Tuesday Poster Session
Category: Liver
P5999 - A Triple Threat to the Liver: Coexisting MASH, Autoimmune Hepatitis, and Alpha-1 Antitrypsin Deficiency in a Single Patient
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Gopala Konduri, MD (he/him/his)
University of Missouri
Columbia, MO
Presenting Author(s)
Gopala Konduri, MD1, Muhammad Yousaf, MD2, Austin Reed, DO3, Ahmad Ali, MD1, Hanna Nale, DO4, Deepthi Rao, MD1, Sravya Ponnapalli, MD5
1University of Missouri, Columbia, MO; 2University of Missouri Health Care, Columbia, MO; 3Sunrise Health GME Consortium, Las Vegas, NV; 4University of Missouri School of Medicine, Columbia, MO; 5Drexel University College of Medicine, Chandler, AZ
Introduction: Chronic liver disease can stem from metabolic, autoimmune, genetic, infectious, or toxin-induced etiologies. As the prevalence of metabolic dysfunction-associated steatohepatitis (MASH) continues to rise, the likelihood of encountering overlap syndromes involving multiple etiologies is increasing. We present a rare case of triple-pathology liver disease involving MASH, autoimmune hepatitis (AIH), and alpha-1 antitrypsin (AAT) deficiency.
Case Description/
Methods: A 52-year-old female with a history of newly diagnosed Hashimoto’s thyroiditis and hyperlipidemia presented with 6 months of asymptomatic transaminitis. Labs revealed an ALP of 238 IU/L, AST 72 IU/L, and ALT 91 IU/L. Liver ultrasound showed hepatomegaly (18 cm) and hepatic steatosis. Given her autoimmune background, additional testing was performed. ANA was positive at 1:1280; other autoimmune markers including AMA, ASMA, LKM1 and immunoglobulin levels were unremarkable. Viral hepatitis panel was negative. AAT levels were low 83 mg/dL with MZ phenotype. Fibroscan indicated F0–F1 fibrosis with a CAP of 334 dB/m consistent with severe steatosis. As the clinical picture remained unclear, a liver biopsy was performed with histology demonstrating F2 fibrosis, active steatohepatitis, PAS-positive diastase-resistant globules confirming AAT deficiency, and prominent interface hepatitis with plasma cells, consistent with AIH. The patient was diagnosed with overlapping MASH, AIH, and AAT deficiency. She was treated with prednisone 40 mg daily for 10 weeks with 5 mg taper weekly and azathioprine 50 mg daily that was titrated to 75 mg daily. Serial hepatic panels showed biochemical improvement, though mild transaminitis persisted.
Discussion: This case underscores the clinical complexity and diagnostic challenge of overlapping liver pathologies. Coexisting MASH, AIH, and AAT deficiency is extremely rare and has not been previously reported. Overlapping liver diseases confer higher risk for progression to cirrhosis and worse outcomes compared to isolated liver conditions. Clinicians should maintain a high index of suspicion for multiple concurrent liver diseases in patients with unexplained or persistent liver enzyme abnormalities, especially in the context of metabolic syndrome and autoimmune conditions. Liver biopsy remains critical when noninvasive testing is inconclusive. Identifying and addressing all contributing etiologies is essential for guiding treatment and improving prognosis.
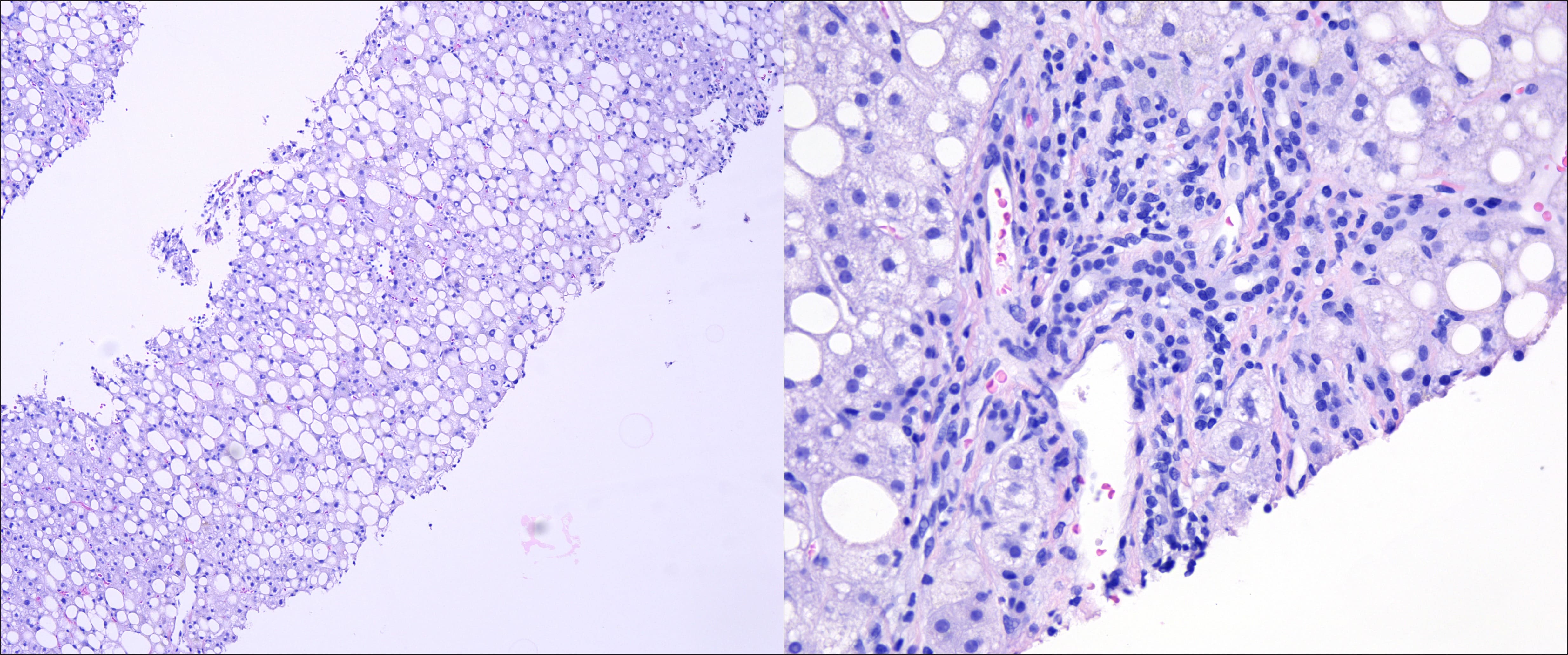
Figure: Left: H&E, 10x: Liver core needle biopsy with macrovesicular steatosis (Grade 3 steatosis)
Right: H&E, 40x: Portal tract with lymphoplasmacytic infiltrate and interface activity
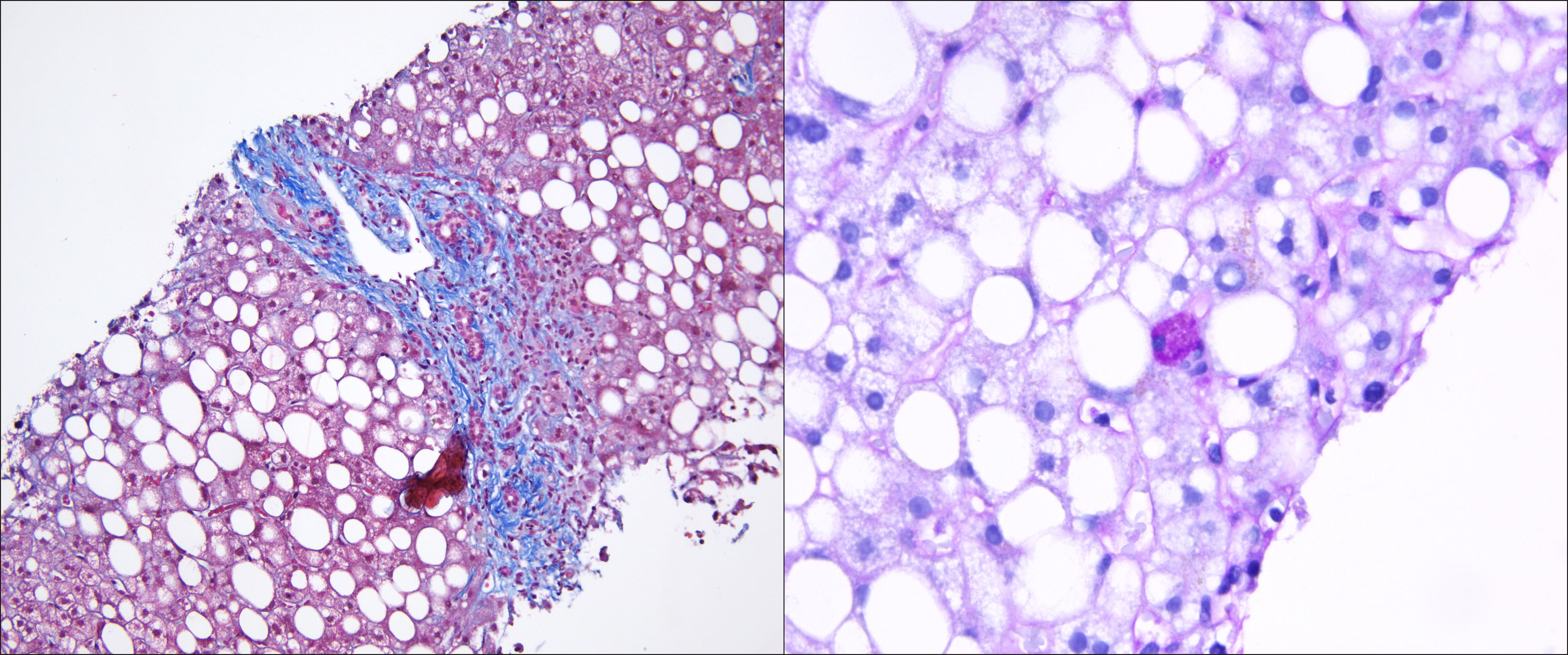
Figure: Left: Trichrome, 20x: Stage 2 fibrosis, with portal/periportal fibrosis
Right: PAS-D, 60x: focal eosinophilic globules of variable sizes within a hepatocyte
Disclosures:
Gopala Konduri indicated no relevant financial relationships.
Muhammad Yousaf indicated no relevant financial relationships.
Austin Reed indicated no relevant financial relationships.
Ahmad Ali indicated no relevant financial relationships.
Hanna Nale indicated no relevant financial relationships.
Deepthi Rao indicated no relevant financial relationships.
Sravya Ponnapalli indicated no relevant financial relationships.
Gopala Konduri, MD1, Muhammad Yousaf, MD2, Austin Reed, DO3, Ahmad Ali, MD1, Hanna Nale, DO4, Deepthi Rao, MD1, Sravya Ponnapalli, MD5. P5999 - A Triple Threat to the Liver: Coexisting MASH, Autoimmune Hepatitis, and Alpha-1 Antitrypsin Deficiency in a Single Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Missouri, Columbia, MO; 2University of Missouri Health Care, Columbia, MO; 3Sunrise Health GME Consortium, Las Vegas, NV; 4University of Missouri School of Medicine, Columbia, MO; 5Drexel University College of Medicine, Chandler, AZ
Introduction: Chronic liver disease can stem from metabolic, autoimmune, genetic, infectious, or toxin-induced etiologies. As the prevalence of metabolic dysfunction-associated steatohepatitis (MASH) continues to rise, the likelihood of encountering overlap syndromes involving multiple etiologies is increasing. We present a rare case of triple-pathology liver disease involving MASH, autoimmune hepatitis (AIH), and alpha-1 antitrypsin (AAT) deficiency.
Case Description/
Methods: A 52-year-old female with a history of newly diagnosed Hashimoto’s thyroiditis and hyperlipidemia presented with 6 months of asymptomatic transaminitis. Labs revealed an ALP of 238 IU/L, AST 72 IU/L, and ALT 91 IU/L. Liver ultrasound showed hepatomegaly (18 cm) and hepatic steatosis. Given her autoimmune background, additional testing was performed. ANA was positive at 1:1280; other autoimmune markers including AMA, ASMA, LKM1 and immunoglobulin levels were unremarkable. Viral hepatitis panel was negative. AAT levels were low 83 mg/dL with MZ phenotype. Fibroscan indicated F0–F1 fibrosis with a CAP of 334 dB/m consistent with severe steatosis. As the clinical picture remained unclear, a liver biopsy was performed with histology demonstrating F2 fibrosis, active steatohepatitis, PAS-positive diastase-resistant globules confirming AAT deficiency, and prominent interface hepatitis with plasma cells, consistent with AIH. The patient was diagnosed with overlapping MASH, AIH, and AAT deficiency. She was treated with prednisone 40 mg daily for 10 weeks with 5 mg taper weekly and azathioprine 50 mg daily that was titrated to 75 mg daily. Serial hepatic panels showed biochemical improvement, though mild transaminitis persisted.
Discussion: This case underscores the clinical complexity and diagnostic challenge of overlapping liver pathologies. Coexisting MASH, AIH, and AAT deficiency is extremely rare and has not been previously reported. Overlapping liver diseases confer higher risk for progression to cirrhosis and worse outcomes compared to isolated liver conditions. Clinicians should maintain a high index of suspicion for multiple concurrent liver diseases in patients with unexplained or persistent liver enzyme abnormalities, especially in the context of metabolic syndrome and autoimmune conditions. Liver biopsy remains critical when noninvasive testing is inconclusive. Identifying and addressing all contributing etiologies is essential for guiding treatment and improving prognosis.
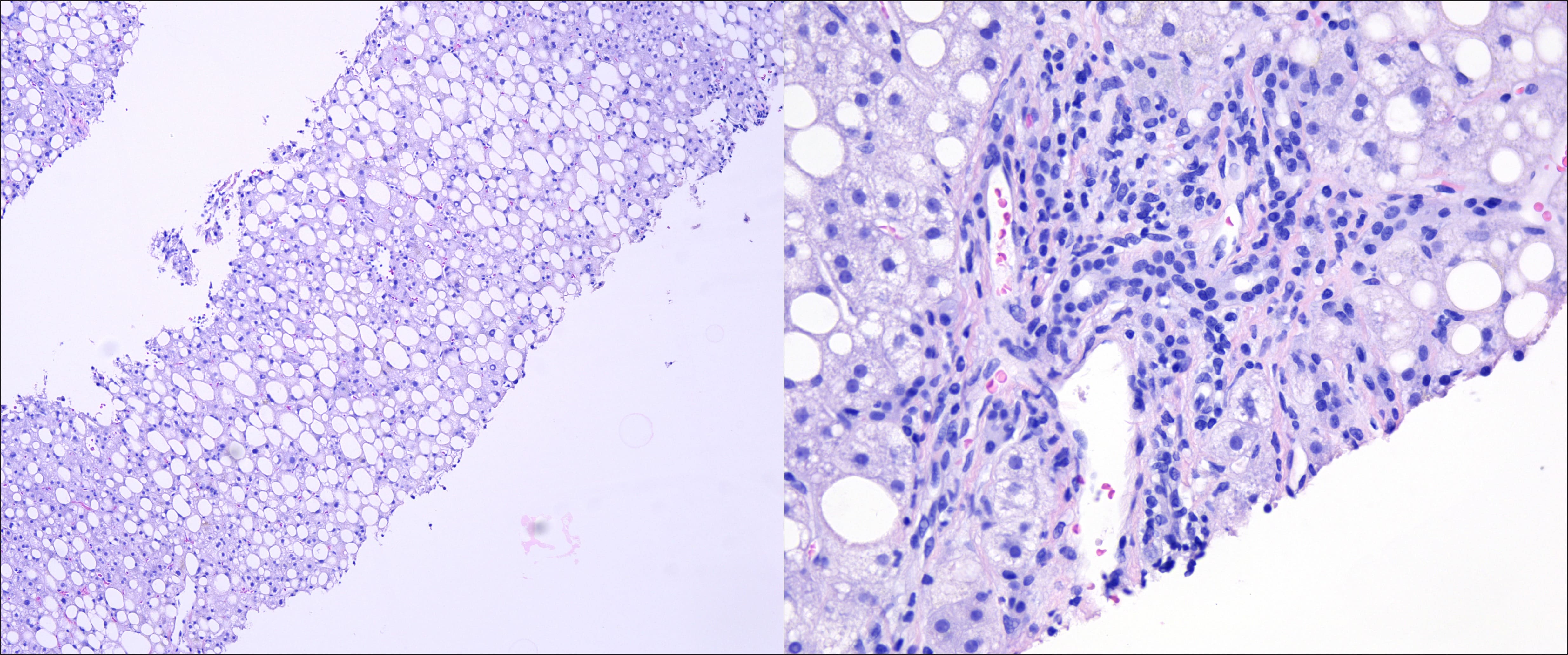
Figure: Left: H&E, 10x: Liver core needle biopsy with macrovesicular steatosis (Grade 3 steatosis)
Right: H&E, 40x: Portal tract with lymphoplasmacytic infiltrate and interface activity
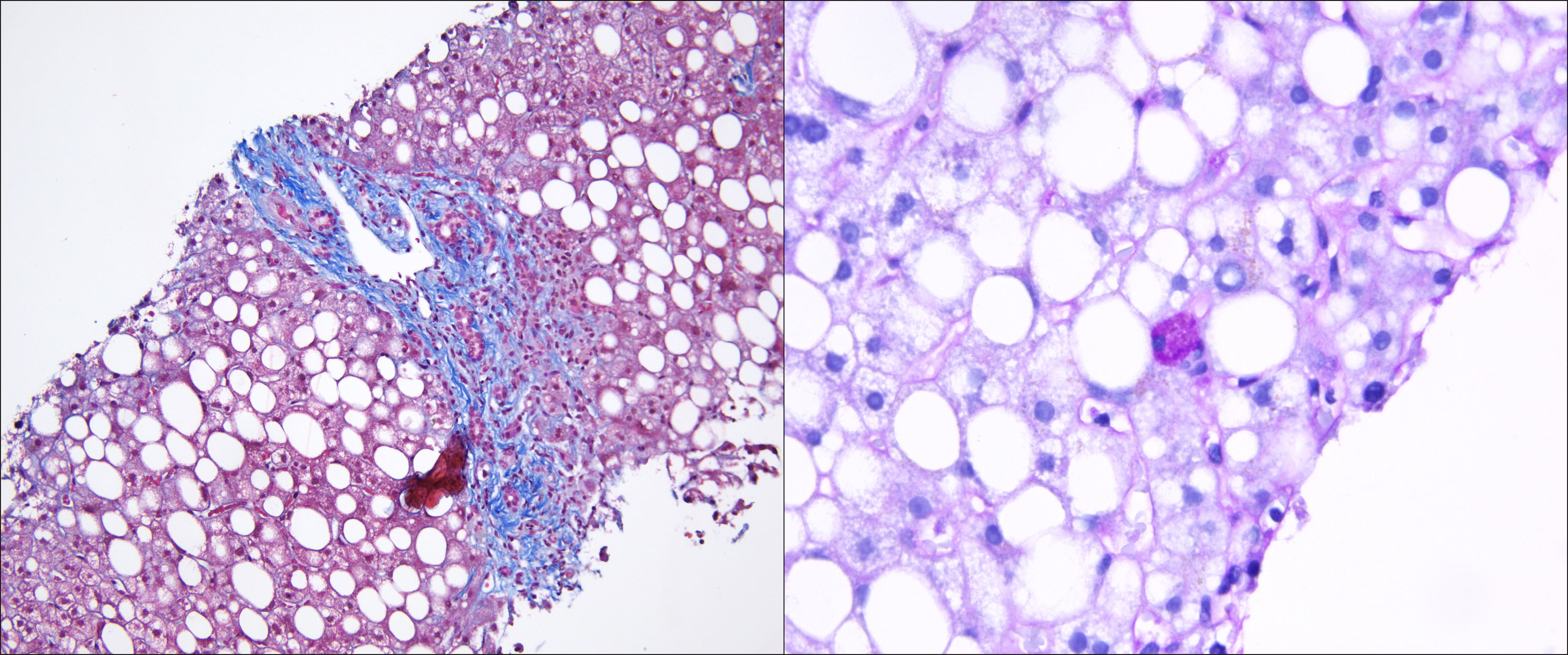
Figure: Left: Trichrome, 20x: Stage 2 fibrosis, with portal/periportal fibrosis
Right: PAS-D, 60x: focal eosinophilic globules of variable sizes within a hepatocyte
Disclosures:
Gopala Konduri indicated no relevant financial relationships.
Muhammad Yousaf indicated no relevant financial relationships.
Austin Reed indicated no relevant financial relationships.
Ahmad Ali indicated no relevant financial relationships.
Hanna Nale indicated no relevant financial relationships.
Deepthi Rao indicated no relevant financial relationships.
Sravya Ponnapalli indicated no relevant financial relationships.
Gopala Konduri, MD1, Muhammad Yousaf, MD2, Austin Reed, DO3, Ahmad Ali, MD1, Hanna Nale, DO4, Deepthi Rao, MD1, Sravya Ponnapalli, MD5. P5999 - A Triple Threat to the Liver: Coexisting MASH, Autoimmune Hepatitis, and Alpha-1 Antitrypsin Deficiency in a Single Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

