Tuesday Poster Session
Category: Liver
Peliosis Hepatitis Secondary to <i>Bartonella Henselae</i> Infection
P6023 - Peliosis Hepatitis Secondary to Bartonella Henselae Infection
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Blake Flores Semyonov, DO
HCA Florida Largo Hospital
Nashville, TN
Presenting Author(s)
Blake Flores Semyonov, DO1, Anabel Rodriguez Loya, DO2, Roxana Bodin, MD2
1HCA Florida Largo Hospital, Pinellas Park, FL; 2HCA Florida Largo Hospital, Largo, FL
Introduction: Peliosis hepatis is a rare vascular condition characterized by blood-filled cystic spaces in the liver, often associated with underlying infections, malignancies, or immunosuppression. Bartonella henselae, the causative agent of cat scratch disease, is a known but uncommon cause. Most reported cases occur in immunocompromised individuals, particularly those with HIV/AIDS.
Case Description/
Methods: A 27-year-old male with multiple prior hospitalizations presented with abdominal pain, weight loss, ascites, and fatigue. He denied alcohol use, recent travel, or medication exposure but reported owning three cats. Laboratory evaluation revealed acute kidney injury, nephrotic-range proteinuria, pancytopenia, elevated alkaline phosphatase, and a mildly elevated erythrocyte sedimentation rate. HIV and tuberculosis testing were negative. Ascitic fluid analysis showed high protein content and a low serum-ascites albumin gradient (SAAG < 1.1), ruling out portal hypertension. Cytology was negative for malignancy. Abdominal MRI demonstrated multiple arterial-enhancing hepatic lesions without cirrhosis. Esophagogastroduodenoscopy and colonoscopy revealed no abnormalities. Bone marrow biopsy and flow cytometry excluded acute leukemia, high-grade myelodysplasia, plasma cell disorders, and lymphoproliferative disease. Diagnostic laparoscopy with peritoneal biopsies was negative for malignancy or amyloidosis, showing only nonspecific chronic inflammation. A liver biopsy revealed features consistent with peliosis hepatis. Warthin-Starry staining and serologic testing confirmed Bartonella henselae infection. The patient was treated with a 3-month course of doxycycline, leading to resolution of hepatic lesions, normalization of renal function, correction of cytopenias, and complete resolution of ascites.
Discussion: In this case, the absence of common risk factors such as immunosuppression or HIV infection obscured the diagnosis. The patient’s systemic findings including cytopenias, renal dysfunction, ascites, and radiographically atypical liver lesions mimicked malignancy or infiltrative disease, leading to extensive workup. This case highlights the importance of considering infectious etiologies, including Bartonella henselae, in patients with multisystem involvement and unexplained hepatic lesions, regardless of immune status. Early recognition is critical, as antimicrobial therapy can lead to complete resolution and prevent unnecessary invasive interventions.
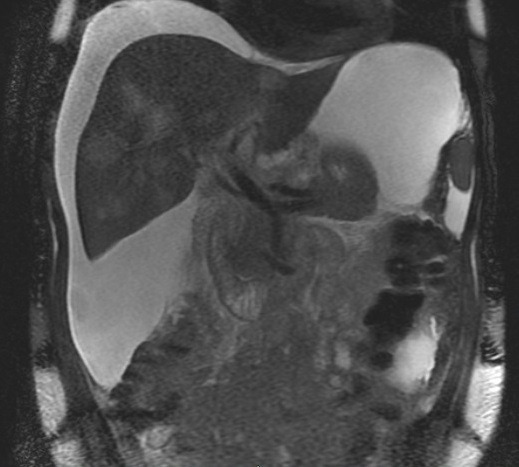
Figure: Peliosis Hepatitis from Bartonella Henslae
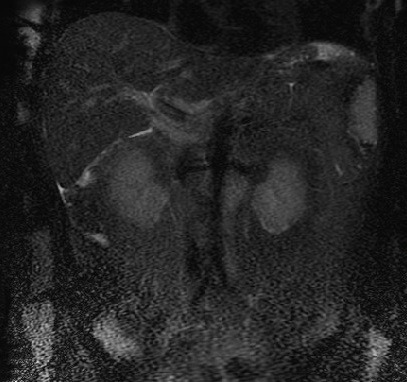
Figure: Resolved Hepatic Lesions
Disclosures:
Blake Flores Semyonov indicated no relevant financial relationships.
Anabel Rodriguez Loya indicated no relevant financial relationships.
Roxana Bodin indicated no relevant financial relationships.
Blake Flores Semyonov, DO1, Anabel Rodriguez Loya, DO2, Roxana Bodin, MD2. P6023 - Peliosis Hepatitis Secondary to <i>Bartonella Henselae</i> Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HCA Florida Largo Hospital, Pinellas Park, FL; 2HCA Florida Largo Hospital, Largo, FL
Introduction: Peliosis hepatis is a rare vascular condition characterized by blood-filled cystic spaces in the liver, often associated with underlying infections, malignancies, or immunosuppression. Bartonella henselae, the causative agent of cat scratch disease, is a known but uncommon cause. Most reported cases occur in immunocompromised individuals, particularly those with HIV/AIDS.
Case Description/
Methods: A 27-year-old male with multiple prior hospitalizations presented with abdominal pain, weight loss, ascites, and fatigue. He denied alcohol use, recent travel, or medication exposure but reported owning three cats. Laboratory evaluation revealed acute kidney injury, nephrotic-range proteinuria, pancytopenia, elevated alkaline phosphatase, and a mildly elevated erythrocyte sedimentation rate. HIV and tuberculosis testing were negative. Ascitic fluid analysis showed high protein content and a low serum-ascites albumin gradient (SAAG < 1.1), ruling out portal hypertension. Cytology was negative for malignancy. Abdominal MRI demonstrated multiple arterial-enhancing hepatic lesions without cirrhosis. Esophagogastroduodenoscopy and colonoscopy revealed no abnormalities. Bone marrow biopsy and flow cytometry excluded acute leukemia, high-grade myelodysplasia, plasma cell disorders, and lymphoproliferative disease. Diagnostic laparoscopy with peritoneal biopsies was negative for malignancy or amyloidosis, showing only nonspecific chronic inflammation. A liver biopsy revealed features consistent with peliosis hepatis. Warthin-Starry staining and serologic testing confirmed Bartonella henselae infection. The patient was treated with a 3-month course of doxycycline, leading to resolution of hepatic lesions, normalization of renal function, correction of cytopenias, and complete resolution of ascites.
Discussion: In this case, the absence of common risk factors such as immunosuppression or HIV infection obscured the diagnosis. The patient’s systemic findings including cytopenias, renal dysfunction, ascites, and radiographically atypical liver lesions mimicked malignancy or infiltrative disease, leading to extensive workup. This case highlights the importance of considering infectious etiologies, including Bartonella henselae, in patients with multisystem involvement and unexplained hepatic lesions, regardless of immune status. Early recognition is critical, as antimicrobial therapy can lead to complete resolution and prevent unnecessary invasive interventions.
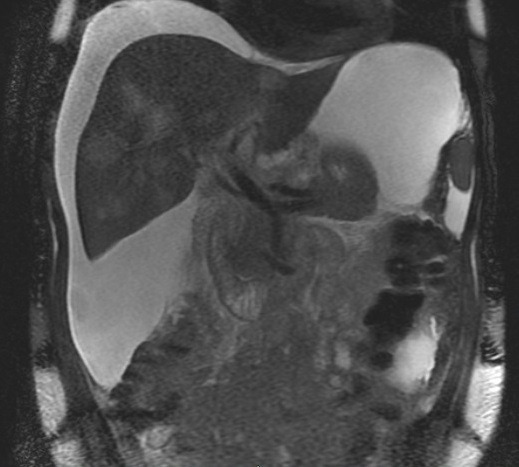
Figure: Peliosis Hepatitis from Bartonella Henslae
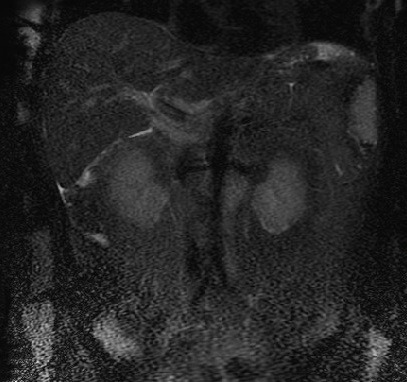
Figure: Resolved Hepatic Lesions
Disclosures:
Blake Flores Semyonov indicated no relevant financial relationships.
Anabel Rodriguez Loya indicated no relevant financial relationships.
Roxana Bodin indicated no relevant financial relationships.
Blake Flores Semyonov, DO1, Anabel Rodriguez Loya, DO2, Roxana Bodin, MD2. P6023 - Peliosis Hepatitis Secondary to <i>Bartonella Henselae</i> Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
