Tuesday Poster Session
Category: Liver
P5997 - The Eye That Struck the Liver: A Rare Case of Uveal Melanoma Presenting as a Solitary Hepatic Mass
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Alexa Plato, MD
Yale New Haven Health, Bridgeport Hospital
Bridgeport, CT
Presenting Author(s)
Alexa Plato, MD1, Cheng-Hung Tai, MD1, Raquel Rozner, MD2
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Yale School of Medicine, Gastroenterology Associates, PC, Northeast Medical Group/Yale New Haven Health, Stratford, CT
Introduction: Uveal melanoma is a rare but distinct subtype of melanoma with a marked predilection for
hepatic metastasis. Unlike cutaneous melanoma, it follows a unique molecular and metastatic
profile, often confounding the diagnosis when a primary lesion is not evident. Here we present a rare
case of presumed uveal melanoma discovered incidentally as an isolated hepatic mass in a
patient without prior melanoma history or detectable primary lesion.
Case Description/
Methods: A 58-year-old male with history of celiac disease was noted to have elevated AST/ALT and
microcytic anemia (Hb 12.9 g/dL). Workup revealed an 8 cm hepatic mass on MRI. Core biopsy
confirmed metastatic melanoma. The patient denied prior cutaneous or mucosal lesions.
Colonoscopy and dermatologic total body skin exam were unremarkable. Ophthalmologic
evaluation was initiated, though no classic GNAQ or GNA11 mutations were found on early
molecular profiling. CT CAP and MRI brain showed no other significant disease. Given the
liver-only pattern of metastasis and absence of cutaneous/mucosal primaries, the diagnosis of
GNAQ/GNA11-wild-type uveal melanoma was favored. The patient was enrolled in an
immunotherapy trial.
Discussion: Over 90% of uveal melanomas metastasize to the liver, making it the principal site of distant
disease. This hepatic tropism is so specific that isolated liver involvement in a melanoma of
unknown primary often implicates a uveal origin—even without a detected ocular lesion. While
GNAQ and GNA11 mutations are present in ~83–95% of uveal melanomas, a small but
meaningful subset (~5–17%) is wild-type for both. These cases may harbor alternative mutations
(CYSLTR2, PLCB4, EIF1AX, SF3B1) or none at all, underscoring the diagnostic difficulty.
Importantly, absence of GNAQ/GNA11 does not exclude uveal origin, especially in patients
lacking skin or mucosal findings. The absence of ocular findings may reflect a regressed or
undetected primary tumor, a phenomenon seen in rare metastatic uveal melanoma cases. Primary
hepatic melanoma remains a theoretical possibility but lacks convincing evidence and is
considered vanishingly rare.
This case highlights the diagnostic nuances of hepatic melanoma metastases in the absence of
cutaneous or mucosal primaries, particularly in GNAQ/GNA11-negative disease. It emphasizes
the need for high clinical suspicion, interdisciplinary collaboration, and consideration of uveal
melanoma in solitary liver lesions, even when conventional genetic markers are absent.
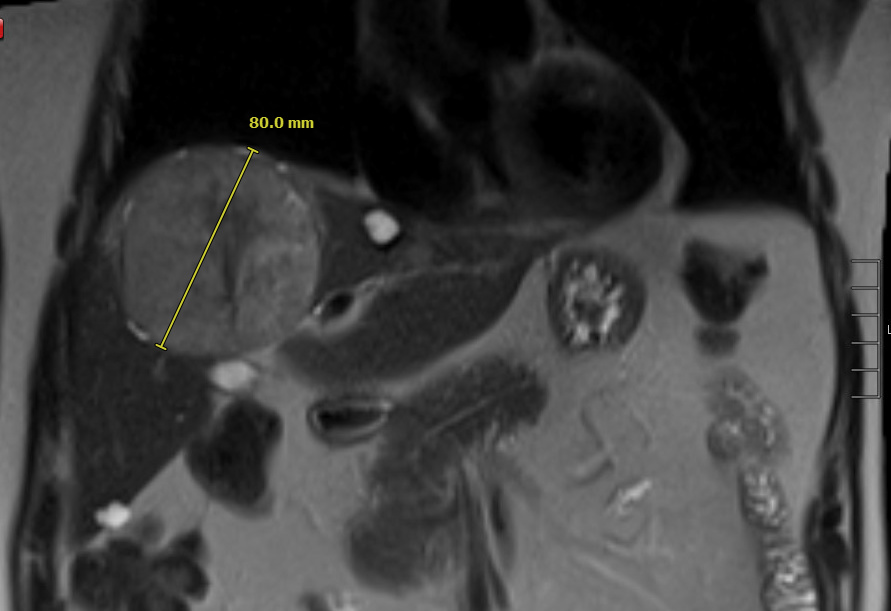
Figure: Image 1: Liver Mass on MRI

Figure: Image 2: Melanoma (Left) within Liver (Right)
Disclosures:
Alexa Plato indicated no relevant financial relationships.
Cheng-Hung Tai indicated no relevant financial relationships.
Raquel Rozner indicated no relevant financial relationships.
Alexa Plato, MD1, Cheng-Hung Tai, MD1, Raquel Rozner, MD2. P5997 - The Eye That Struck the Liver: A Rare Case of Uveal Melanoma Presenting as a Solitary Hepatic Mass, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Yale School of Medicine, Gastroenterology Associates, PC, Northeast Medical Group/Yale New Haven Health, Stratford, CT
Introduction: Uveal melanoma is a rare but distinct subtype of melanoma with a marked predilection for
hepatic metastasis. Unlike cutaneous melanoma, it follows a unique molecular and metastatic
profile, often confounding the diagnosis when a primary lesion is not evident. Here we present a rare
case of presumed uveal melanoma discovered incidentally as an isolated hepatic mass in a
patient without prior melanoma history or detectable primary lesion.
Case Description/
Methods: A 58-year-old male with history of celiac disease was noted to have elevated AST/ALT and
microcytic anemia (Hb 12.9 g/dL). Workup revealed an 8 cm hepatic mass on MRI. Core biopsy
confirmed metastatic melanoma. The patient denied prior cutaneous or mucosal lesions.
Colonoscopy and dermatologic total body skin exam were unremarkable. Ophthalmologic
evaluation was initiated, though no classic GNAQ or GNA11 mutations were found on early
molecular profiling. CT CAP and MRI brain showed no other significant disease. Given the
liver-only pattern of metastasis and absence of cutaneous/mucosal primaries, the diagnosis of
GNAQ/GNA11-wild-type uveal melanoma was favored. The patient was enrolled in an
immunotherapy trial.
Discussion: Over 90% of uveal melanomas metastasize to the liver, making it the principal site of distant
disease. This hepatic tropism is so specific that isolated liver involvement in a melanoma of
unknown primary often implicates a uveal origin—even without a detected ocular lesion. While
GNAQ and GNA11 mutations are present in ~83–95% of uveal melanomas, a small but
meaningful subset (~5–17%) is wild-type for both. These cases may harbor alternative mutations
(CYSLTR2, PLCB4, EIF1AX, SF3B1) or none at all, underscoring the diagnostic difficulty.
Importantly, absence of GNAQ/GNA11 does not exclude uveal origin, especially in patients
lacking skin or mucosal findings. The absence of ocular findings may reflect a regressed or
undetected primary tumor, a phenomenon seen in rare metastatic uveal melanoma cases. Primary
hepatic melanoma remains a theoretical possibility but lacks convincing evidence and is
considered vanishingly rare.
This case highlights the diagnostic nuances of hepatic melanoma metastases in the absence of
cutaneous or mucosal primaries, particularly in GNAQ/GNA11-negative disease. It emphasizes
the need for high clinical suspicion, interdisciplinary collaboration, and consideration of uveal
melanoma in solitary liver lesions, even when conventional genetic markers are absent.
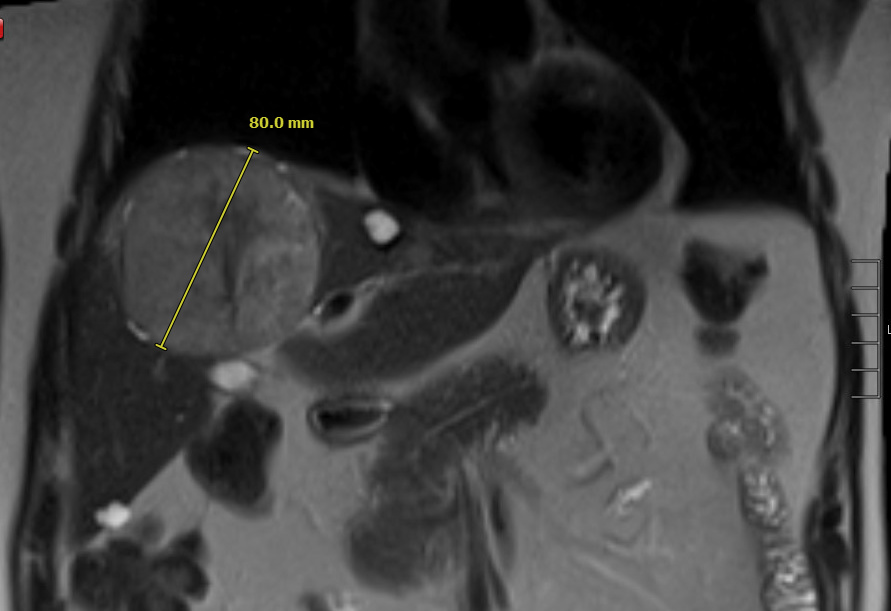
Figure: Image 1: Liver Mass on MRI

Figure: Image 2: Melanoma (Left) within Liver (Right)
Disclosures:
Alexa Plato indicated no relevant financial relationships.
Cheng-Hung Tai indicated no relevant financial relationships.
Raquel Rozner indicated no relevant financial relationships.
Alexa Plato, MD1, Cheng-Hung Tai, MD1, Raquel Rozner, MD2. P5997 - The Eye That Struck the Liver: A Rare Case of Uveal Melanoma Presenting as a Solitary Hepatic Mass, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
