; 2Larkin Community Hospital, Glendale, AZ; 3HonorHealth, Scottsdale, AZ; 4Abrazo Health Network, Glendale, AZ; 5University of Arizona College of Medicine, Phoenix, AZ; 6Arrowhead Gastroenterology Associates, Phoenix, AZ
Introduction: Neuroendocrine tumor (NET) are a rare disease entity with a growing incidence that predominantly originates in the GI tract. During the early disease course, NETs are commonly asymptomatic, attributed to the liver's ability to deactivate hormones secreted by the tumors. Symptoms such as flushing and diarrhea often only manifest after hepatic metastasis, leading to a significant number of patients being diagnosed with advanced disease. Targeted treatment requires early identification of the primary source and often includes resection with curative intent.
Case Description/
Methods: In this case, we describe a 28-year-old male who presented with a 3-day history of presyncope, nausea, vomiting, epigastric abdominal pain as well as acute on chronic diarrhea and 35 lb. unintentional weight loss over the past year. On initial presentation, the patient was hemodynamically stable with unremarkable physical exam and normal CBC/CMP. US abdomen revealed innumerable hypoechoic liver nodules. MR abdomen revealed numerous masses in both hepatic lobes measuring from 0.2-2.3 cm with areas of central necrosis. Metastatic surveillance included CT chest, which revealed a solitary 6 mm nodule with central calcification; however, MRI brain and US scrotum were unrevealing. Further work-up included CA 19-9, AFP, CEA, b-hCG, TB Gold, Hepatitis A/B/C, which were negative and/or within normal limits. Liver biopsy on histopathology showed WHO Grade 1 NET with Ki-67 < 1%, p53 negative, strong synaptophysin and chromogranin positivity, and CDX-2 staining suggestive of GI or pancreatic origin. Outpatient GI evaluation included bidirectional endoscopy, which was unrevealing. Outpatient oncology evaluation with [68Ga]DOTATATE PET/CT showed pelvic and sacral uptake consistent with somatostatin receptor 2–expressing lesions, concerning for small bowel origin. Currently, the patient is being treated with Lanreotide and is pending further evaluation with colorectal surgery.
Discussion: Hepatic NETs are most commonly of metastatic origin; however, a careful and comprehensive evaluation should prioritize identification of the primary source. In the case of hepatic metastasis, thorough assessment of the GI tract is warranted, particularly of the small bowel, which represents the most likely origin. Close attention to the unique and characteristic symptoms of NETs, such as flushing and diarrhea, should prompt early clinical suspicion given the climbing disease incidence and high associated mortality.

Figure: CT with contrast revealing multiple nodules involving all lobes of the liver
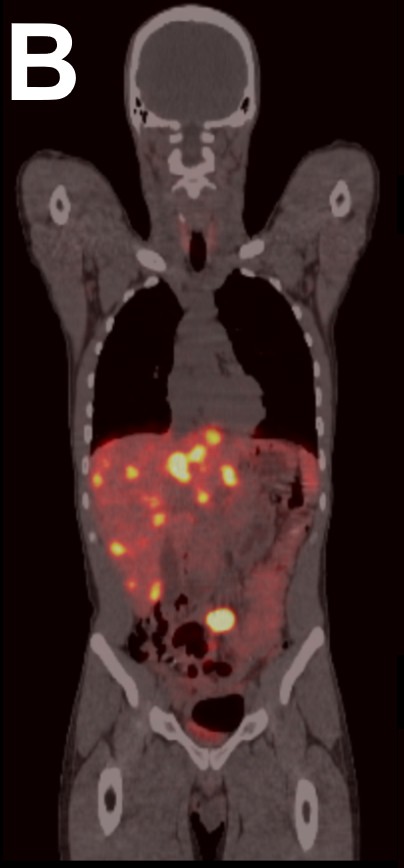
Figure: [68Ga]DOTATATE PET/CT demonstrating uptake in the liver and lower abdomen compatible with lesions with marked increase expression of somatostatin receptor 2
Disclosures:
Hassan Abidali indicated no relevant financial relationships.
Ahmed Abidali indicated no relevant financial relationships.
Samier Deen indicated no relevant financial relationships.
Harneet Grewal indicated no relevant financial relationships.
Ava Koehler De Celaya indicated no relevant financial relationships.
Khushbir Bath indicated no relevant financial relationships.
Hassan Abidali, BS1, Ahmed Abidali, DO2, Samier Deen, DO3, Harneet Grewal, MD4, Ava M. Koehler De Celaya, BS5, Khushbir Bath, MD6. P6078 - Hepatic Neuroendocrine Tumors: Searching for the Source, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Midwestern University Arizona College of Osteopathic Medicine, Glendale, AZ; 2Larkin Community Hospital, Glendale, AZ; 3HonorHealth, Scottsdale, AZ; 4Abrazo Health Network, Glendale, AZ; 5University of Arizona College of Medicine, Phoenix, AZ; 6Arrowhead Gastroenterology Associates, Phoenix, AZ
Introduction: Neuroendocrine tumor (NET) are a rare disease entity with a growing incidence that predominantly originates in the GI tract. During the early disease course, NETs are commonly asymptomatic, attributed to the liver's ability to deactivate hormones secreted by the tumors. Symptoms such as flushing and diarrhea often only manifest after hepatic metastasis, leading to a significant number of patients being diagnosed with advanced disease. Targeted treatment requires early identification of the primary source and often includes resection with curative intent.
Case Description/
Methods: In this case, we describe a 28-year-old male who presented with a 3-day history of presyncope, nausea, vomiting, epigastric abdominal pain as well as acute on chronic diarrhea and 35 lb. unintentional weight loss over the past year. On initial presentation, the patient was hemodynamically stable with unremarkable physical exam and normal CBC/CMP. US abdomen revealed innumerable hypoechoic liver nodules. MR abdomen revealed numerous masses in both hepatic lobes measuring from 0.2-2.3 cm with areas of central necrosis. Metastatic surveillance included CT chest, which revealed a solitary 6 mm nodule with central calcification; however, MRI brain and US scrotum were unrevealing. Further work-up included CA 19-9, AFP, CEA, b-hCG, TB Gold, Hepatitis A/B/C, which were negative and/or within normal limits. Liver biopsy on histopathology showed WHO Grade 1 NET with Ki-67 < 1%, p53 negative, strong synaptophysin and chromogranin positivity, and CDX-2 staining suggestive of GI or pancreatic origin. Outpatient GI evaluation included bidirectional endoscopy, which was unrevealing. Outpatient oncology evaluation with [68Ga]DOTATATE PET/CT showed pelvic and sacral uptake consistent with somatostatin receptor 2–expressing lesions, concerning for small bowel origin. Currently, the patient is being treated with Lanreotide and is pending further evaluation with colorectal surgery.
Discussion: Hepatic NETs are most commonly of metastatic origin; however, a careful and comprehensive evaluation should prioritize identification of the primary source. In the case of hepatic metastasis, thorough assessment of the GI tract is warranted, particularly of the small bowel, which represents the most likely origin. Close attention to the unique and characteristic symptoms of NETs, such as flushing and diarrhea, should prompt early clinical suspicion given the climbing disease incidence and high associated mortality.

Figure: CT with contrast revealing multiple nodules involving all lobes of the liver
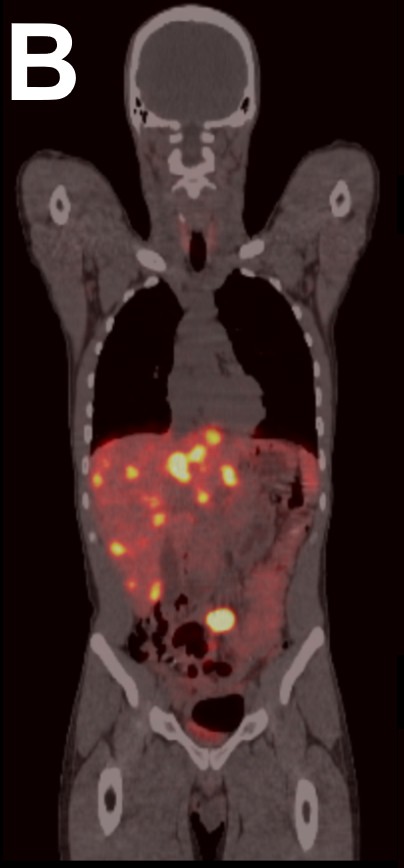
Figure: [68Ga]DOTATATE PET/CT demonstrating uptake in the liver and lower abdomen compatible with lesions with marked increase expression of somatostatin receptor 2
Disclosures:
Hassan Abidali indicated no relevant financial relationships.
Ahmed Abidali indicated no relevant financial relationships.
Samier Deen indicated no relevant financial relationships.
Harneet Grewal indicated no relevant financial relationships.
Ava Koehler De Celaya indicated no relevant financial relationships.
Khushbir Bath indicated no relevant financial relationships.
Hassan Abidali, BS1, Ahmed Abidali, DO2, Samier Deen, DO3, Harneet Grewal, MD4, Ava M. Koehler De Celaya, BS5, Khushbir Bath, MD6. P6078 - Hepatic Neuroendocrine Tumors: Searching for the Source, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
