Monday Poster Session
Category: Liver
P3699 - Assessing the Effects of Glucagon-Like Peptide-1 Agonists and Lifestyle Changes on Fibrosis and Steatosis in Metabolic Dysfunction-Associated Steatotic Liver Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Jason N. Chen, MD (he/him/his)
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Jason N.. Chen, MD, Bulent Tolga. Delibasi, BA, Thomas Tran, BSA, Connie Hu, BA, James Wang, MD, Charles Randall, MD
University of Texas Health San Antonio, San Antonio, TX
Introduction: Metabolic associated diseases, conditions caused by disruptions in normal metabolic processing, are on the rise. One example is Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD). The gold standard for treatment has been lifestyle modifications, including diet and exercise. However, new research suggests the potential role of glucagon-like peptide-1 (GLP-1) agonists in treating MASLD. Initially developed for diabetes and obesity management, the difference between GLP-1 agonists and lifestyle modification effects on MASLD is ambiguous. This study aims to compare GLP-1 agonist and lifestyle modifications on liver metrics in MASLD.
Methods: This ongoing retrospective chart review compared liver metrics, including liver function enzymes and fibroscan scores, between adults who dieted or exercised and those who took a GLP-1 agonist. For each patient, two data sets were collected 6 months to 3 years apart. Descriptive statistics and two-sample t-tests (α = 0.05) were used to analyze differences in outcomes between the two groups.
Results: Of 84 patients, the average age was 59.3 years; 44% were Hispanic and 69%/31% were female/male. There was an overall 2.6% decrease in fibrosis-4 (FIB-4) scores, a 4% decrease in Controlled Attenuation Parameter (CAP) scores, and a 6.7% decrease in liver stiffness (kPa) for those who engaged in lifestyle modifications or used GLP-1 agonists. There were no significant differences between lifestyle only and GLP-1 agonist use in terms of fib-4 score (p = 0.16), CAP score (p = 0.87), or kPa (p = 0.83) (Figure 1). However, the average fib-4 score decreased more (11.2%) in those on GLP-1 agonists compared to those who were engaging in lifestyle changes only (0% change). The average CAP and kPa decrease was 4.5% and 5% for those on GLP-1 and 3.8% and 7.4% for those engaging in lifestyle only, respectively.
Discussion: While both lifestyle modifications and GLP-1 agonists were associated with improvements in liver metrics among patients with MASLD, no significant differences were observed. Notably, GLP-1 agonist use was associated with a greater reduction in FIB-4 scores, suggesting a potential advantage in improving fibrosis-related outcomes. However, lifestyle interventions resulted in greater reductions in liver stiffness. These findings highlight the clinical relevance of both approaches and support the need for further studies to better define the role of GLP-1 agonists in the management of MASLD in addition to traditional lifestyle strategies.
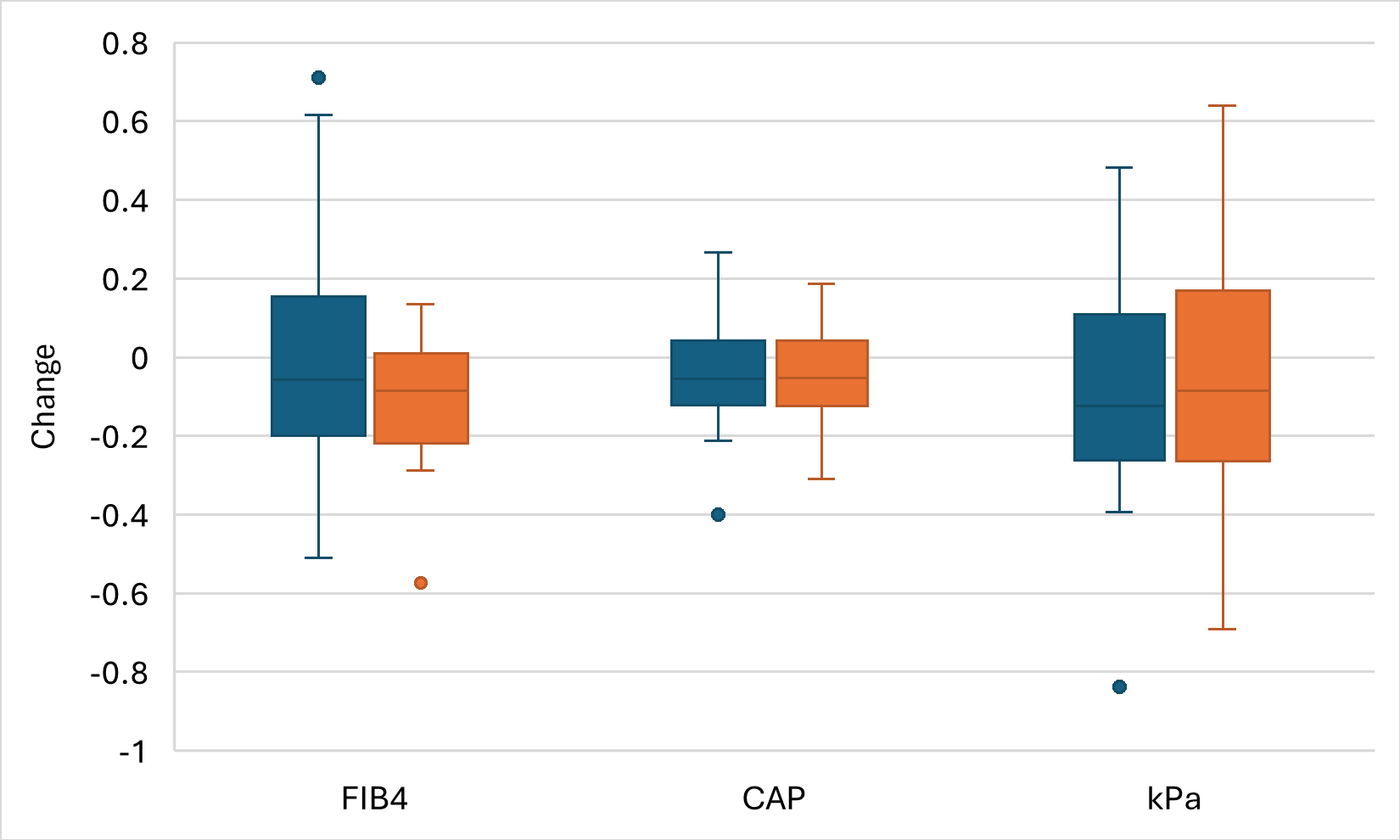
Figure: Figure 1. Changes in fibrosis 4 (FIB4), Controlled Attenuation Parameter (CAP), and liver stiffness (kPa) compared between patients who engaged in lifestyle management only (blue) and GLP-1 agonist use (orange).
Disclosures:
Jason Chen indicated no relevant financial relationships.
Bulent Delibasi indicated no relevant financial relationships.
Thomas Tran indicated no relevant financial relationships.
Connie Hu indicated no relevant financial relationships.
James Wang indicated no relevant financial relationships.
Charles Randall indicated no relevant financial relationships.
Jason N.. Chen, MD, Bulent Tolga. Delibasi, BA, Thomas Tran, BSA, Connie Hu, BA, James Wang, MD, Charles Randall, MD. P3699 - Assessing the Effects of Glucagon-Like Peptide-1 Agonists and Lifestyle Changes on Fibrosis and Steatosis in Metabolic Dysfunction-Associated Steatotic Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Texas Health San Antonio, San Antonio, TX
Introduction: Metabolic associated diseases, conditions caused by disruptions in normal metabolic processing, are on the rise. One example is Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD). The gold standard for treatment has been lifestyle modifications, including diet and exercise. However, new research suggests the potential role of glucagon-like peptide-1 (GLP-1) agonists in treating MASLD. Initially developed for diabetes and obesity management, the difference between GLP-1 agonists and lifestyle modification effects on MASLD is ambiguous. This study aims to compare GLP-1 agonist and lifestyle modifications on liver metrics in MASLD.
Methods: This ongoing retrospective chart review compared liver metrics, including liver function enzymes and fibroscan scores, between adults who dieted or exercised and those who took a GLP-1 agonist. For each patient, two data sets were collected 6 months to 3 years apart. Descriptive statistics and two-sample t-tests (α = 0.05) were used to analyze differences in outcomes between the two groups.
Results: Of 84 patients, the average age was 59.3 years; 44% were Hispanic and 69%/31% were female/male. There was an overall 2.6% decrease in fibrosis-4 (FIB-4) scores, a 4% decrease in Controlled Attenuation Parameter (CAP) scores, and a 6.7% decrease in liver stiffness (kPa) for those who engaged in lifestyle modifications or used GLP-1 agonists. There were no significant differences between lifestyle only and GLP-1 agonist use in terms of fib-4 score (p = 0.16), CAP score (p = 0.87), or kPa (p = 0.83) (Figure 1). However, the average fib-4 score decreased more (11.2%) in those on GLP-1 agonists compared to those who were engaging in lifestyle changes only (0% change). The average CAP and kPa decrease was 4.5% and 5% for those on GLP-1 and 3.8% and 7.4% for those engaging in lifestyle only, respectively.
Discussion: While both lifestyle modifications and GLP-1 agonists were associated with improvements in liver metrics among patients with MASLD, no significant differences were observed. Notably, GLP-1 agonist use was associated with a greater reduction in FIB-4 scores, suggesting a potential advantage in improving fibrosis-related outcomes. However, lifestyle interventions resulted in greater reductions in liver stiffness. These findings highlight the clinical relevance of both approaches and support the need for further studies to better define the role of GLP-1 agonists in the management of MASLD in addition to traditional lifestyle strategies.
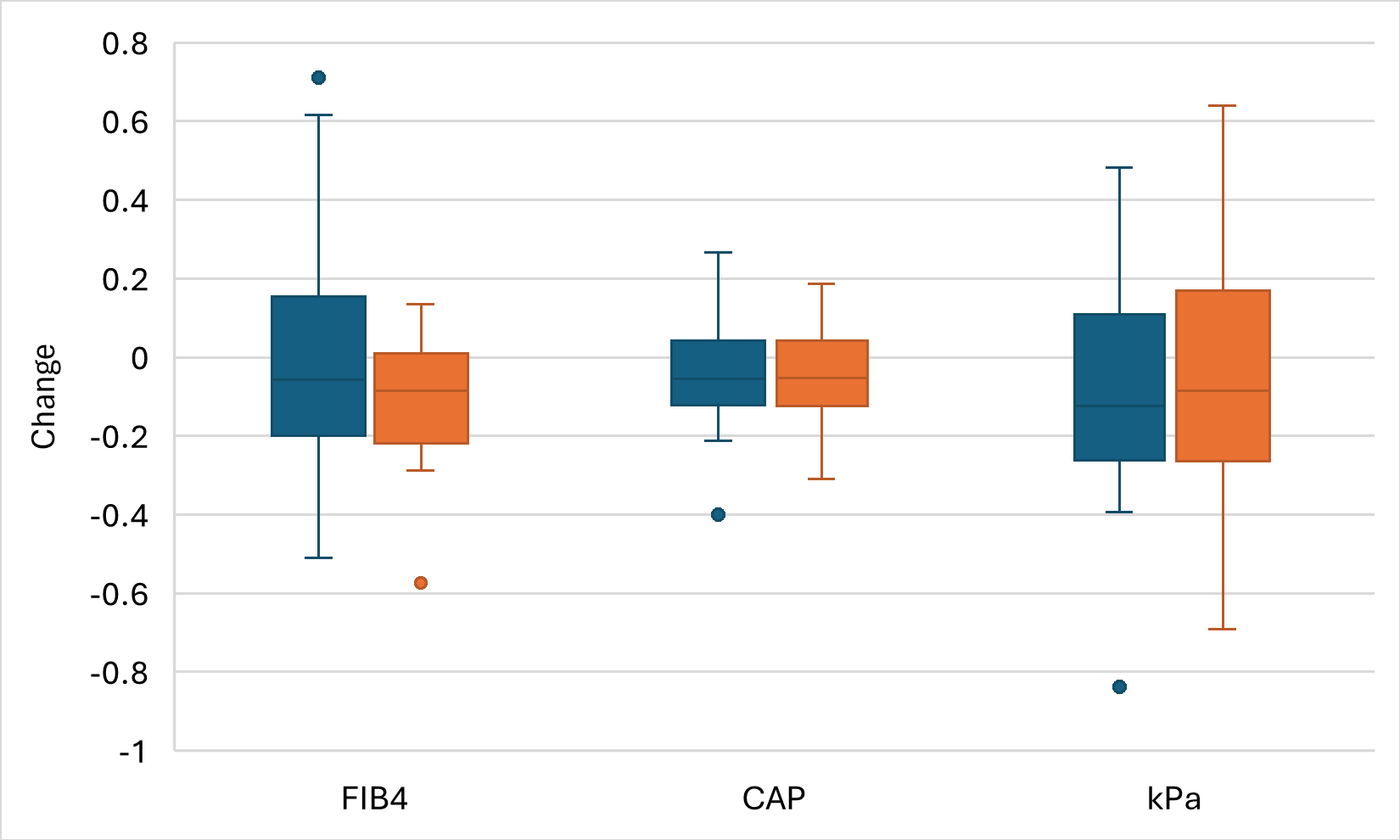
Figure: Figure 1. Changes in fibrosis 4 (FIB4), Controlled Attenuation Parameter (CAP), and liver stiffness (kPa) compared between patients who engaged in lifestyle management only (blue) and GLP-1 agonist use (orange).
Disclosures:
Jason Chen indicated no relevant financial relationships.
Bulent Delibasi indicated no relevant financial relationships.
Thomas Tran indicated no relevant financial relationships.
Connie Hu indicated no relevant financial relationships.
James Wang indicated no relevant financial relationships.
Charles Randall indicated no relevant financial relationships.
Jason N.. Chen, MD, Bulent Tolga. Delibasi, BA, Thomas Tran, BSA, Connie Hu, BA, James Wang, MD, Charles Randall, MD. P3699 - Assessing the Effects of Glucagon-Like Peptide-1 Agonists and Lifestyle Changes on Fibrosis and Steatosis in Metabolic Dysfunction-Associated Steatotic Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

