Monday Poster Session
Category: Liver
P3700 - Hepatic Encephalopathy Readmission Rates and Assessment
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Madeline Washburn, DO
Baylor Scott & White Medical Center
Temple, TX
Presenting Author(s)
Madeline Washburn-Rodriguez, DO, Lancaster Weld, DO, Jennifer Vincent, DO
Baylor Scott & White Medical Center, Temple, TX
Introduction: Decompensated cirrhosis and its complications lead to significant morbidity and mortality in the United States. Complications need to be managed closely in the outpatient setting in order to avoid repeat hospitalizations. Ongoing literature suggests that hepatic encephalopathy (HE) is the leading cause of readmission in patients with decompensated cirrhosis. Optimizing medical management upon discharge is critical to avoid readmission. We would like to compare the readmission rates and mortality for patients with HE before and after introducing an automated lactulose reminder as well as a rifaximin prior authorization algorithm.
Methods: This retrospective review used data obtained by the Best Practice Advisory board at our institution to determine the impact of prior interventions on mortality and readmission rates within 30 days for decompensated cirrhotic patients with HE. In October 2023, our institution introduced an alert in the electronic medical record to ensure that lactulose was ordered for the patient upon admission. We also introduced another intervention which took a multidisciplinary approach. Upon ordering rifaximin, the pharmacy would know to begin the process of authorizing the medication for outpatient use. Figure 1 provides an overview of the interventions. Mortality and 30-day readmission rates from one year prior to these interventions were compared to those one year after the interventions.
Results: From October 1, 2022 to September 30, 2023, the 30-day readmission rate was 23.83% and the mortality rate was 13.24%. This was the control group and consisted of 306 encounters (n=306). From October 1, 2023 to September 30, 2024, the 30-day readmission rate was 21.30% and the mortality rate was 9.39%. This was the intervention group and consisted of 399 encounters (n=399). Refer to Table 1 for the corresponding data.
Discussion: Data suggests that 30-day readmission and mortality rates after introducing the automated approaches to initiate lactulose and begin prior authorization for rifaximin were improved. The small degree of improvement post intervention could be due to a variety of factors such as infection, falls, other comorbidities, and patients not taking rifaximin due to cost, miscommunication, or non-compliance. Though encouraging, additional intervention is necessary to further decrease readmission rates in decompensated cirrhotic patients with HE. Prospective studies to further intervene and ensure access to rifaximin are ongoing at our institution.
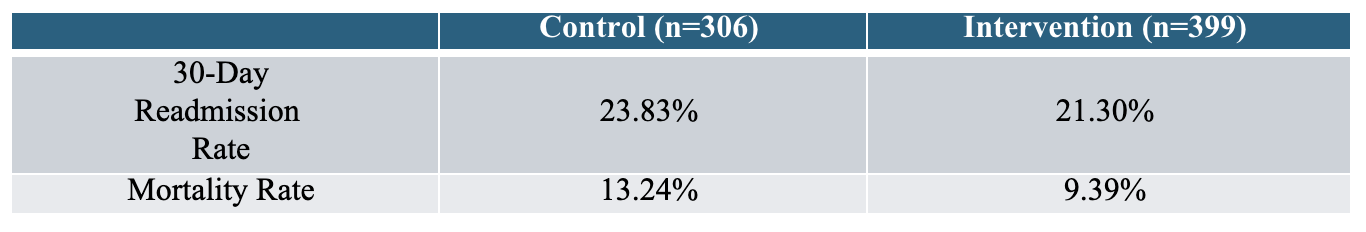
Figure: Figure 1: Flow diagram illustrating the two interventions. 1. The first intervention was put forth by the Best Practice Advisory who created an automated order for lactulose upon admission for those with HE. 2. The second intervention involves initiating the prior authorization for rifaximin while the patient is admitted if the patient has received rifaximin while in the hospital.
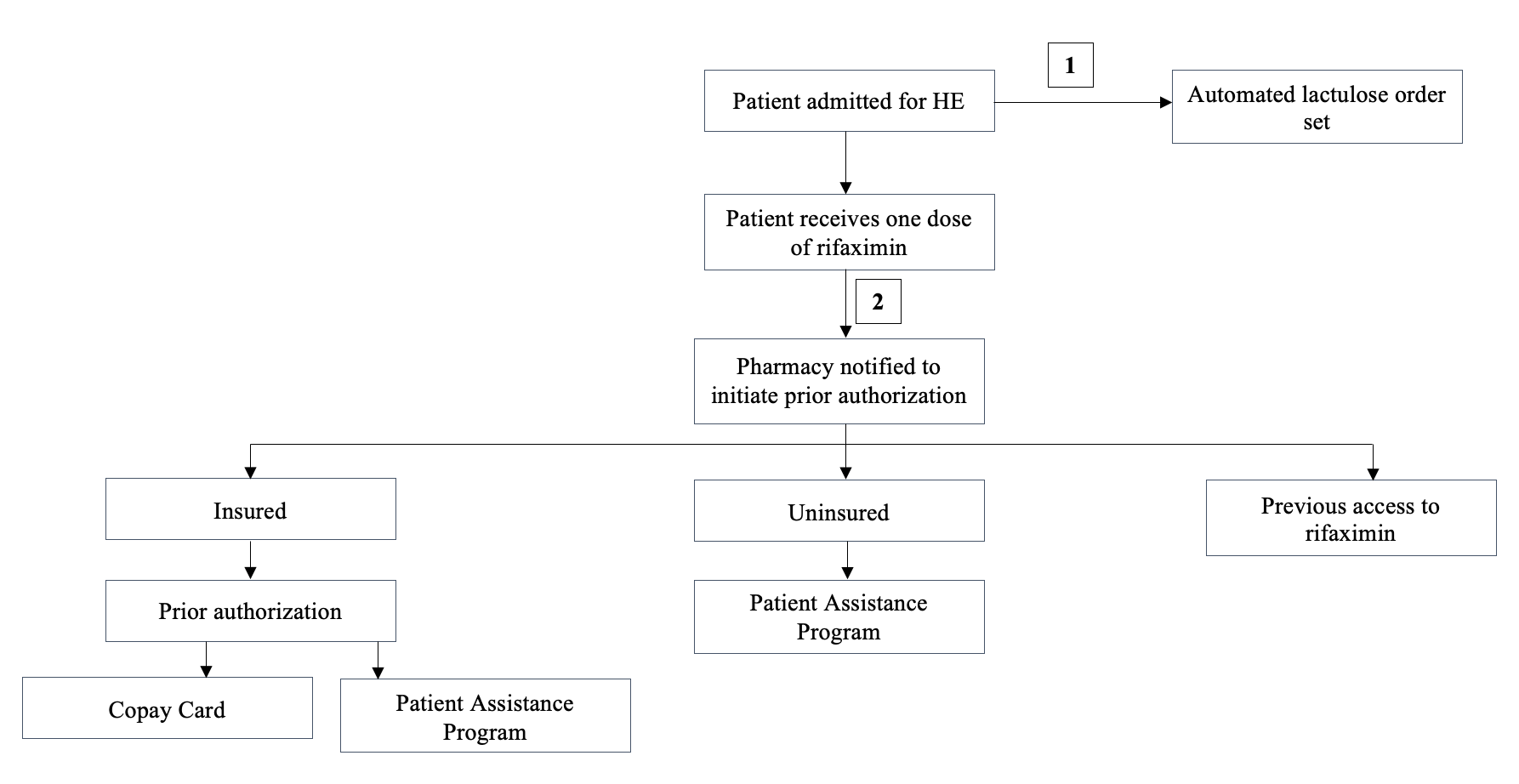
Figure: Table 1: 30-day readmission rates and mortality rates before and after interventions.
Disclosures:
Madeline Washburn-Rodriguez indicated no relevant financial relationships.
Lancaster Weld indicated no relevant financial relationships.
Jennifer Vincent indicated no relevant financial relationships.
Madeline Washburn-Rodriguez, DO, Lancaster Weld, DO, Jennifer Vincent, DO. P3700 - Hepatic Encephalopathy Readmission Rates and Assessment, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Baylor Scott & White Medical Center, Temple, TX
Introduction: Decompensated cirrhosis and its complications lead to significant morbidity and mortality in the United States. Complications need to be managed closely in the outpatient setting in order to avoid repeat hospitalizations. Ongoing literature suggests that hepatic encephalopathy (HE) is the leading cause of readmission in patients with decompensated cirrhosis. Optimizing medical management upon discharge is critical to avoid readmission. We would like to compare the readmission rates and mortality for patients with HE before and after introducing an automated lactulose reminder as well as a rifaximin prior authorization algorithm.
Methods: This retrospective review used data obtained by the Best Practice Advisory board at our institution to determine the impact of prior interventions on mortality and readmission rates within 30 days for decompensated cirrhotic patients with HE. In October 2023, our institution introduced an alert in the electronic medical record to ensure that lactulose was ordered for the patient upon admission. We also introduced another intervention which took a multidisciplinary approach. Upon ordering rifaximin, the pharmacy would know to begin the process of authorizing the medication for outpatient use. Figure 1 provides an overview of the interventions. Mortality and 30-day readmission rates from one year prior to these interventions were compared to those one year after the interventions.
Results: From October 1, 2022 to September 30, 2023, the 30-day readmission rate was 23.83% and the mortality rate was 13.24%. This was the control group and consisted of 306 encounters (n=306). From October 1, 2023 to September 30, 2024, the 30-day readmission rate was 21.30% and the mortality rate was 9.39%. This was the intervention group and consisted of 399 encounters (n=399). Refer to Table 1 for the corresponding data.
Discussion: Data suggests that 30-day readmission and mortality rates after introducing the automated approaches to initiate lactulose and begin prior authorization for rifaximin were improved. The small degree of improvement post intervention could be due to a variety of factors such as infection, falls, other comorbidities, and patients not taking rifaximin due to cost, miscommunication, or non-compliance. Though encouraging, additional intervention is necessary to further decrease readmission rates in decompensated cirrhotic patients with HE. Prospective studies to further intervene and ensure access to rifaximin are ongoing at our institution.
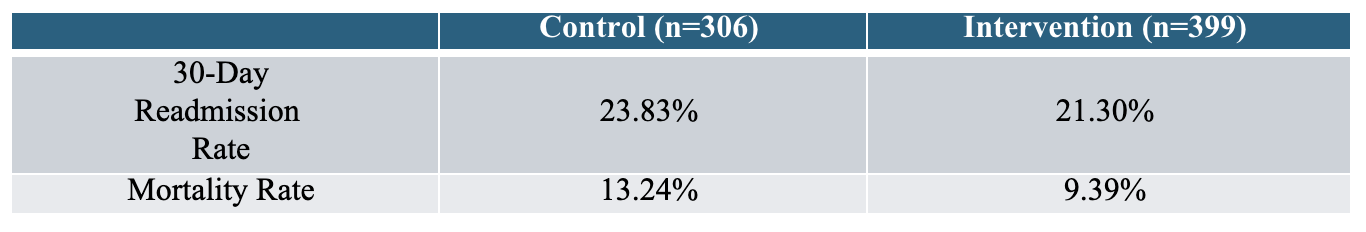
Figure: Figure 1: Flow diagram illustrating the two interventions. 1. The first intervention was put forth by the Best Practice Advisory who created an automated order for lactulose upon admission for those with HE. 2. The second intervention involves initiating the prior authorization for rifaximin while the patient is admitted if the patient has received rifaximin while in the hospital.
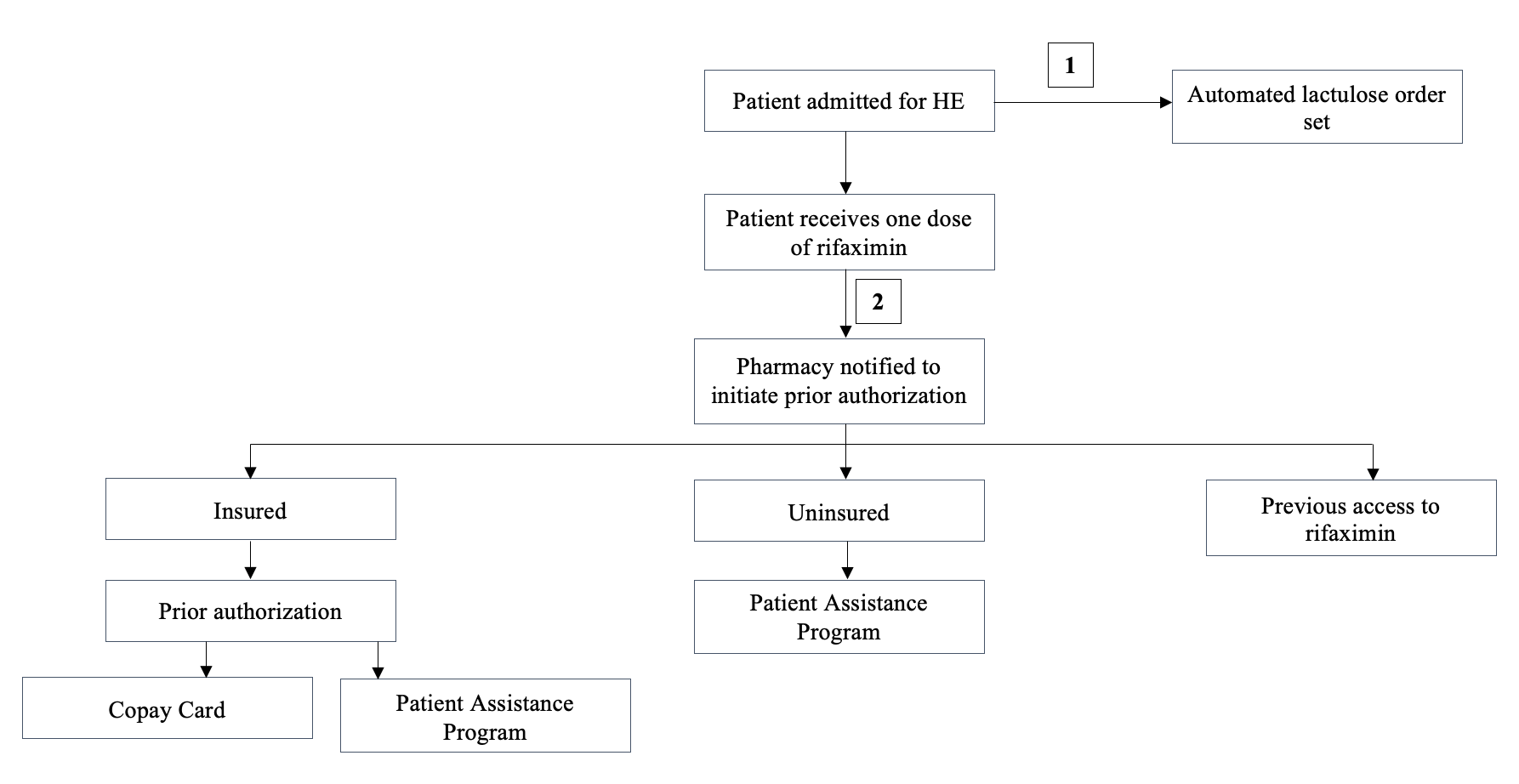
Figure: Table 1: 30-day readmission rates and mortality rates before and after interventions.
Disclosures:
Madeline Washburn-Rodriguez indicated no relevant financial relationships.
Lancaster Weld indicated no relevant financial relationships.
Jennifer Vincent indicated no relevant financial relationships.
Madeline Washburn-Rodriguez, DO, Lancaster Weld, DO, Jennifer Vincent, DO. P3700 - Hepatic Encephalopathy Readmission Rates and Assessment, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
