Tuesday Poster Session
Category: Liver
P6012 - Gut Feeling: Acute Colitis Unmasks a Silent Portosystemic Shunt
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- GS
Gevork Salmastyan, MD
Keck School of Medicine of the University of Southern California
Los Angeles, CA
Presenting Author(s)
Gevork Salmastyan, MD, Michael Sullivan, BS, Madeline Garcia, BS, Sean Dewberry, MD, Michael Repajic, MD, Lucas Tsikita, MD, Jeffrey Kahn, MD
Keck School of Medicine of the University of Southern California, Los Angeles, CA
Introduction: Portosystemic shunts (PSS) are abnormal vascular connections between the portal and systemic circulations that divert blood away from hepatic metabolism. These shunts may be congenital, acquired from portal hypertension, or iatrogenic. We present a rare case of a patient with a congenital intrahepatic PSS between the right portal and hepatic veins who developed severe portosystemic encephalopathy, likely triggered by acute colitis.
Case Description/
Methods: A 63-year-old female with a history of diabetes, hepatic steatosis, and subclinical hypothyroidism presented with sudden-onset confusion and black stools. Her family reported a brief episode of emesis followed by progressive disorientation. Upon arrival, she passed approximately 200cc of melena, developed worsening encephalopathy, and required intubation for airway protection. Laboratory evaluation revealed a serum ammonia of 226 µmol/L, normal liver chemistries, platelets of 250 K/μL, and no coagulopathy. Cross-sectional CT demonstrated acute sigmoid diverticulitis with adjacent phlegmon and a large congenital portosystemic shunt between the right portal and hepatic veins. Five abnormal portovenous connections were seen across both hepatic lobes, consistent with a type 4 congenital shunt. EGD revealed mild gastric oozing but no varices or other stigmata of portal hypertension-related bleeding. The patient was managed with lactulose and rifaximin via nasogastric tube, resulting in rapid ammonia level normalization by hospital day 3. Her mental status fully recovered by day 5 and she was discharged home in stable condition later that week. She is currently undergoing evaluation for potential shunt closure.
Discussion: PSS can be asymptomatic or present with encephalopathy or liver dysfunction, depending on anatomy and shunt ratio. Unlike cirrhosis, PSS typically leads to portosystemic encephalopathy without portal hypertension. This case illustrates how acute colitis can unmask a silent shunt by abruptly increasing splanchnic flow and ammonia load beyond hepatic clearance. While shunt anatomy determines baseline risk, transient inflammation can precipitate encephalopathy even with normal liver function.
Initial management targets reversible triggers and ammonia reduction. However, patients with recurrent or refractory symptoms may require shunt closure via embolization or surgery to restore hepatopetal flow and reduce hyperammonemia. Early recognition and treatment can lead to full recovery and may obviate the need for intervention.
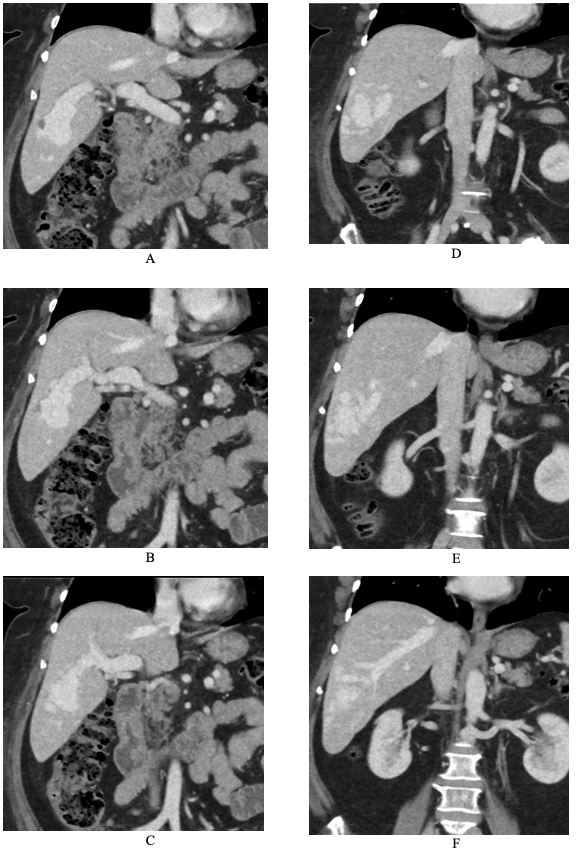
Figure: Figure 1. Coronal contrast-enhanced CT of the liver demonstrating an intrahepatic portosystemic shunt. Panels A–C show sequential images of the right portal vein (RPV) coursing toward and draining into the right hepatic vein (RHV): Panel A displays the RPV branching toward the hepatic vein; Panel B shows further progression toward hepatic outflow; Panel C depicts the RPV entering the RHV. Panels D–F illustrate the reverse trajectory: Panel D shows the confluence of the RPV and RHV within the liver; Panel E highlights the RHV extending toward the RPV; and Panel F captures an inferior intrahepatic communication between the two vessels.
Disclosures:
Gevork Salmastyan indicated no relevant financial relationships.
Michael Sullivan indicated no relevant financial relationships.
Madeline Garcia indicated no relevant financial relationships.
Sean Dewberry indicated no relevant financial relationships.
Michael Repajic indicated no relevant financial relationships.
Lucas Tsikita indicated no relevant financial relationships.
Jeffrey Kahn indicated no relevant financial relationships.
Gevork Salmastyan, MD, Michael Sullivan, BS, Madeline Garcia, BS, Sean Dewberry, MD, Michael Repajic, MD, Lucas Tsikita, MD, Jeffrey Kahn, MD. P6012 - Gut Feeling: Acute Colitis Unmasks a Silent Portosystemic Shunt, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Keck School of Medicine of the University of Southern California, Los Angeles, CA
Introduction: Portosystemic shunts (PSS) are abnormal vascular connections between the portal and systemic circulations that divert blood away from hepatic metabolism. These shunts may be congenital, acquired from portal hypertension, or iatrogenic. We present a rare case of a patient with a congenital intrahepatic PSS between the right portal and hepatic veins who developed severe portosystemic encephalopathy, likely triggered by acute colitis.
Case Description/
Methods: A 63-year-old female with a history of diabetes, hepatic steatosis, and subclinical hypothyroidism presented with sudden-onset confusion and black stools. Her family reported a brief episode of emesis followed by progressive disorientation. Upon arrival, she passed approximately 200cc of melena, developed worsening encephalopathy, and required intubation for airway protection. Laboratory evaluation revealed a serum ammonia of 226 µmol/L, normal liver chemistries, platelets of 250 K/μL, and no coagulopathy. Cross-sectional CT demonstrated acute sigmoid diverticulitis with adjacent phlegmon and a large congenital portosystemic shunt between the right portal and hepatic veins. Five abnormal portovenous connections were seen across both hepatic lobes, consistent with a type 4 congenital shunt. EGD revealed mild gastric oozing but no varices or other stigmata of portal hypertension-related bleeding. The patient was managed with lactulose and rifaximin via nasogastric tube, resulting in rapid ammonia level normalization by hospital day 3. Her mental status fully recovered by day 5 and she was discharged home in stable condition later that week. She is currently undergoing evaluation for potential shunt closure.
Discussion: PSS can be asymptomatic or present with encephalopathy or liver dysfunction, depending on anatomy and shunt ratio. Unlike cirrhosis, PSS typically leads to portosystemic encephalopathy without portal hypertension. This case illustrates how acute colitis can unmask a silent shunt by abruptly increasing splanchnic flow and ammonia load beyond hepatic clearance. While shunt anatomy determines baseline risk, transient inflammation can precipitate encephalopathy even with normal liver function.
Initial management targets reversible triggers and ammonia reduction. However, patients with recurrent or refractory symptoms may require shunt closure via embolization or surgery to restore hepatopetal flow and reduce hyperammonemia. Early recognition and treatment can lead to full recovery and may obviate the need for intervention.
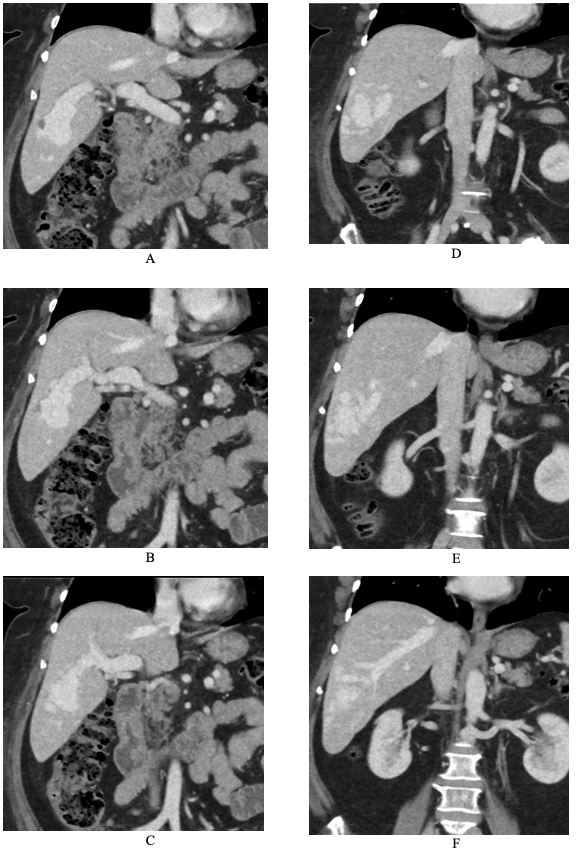
Figure: Figure 1. Coronal contrast-enhanced CT of the liver demonstrating an intrahepatic portosystemic shunt. Panels A–C show sequential images of the right portal vein (RPV) coursing toward and draining into the right hepatic vein (RHV): Panel A displays the RPV branching toward the hepatic vein; Panel B shows further progression toward hepatic outflow; Panel C depicts the RPV entering the RHV. Panels D–F illustrate the reverse trajectory: Panel D shows the confluence of the RPV and RHV within the liver; Panel E highlights the RHV extending toward the RPV; and Panel F captures an inferior intrahepatic communication between the two vessels.
Disclosures:
Gevork Salmastyan indicated no relevant financial relationships.
Michael Sullivan indicated no relevant financial relationships.
Madeline Garcia indicated no relevant financial relationships.
Sean Dewberry indicated no relevant financial relationships.
Michael Repajic indicated no relevant financial relationships.
Lucas Tsikita indicated no relevant financial relationships.
Jeffrey Kahn indicated no relevant financial relationships.
Gevork Salmastyan, MD, Michael Sullivan, BS, Madeline Garcia, BS, Sean Dewberry, MD, Michael Repajic, MD, Lucas Tsikita, MD, Jeffrey Kahn, MD. P6012 - Gut Feeling: Acute Colitis Unmasks a Silent Portosystemic Shunt, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
