Monday Poster Session
Category: Liver
P3702 - Racial and Sex Disparities in Inpatient Outcomes and Comorbidity Profiles Among Patients With Alcohol-Associated Liver Disease With and Without Metabolic Syndrome: Insights From a Nationally Representative Database
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Talal Bhatti, MBBS (he/him/his)
Northwell Health
Brooklyn, NY
Presenting Author(s)
Talal Bhatti, MBBS1, Carla Barberan Parraga, MD2, Sanjaya Satapathy, MD3, Kundan Raja, MBBS2, Madeha Irfan, MBBS4, Shahzad Ashraf, MD, MBBS, PhD5, Zunaira Naeem, MBBS6, Taimur Aslam, MD7, Fareed Muslim, MD8, Ali Sufyan, MBBS9
1Northwell Health, Brooklyn, NY; 2Maimonides Medical Center, Brooklyn, NY; 3North Shore University Hospital - Northwell Health, Manhasset, NY; 4University of Health Sciences, Brooklyn, NY; 5NUMS, Islamabad, Islamabad, Pakistan; 6University of Health Sciences, Lahore, Punjab, Pakistan; 7Staten Island University Hospital, Northwell Health, Staten Island, NY; 8Mayo Clinic, Florida, FL; 9SZABMU, Islamabad, Islamabad, Pakistan
Introduction: Metabolic dysfunction in alcohol-associated liver disease (ALD), termed MetALD, represents a distinct clinical phenotype. However, disparities in race and sex distribution, comorbidities, and inpatient outcomes among hospitalized ALD patients—with and without metabolic syndrome—remain underexplored.
Methods: We utilized the National Inpatient Sample (2016–2021) to identify adult hospitalizations with a principal diagnosis of ALD using ICD-10 codes. Patients were stratified by the presence of metabolic syndrome, defined as ≥3 of the following: obesity (BMI ≥30), diabetes, hypertension, and hyperlipidemia. Demographic, clinical, and outcome variables were compared using Rao-Scott chi-square and Student’s t-tests. Multivariate regression was performed for outcomes with p < 0.1 in univariate analysis.
Results: Among 936,645 weighted hospitalizations (ALD without MetS: 759,680 [81.1%]; MetS + ALD: 176,965 [18.9%]), the MetS + ALD group had a higher proportion of males (80.1% vs. 67.4%, p < 0.0001) and lower representation of females (19.9% vs. 32.6%, p < 0.0001). Racial differences were also significant: White patients were overrepresented in the MetS + ALD group (70.1% vs. 66.7%, p = 0.0085), while patients classified as 'Other' race were underrepresented (1.8% vs. 3.2%, p = 0.0053). Despite greater comorbidity burden, MetS + ALD patients had lower in-hospital mortality (3.0% vs. 4.9%, p = 0.0024), with no significant differences in length of stay or total hospital charges.
Discussion: MetS + ALD is associated with notable racial and sex disparities, including underrepresentation of non-White groups and female patients. Despite these disparities and a higher metabolic comorbidity load, MetS + ALD patients demonstrated paradoxically lower inpatient mortality, suggesting that phenotype-specific factors or access-related differences may influence outcomes. These findings underscore the need for further research into the mechanisms and health equity implications of MetALD across diverse populations.
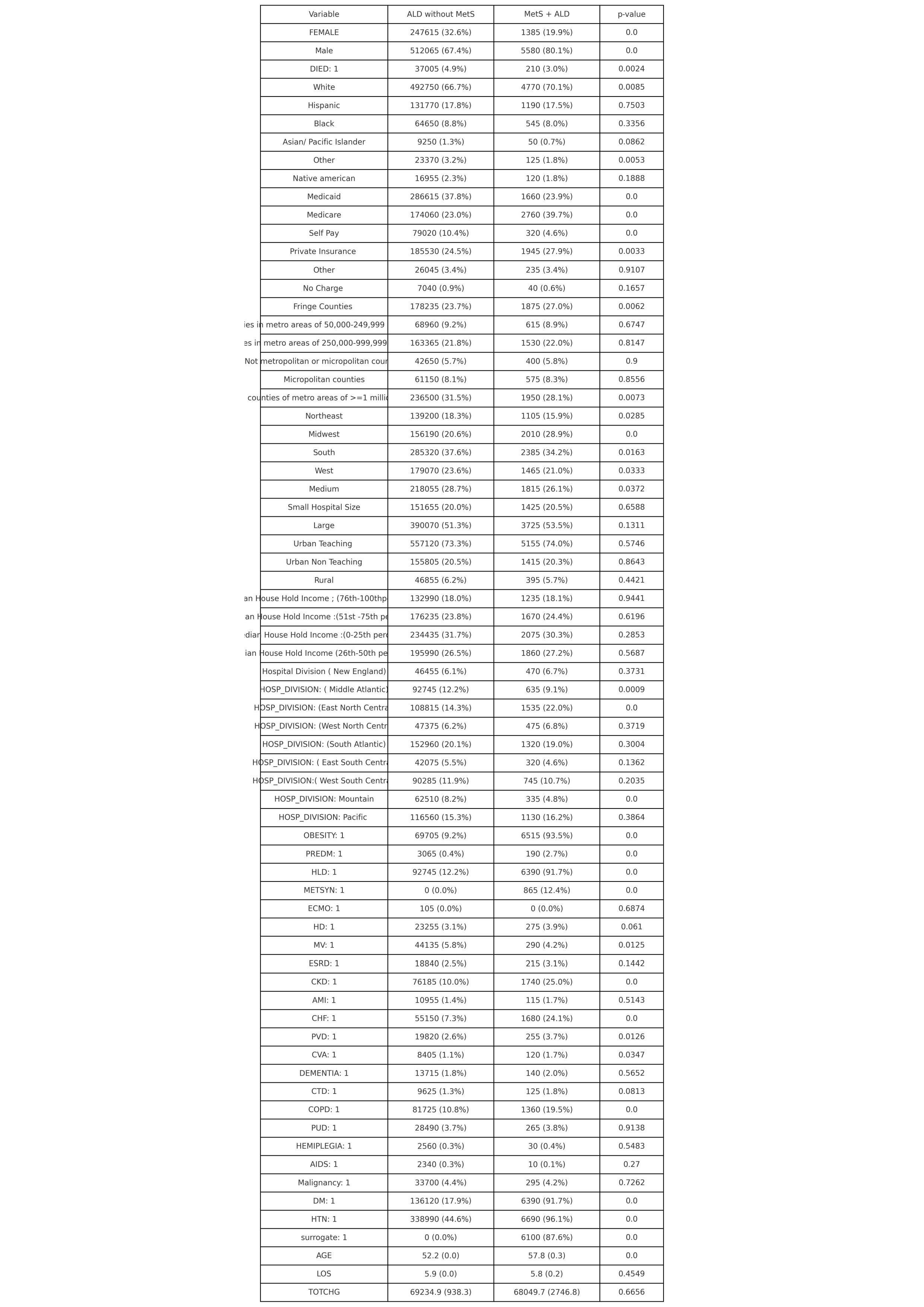
Figure: baseline Characteristics of ALD patients with and without metabolic Syndrome
Disclosures:
Talal Bhatti indicated no relevant financial relationships.
Carla Barberan Parraga indicated no relevant financial relationships.
Sanjaya Satapathy indicated no relevant financial relationships.
Kundan Raja indicated no relevant financial relationships.
Madeha Irfan indicated no relevant financial relationships.
Shahzad Ashraf indicated no relevant financial relationships.
Zunaira Naeem indicated no relevant financial relationships.
Taimur Aslam indicated no relevant financial relationships.
Fareed Muslim indicated no relevant financial relationships.
Ali Sufyan indicated no relevant financial relationships.
Talal Bhatti, MBBS1, Carla Barberan Parraga, MD2, Sanjaya Satapathy, MD3, Kundan Raja, MBBS2, Madeha Irfan, MBBS4, Shahzad Ashraf, MD, MBBS, PhD5, Zunaira Naeem, MBBS6, Taimur Aslam, MD7, Fareed Muslim, MD8, Ali Sufyan, MBBS9. P3702 - Racial and Sex Disparities in Inpatient Outcomes and Comorbidity Profiles Among Patients With Alcohol-Associated Liver Disease With and Without Metabolic Syndrome: Insights From a Nationally Representative Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Northwell Health, Brooklyn, NY; 2Maimonides Medical Center, Brooklyn, NY; 3North Shore University Hospital - Northwell Health, Manhasset, NY; 4University of Health Sciences, Brooklyn, NY; 5NUMS, Islamabad, Islamabad, Pakistan; 6University of Health Sciences, Lahore, Punjab, Pakistan; 7Staten Island University Hospital, Northwell Health, Staten Island, NY; 8Mayo Clinic, Florida, FL; 9SZABMU, Islamabad, Islamabad, Pakistan
Introduction: Metabolic dysfunction in alcohol-associated liver disease (ALD), termed MetALD, represents a distinct clinical phenotype. However, disparities in race and sex distribution, comorbidities, and inpatient outcomes among hospitalized ALD patients—with and without metabolic syndrome—remain underexplored.
Methods: We utilized the National Inpatient Sample (2016–2021) to identify adult hospitalizations with a principal diagnosis of ALD using ICD-10 codes. Patients were stratified by the presence of metabolic syndrome, defined as ≥3 of the following: obesity (BMI ≥30), diabetes, hypertension, and hyperlipidemia. Demographic, clinical, and outcome variables were compared using Rao-Scott chi-square and Student’s t-tests. Multivariate regression was performed for outcomes with p < 0.1 in univariate analysis.
Results: Among 936,645 weighted hospitalizations (ALD without MetS: 759,680 [81.1%]; MetS + ALD: 176,965 [18.9%]), the MetS + ALD group had a higher proportion of males (80.1% vs. 67.4%, p < 0.0001) and lower representation of females (19.9% vs. 32.6%, p < 0.0001). Racial differences were also significant: White patients were overrepresented in the MetS + ALD group (70.1% vs. 66.7%, p = 0.0085), while patients classified as 'Other' race were underrepresented (1.8% vs. 3.2%, p = 0.0053). Despite greater comorbidity burden, MetS + ALD patients had lower in-hospital mortality (3.0% vs. 4.9%, p = 0.0024), with no significant differences in length of stay or total hospital charges.
Discussion: MetS + ALD is associated with notable racial and sex disparities, including underrepresentation of non-White groups and female patients. Despite these disparities and a higher metabolic comorbidity load, MetS + ALD patients demonstrated paradoxically lower inpatient mortality, suggesting that phenotype-specific factors or access-related differences may influence outcomes. These findings underscore the need for further research into the mechanisms and health equity implications of MetALD across diverse populations.
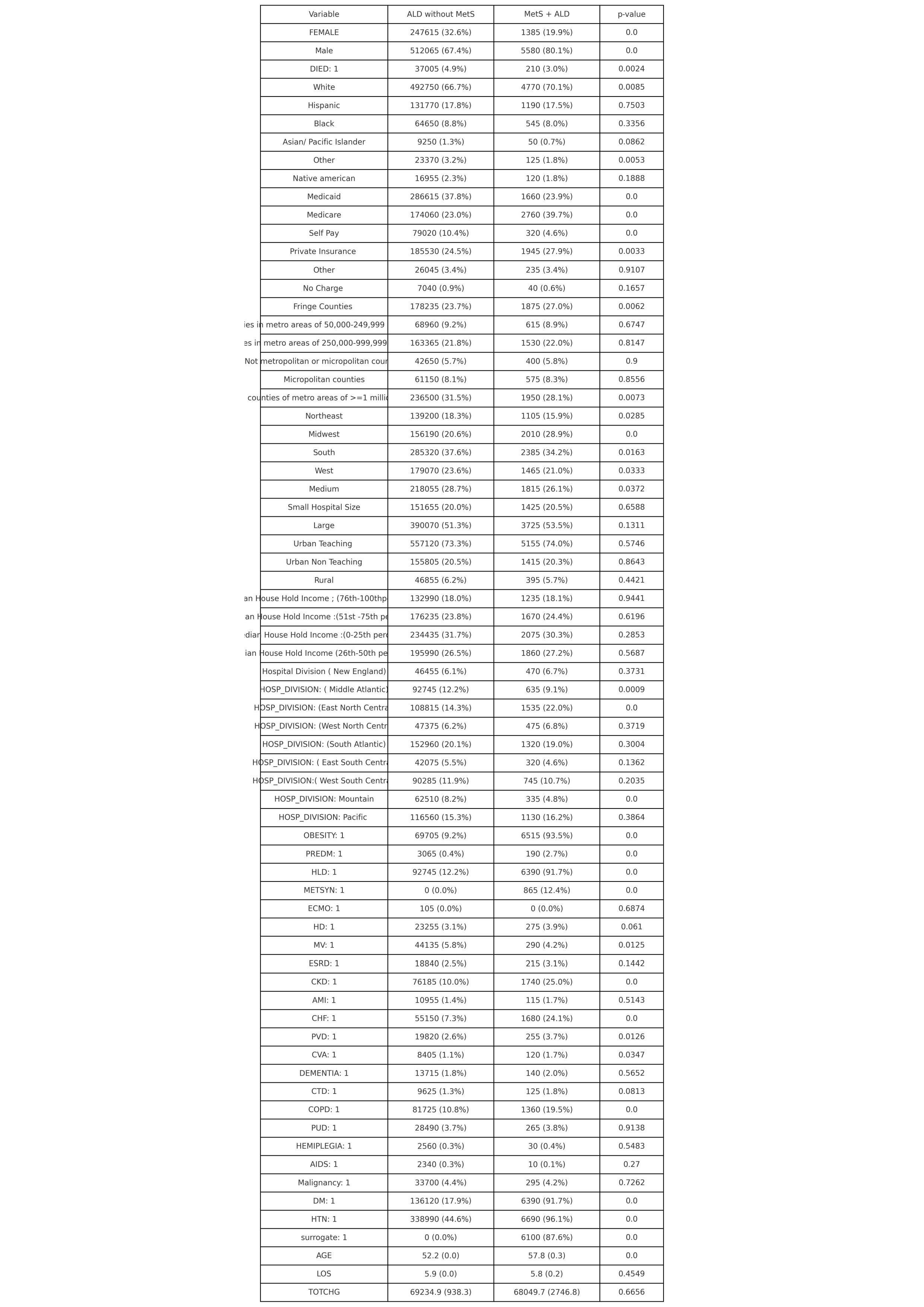
Figure: baseline Characteristics of ALD patients with and without metabolic Syndrome
Disclosures:
Talal Bhatti indicated no relevant financial relationships.
Carla Barberan Parraga indicated no relevant financial relationships.
Sanjaya Satapathy indicated no relevant financial relationships.
Kundan Raja indicated no relevant financial relationships.
Madeha Irfan indicated no relevant financial relationships.
Shahzad Ashraf indicated no relevant financial relationships.
Zunaira Naeem indicated no relevant financial relationships.
Taimur Aslam indicated no relevant financial relationships.
Fareed Muslim indicated no relevant financial relationships.
Ali Sufyan indicated no relevant financial relationships.
Talal Bhatti, MBBS1, Carla Barberan Parraga, MD2, Sanjaya Satapathy, MD3, Kundan Raja, MBBS2, Madeha Irfan, MBBS4, Shahzad Ashraf, MD, MBBS, PhD5, Zunaira Naeem, MBBS6, Taimur Aslam, MD7, Fareed Muslim, MD8, Ali Sufyan, MBBS9. P3702 - Racial and Sex Disparities in Inpatient Outcomes and Comorbidity Profiles Among Patients With Alcohol-Associated Liver Disease With and Without Metabolic Syndrome: Insights From a Nationally Representative Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
