Tuesday Poster Session
Category: Liver
P6074 - Suspected Glycogen Storage Disease in a Young Adult With Cryptogenic Cirrhosis: A Case Report
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Vishnu Yanamaladoddi, MD
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
Vishnu Yanamaladoddi, MD1, Jazza Jamil, MBBS2, Brianna A. Werner, 1, Pir Shah, MD1, Mohanad Al-Qaisi, MD1, Nilofar Najafian, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2Northwest School of Medicine, Phoenix, AZ
Introduction: Glycogen storage diseases (GSD) are inherited metabolic disorders of carbohydrate metabolism. GSD type III (Cori’s disease) and type IV (Andersen’s disease) have been associated with liver cirrhosis and hepatocellular carcinoma. We describe a rare case of GSD and cirrhosis in a patient with a history of childhood seizures and hypoglycemia.
Case Description/
Methods: A 38-year-old male without known medical history presented with intermittent hematochezia without abdominal pain, weight loss, or fever. He was hemodynamically stable with an unremarkable exam. Labs showed hemoglobin 13.8 g/dL, platelets 64,000/uL, INR 1.3, ALT 158 U/L, AST 260 U/L. Alkaline phosphatase and GGT were minimally elevated. C-reactive protein was 75.8 mg/dL. CT showed cirrhosis, portal hypertension, and splenomegaly. He denied herbal supplements, IV drug, or heavy alcohol use. Family history was non-contributory.
Abdominal MRI revealed multiple enhancing liver lesions not seen on CT one week prior, suggesting rapid development. Upper endoscopy showed large esophageal varices and portal hypertensive gastropathy. Colonoscopy showed mild portal colopathy and hemorrhoids. Workup for chronic liver disease was negative, including viral hepatitis, autoimmune markers, iron/copper studies, and tumor markers. Biopsy of the largest lesion and background tissue showed cirrhosis with ballooning degeneration, clear cell change, and glycogenated hepatocytes. PAS staining without diastase confirmed glycogen accumulation. No malignancy, steatosis, or iron/copper overload was seen.
In absence of classic risk factors and unusual histology, rare causes of cirrhosis were considered. A family member later recalled childhood hypoglycemia and seizures, which had resolved without diagnosis. These, along with imaging and biopsy findings, raised suspicion for late-presenting GSD. Repeat MRI at three months showed complete resolution of the liver lesions, suggesting a metabolic rather than neoplastic process. Genetic testing was initiated for confirmation.
Discussion: This case illustrates an atypical presentation of cryptogenic cirrhosis and portal hypertension in a young adult with suspected GSD. The spontaneous resolution of liver lesions, glycogenated hepatocytes, and childhood hypoglycemia support a metabolic etiology. GSD should be considered in unexplained liver disease, even in adults. Early recognition using detailed history and genetic testing is essential for management and counseling.
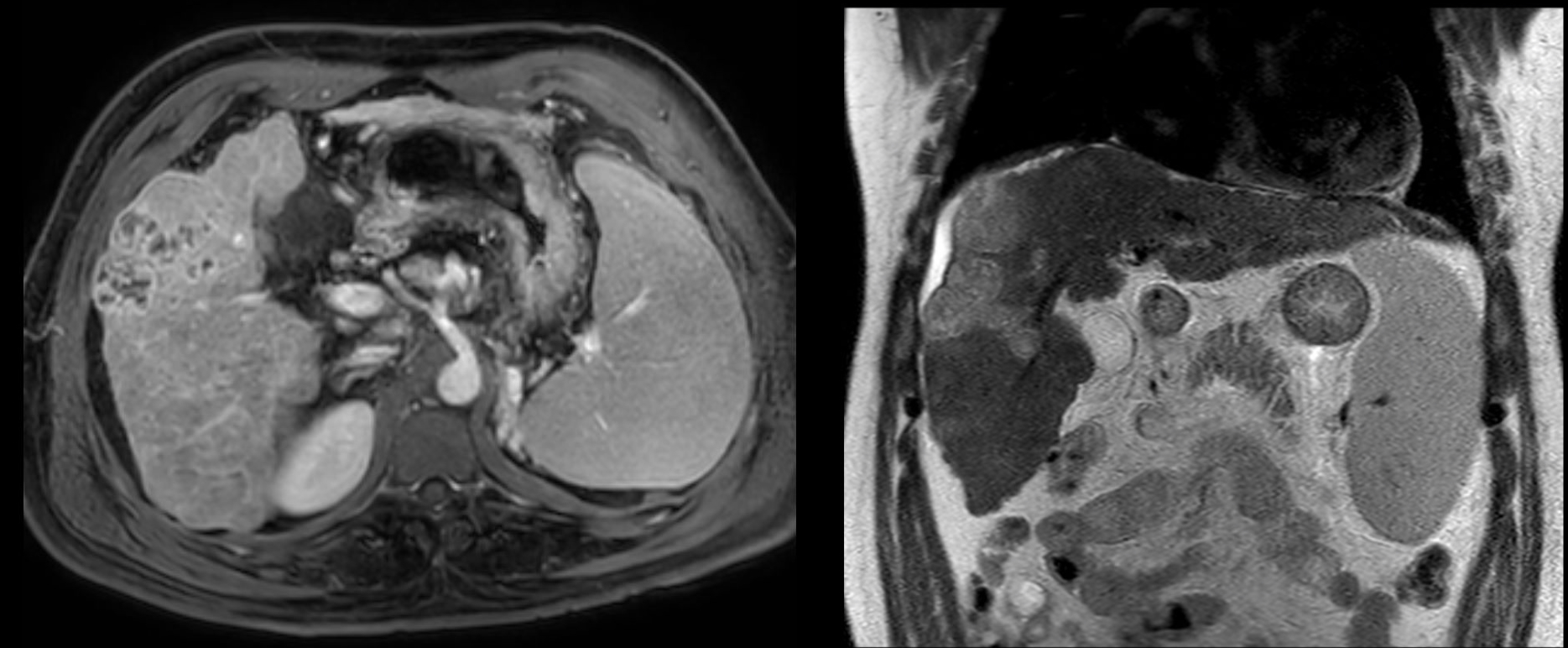
Figure: MRI abdomen at presentation showing cirrhosis and enhancing liver lesions

Figure: MRI at 3-month follow up showing interval resolution of the scattered heterogeneously enhancing liver lesions
Disclosures:
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Jazza Jamil indicated no relevant financial relationships.
Brianna Werner indicated no relevant financial relationships.
Pir Shah indicated no relevant financial relationships.
Mohanad Al-Qaisi indicated no relevant financial relationships.
Nilofar Najafian indicated no relevant financial relationships.
Vishnu Yanamaladoddi, MD1, Jazza Jamil, MBBS2, Brianna A. Werner, 1, Pir Shah, MD1, Mohanad Al-Qaisi, MD1, Nilofar Najafian, MD1. P6074 - Suspected Glycogen Storage Disease in a Young Adult With Cryptogenic Cirrhosis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University School of Medicine, Phoenix, AZ; 2Northwest School of Medicine, Phoenix, AZ
Introduction: Glycogen storage diseases (GSD) are inherited metabolic disorders of carbohydrate metabolism. GSD type III (Cori’s disease) and type IV (Andersen’s disease) have been associated with liver cirrhosis and hepatocellular carcinoma. We describe a rare case of GSD and cirrhosis in a patient with a history of childhood seizures and hypoglycemia.
Case Description/
Methods: A 38-year-old male without known medical history presented with intermittent hematochezia without abdominal pain, weight loss, or fever. He was hemodynamically stable with an unremarkable exam. Labs showed hemoglobin 13.8 g/dL, platelets 64,000/uL, INR 1.3, ALT 158 U/L, AST 260 U/L. Alkaline phosphatase and GGT were minimally elevated. C-reactive protein was 75.8 mg/dL. CT showed cirrhosis, portal hypertension, and splenomegaly. He denied herbal supplements, IV drug, or heavy alcohol use. Family history was non-contributory.
Abdominal MRI revealed multiple enhancing liver lesions not seen on CT one week prior, suggesting rapid development. Upper endoscopy showed large esophageal varices and portal hypertensive gastropathy. Colonoscopy showed mild portal colopathy and hemorrhoids. Workup for chronic liver disease was negative, including viral hepatitis, autoimmune markers, iron/copper studies, and tumor markers. Biopsy of the largest lesion and background tissue showed cirrhosis with ballooning degeneration, clear cell change, and glycogenated hepatocytes. PAS staining without diastase confirmed glycogen accumulation. No malignancy, steatosis, or iron/copper overload was seen.
In absence of classic risk factors and unusual histology, rare causes of cirrhosis were considered. A family member later recalled childhood hypoglycemia and seizures, which had resolved without diagnosis. These, along with imaging and biopsy findings, raised suspicion for late-presenting GSD. Repeat MRI at three months showed complete resolution of the liver lesions, suggesting a metabolic rather than neoplastic process. Genetic testing was initiated for confirmation.
Discussion: This case illustrates an atypical presentation of cryptogenic cirrhosis and portal hypertension in a young adult with suspected GSD. The spontaneous resolution of liver lesions, glycogenated hepatocytes, and childhood hypoglycemia support a metabolic etiology. GSD should be considered in unexplained liver disease, even in adults. Early recognition using detailed history and genetic testing is essential for management and counseling.
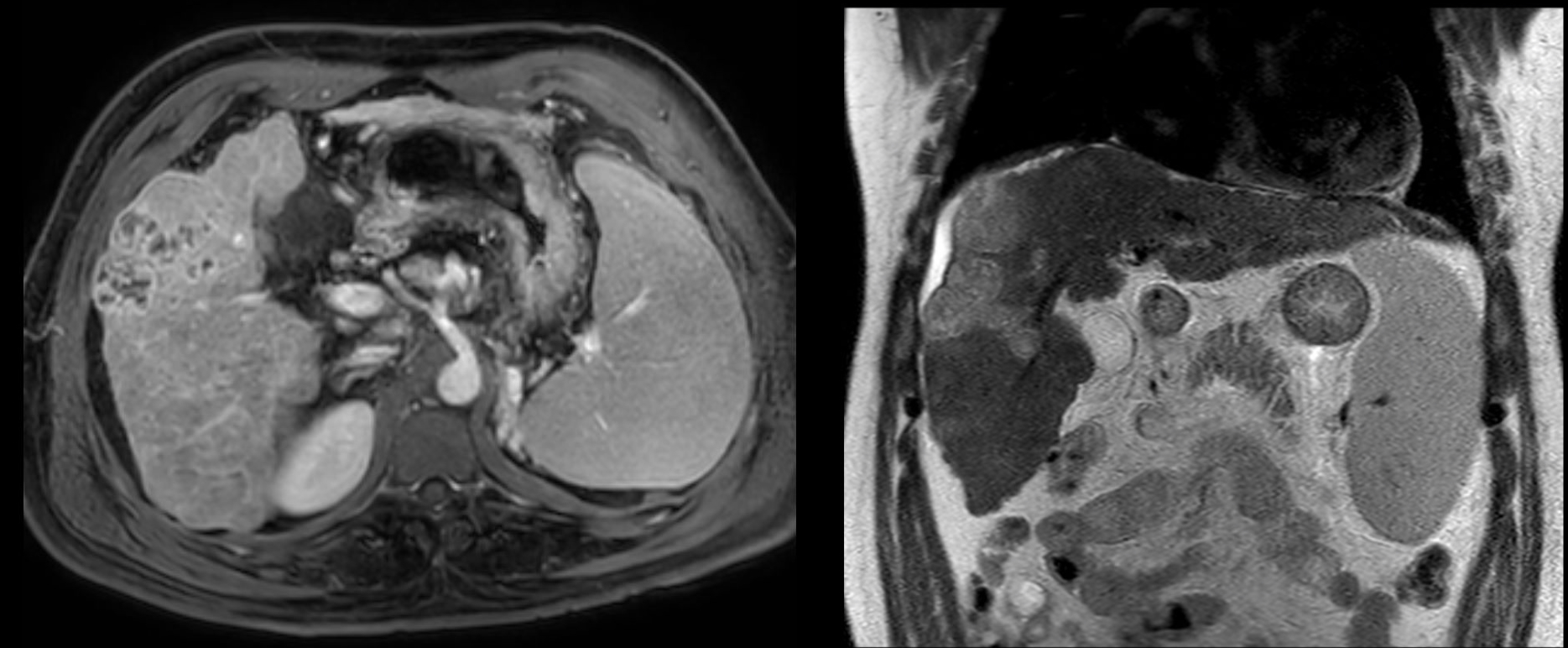
Figure: MRI abdomen at presentation showing cirrhosis and enhancing liver lesions

Figure: MRI at 3-month follow up showing interval resolution of the scattered heterogeneously enhancing liver lesions
Disclosures:
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Jazza Jamil indicated no relevant financial relationships.
Brianna Werner indicated no relevant financial relationships.
Pir Shah indicated no relevant financial relationships.
Mohanad Al-Qaisi indicated no relevant financial relationships.
Nilofar Najafian indicated no relevant financial relationships.
Vishnu Yanamaladoddi, MD1, Jazza Jamil, MBBS2, Brianna A. Werner, 1, Pir Shah, MD1, Mohanad Al-Qaisi, MD1, Nilofar Najafian, MD1. P6074 - Suspected Glycogen Storage Disease in a Young Adult With Cryptogenic Cirrhosis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
