Monday Poster Session
Category: Liver
P3690 - Autoimmune Hepatitis Overlaps: One-Year Outcome Differences Between PBC and PSC Variants
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- A
Alvina, MD (she/her/hers)
SUNY Upstate Medical University Hospital
Syracuse, New York
Presenting Author(s)
Chidera Onwuzo, MBBS1, Somtochukwu Onwuzo, MD2, Kojo-Frimpong B. Awuah, MD3, Rashid Abdel-Razeq, MD4, Emmanuel Otabor, MBBS5, Alvina, MD1, Laith Alomari, MD5, Vishal Busa, MD1
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Allegheny Health Network, Pittsburgh, PA; 4Cleveland Clinic Foundation, Cleveland, OH; 5Thomas Jefferson University, Philadelphia, PA
Introduction: Autoimmune hepatitis (AIH) can coexist with either primary biliary cholangitis (PBC) or primary sclerosing cholangitis (PSC), forming distinct overlap syndromes with variable prognoses. While both conditions are recognized in clinical hepatology, comparative outcome data remains limited. This study aimed to compare 1-year clinical outcomes between AIH-PBC and AIH-PSC overlap syndromes using a large, multicenter EHR database.
Methods: We used the TriNetX Global Collaborative Network to conduct a retrospective cohort study. Cohort 1 included 6,654 patients with AIH-PBC overlap; cohort 2 included 1,994 with AIH-PSC overlap. Propensity score matching (1:1) was performed using a greedy nearest-neighbor algorithm (caliper: 0.1 SD), balancing age, sex, race, comorbidities (e.g., diabetes, obesity, cardiovascular disease), nicotine use, and NSAID exposure. This yielded 1,592 patients in each group. Outcomes assessed over 1 year post-index included mortality, cirrhosis, portal vein thrombosis (PVT), liver transplantation, cholangiocarcinoma, and hepatocellular carcinoma (HCC). Odds ratios (OR) with 95% confidence intervals (CI) were used for comparison.
Results: After matching cohorts , the AIH-PBC group had significantly lower odds of cirrhosis (OR 0.688, 95% CI 0.553–0.855, p=0.001), cholangiocarcinoma (OR 0.418, 95% CI 0.243–0.719, p=0.001), and all-cause mortality (OR 0.806, 95% CI 0.653–0.993, p=0.043) compared to the AIH-PSC group. No significant differences were observed for PVT (OR 0.827, p=0.254), liver transplantation (OR 0.931, p=0.585), or HCC (OR 1.002, p=0.997).
Discussion: Patients with AIH-PBC overlap syndrome experienced significantly lower risks of cirrhosis, mortality, and particularly cholangiocarcinoma compared to those with AIH-PSC, highlighting the more favorable prognosis associated with AIH-PBC. In contrast, the AIH-PSC phenotype appears to follow a more aggressive clinical course, which reinforces the importance of early recognition, close monitoring, and timely intervention in this subgroup. These findings support the need for risk-stratified surveillance strategies and may help inform therapeutic decision-making. Further prospective studies are essential to validate these observations and explore underlying pathophysiologic differences.
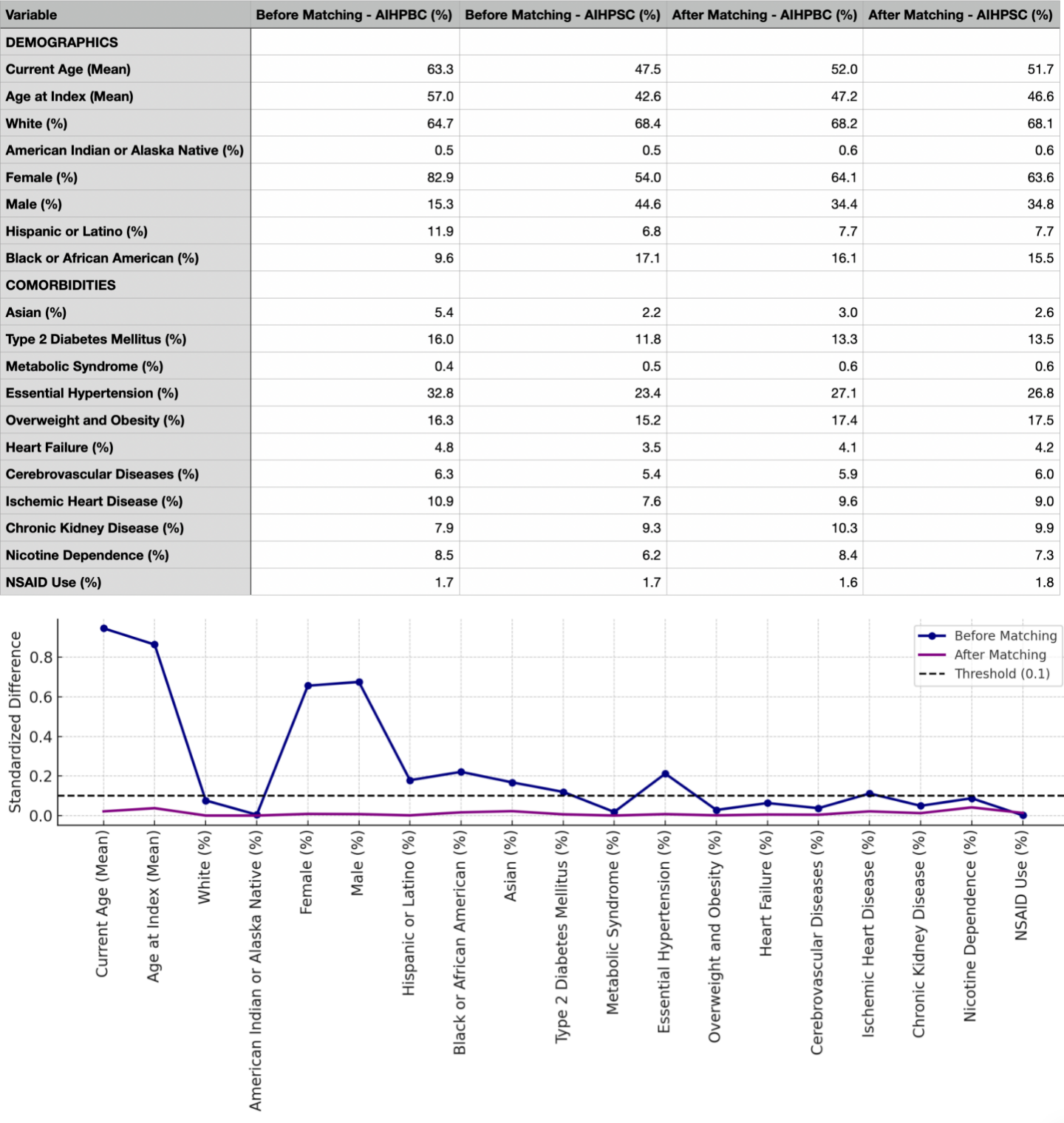
Figure: Figure 1: Baseline Characteristics of the Study Population and Standardized Mean Differences Before and After Propensity Score Matching,
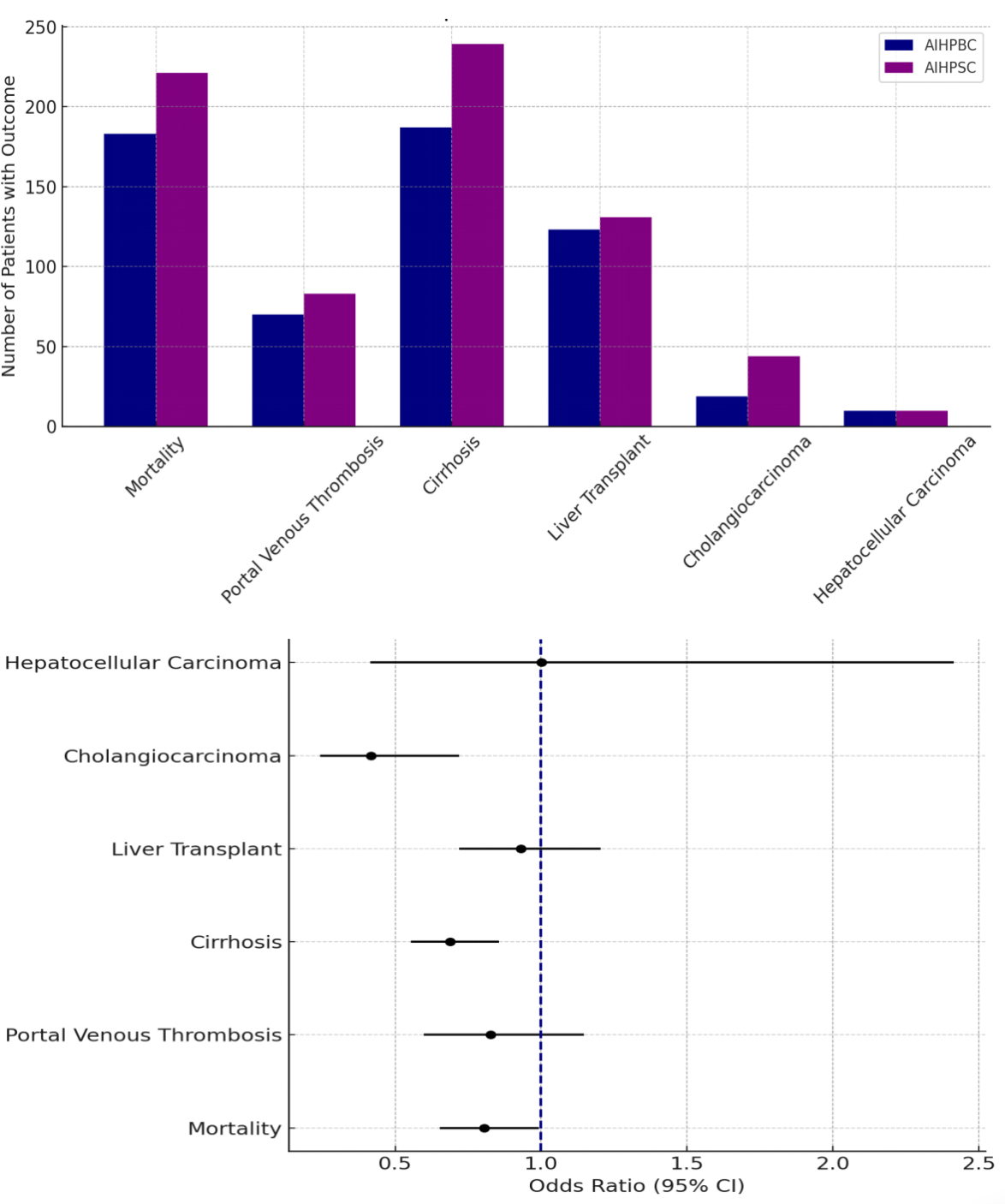
Figure: Figure 2: Comparative Outcomes Between AIH-PBC and AIH-PSC Groups, Including Forest Plot of Odds Ratios
Disclosures:
Chidera Onwuzo indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Emmanuel Otabor indicated no relevant financial relationships.
Alvina indicated no relevant financial relationships.
Laith Alomari indicated no relevant financial relationships.
Vishal Busa indicated no relevant financial relationships.
Chidera Onwuzo, MBBS1, Somtochukwu Onwuzo, MD2, Kojo-Frimpong B. Awuah, MD3, Rashid Abdel-Razeq, MD4, Emmanuel Otabor, MBBS5, Alvina, MD1, Laith Alomari, MD5, Vishal Busa, MD1. P3690 - Autoimmune Hepatitis Overlaps: One-Year Outcome Differences Between PBC and PSC Variants, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Upstate Medical University Hospital, Syracuse, NY; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Allegheny Health Network, Pittsburgh, PA; 4Cleveland Clinic Foundation, Cleveland, OH; 5Thomas Jefferson University, Philadelphia, PA
Introduction: Autoimmune hepatitis (AIH) can coexist with either primary biliary cholangitis (PBC) or primary sclerosing cholangitis (PSC), forming distinct overlap syndromes with variable prognoses. While both conditions are recognized in clinical hepatology, comparative outcome data remains limited. This study aimed to compare 1-year clinical outcomes between AIH-PBC and AIH-PSC overlap syndromes using a large, multicenter EHR database.
Methods: We used the TriNetX Global Collaborative Network to conduct a retrospective cohort study. Cohort 1 included 6,654 patients with AIH-PBC overlap; cohort 2 included 1,994 with AIH-PSC overlap. Propensity score matching (1:1) was performed using a greedy nearest-neighbor algorithm (caliper: 0.1 SD), balancing age, sex, race, comorbidities (e.g., diabetes, obesity, cardiovascular disease), nicotine use, and NSAID exposure. This yielded 1,592 patients in each group. Outcomes assessed over 1 year post-index included mortality, cirrhosis, portal vein thrombosis (PVT), liver transplantation, cholangiocarcinoma, and hepatocellular carcinoma (HCC). Odds ratios (OR) with 95% confidence intervals (CI) were used for comparison.
Results: After matching cohorts , the AIH-PBC group had significantly lower odds of cirrhosis (OR 0.688, 95% CI 0.553–0.855, p=0.001), cholangiocarcinoma (OR 0.418, 95% CI 0.243–0.719, p=0.001), and all-cause mortality (OR 0.806, 95% CI 0.653–0.993, p=0.043) compared to the AIH-PSC group. No significant differences were observed for PVT (OR 0.827, p=0.254), liver transplantation (OR 0.931, p=0.585), or HCC (OR 1.002, p=0.997).
Discussion: Patients with AIH-PBC overlap syndrome experienced significantly lower risks of cirrhosis, mortality, and particularly cholangiocarcinoma compared to those with AIH-PSC, highlighting the more favorable prognosis associated with AIH-PBC. In contrast, the AIH-PSC phenotype appears to follow a more aggressive clinical course, which reinforces the importance of early recognition, close monitoring, and timely intervention in this subgroup. These findings support the need for risk-stratified surveillance strategies and may help inform therapeutic decision-making. Further prospective studies are essential to validate these observations and explore underlying pathophysiologic differences.
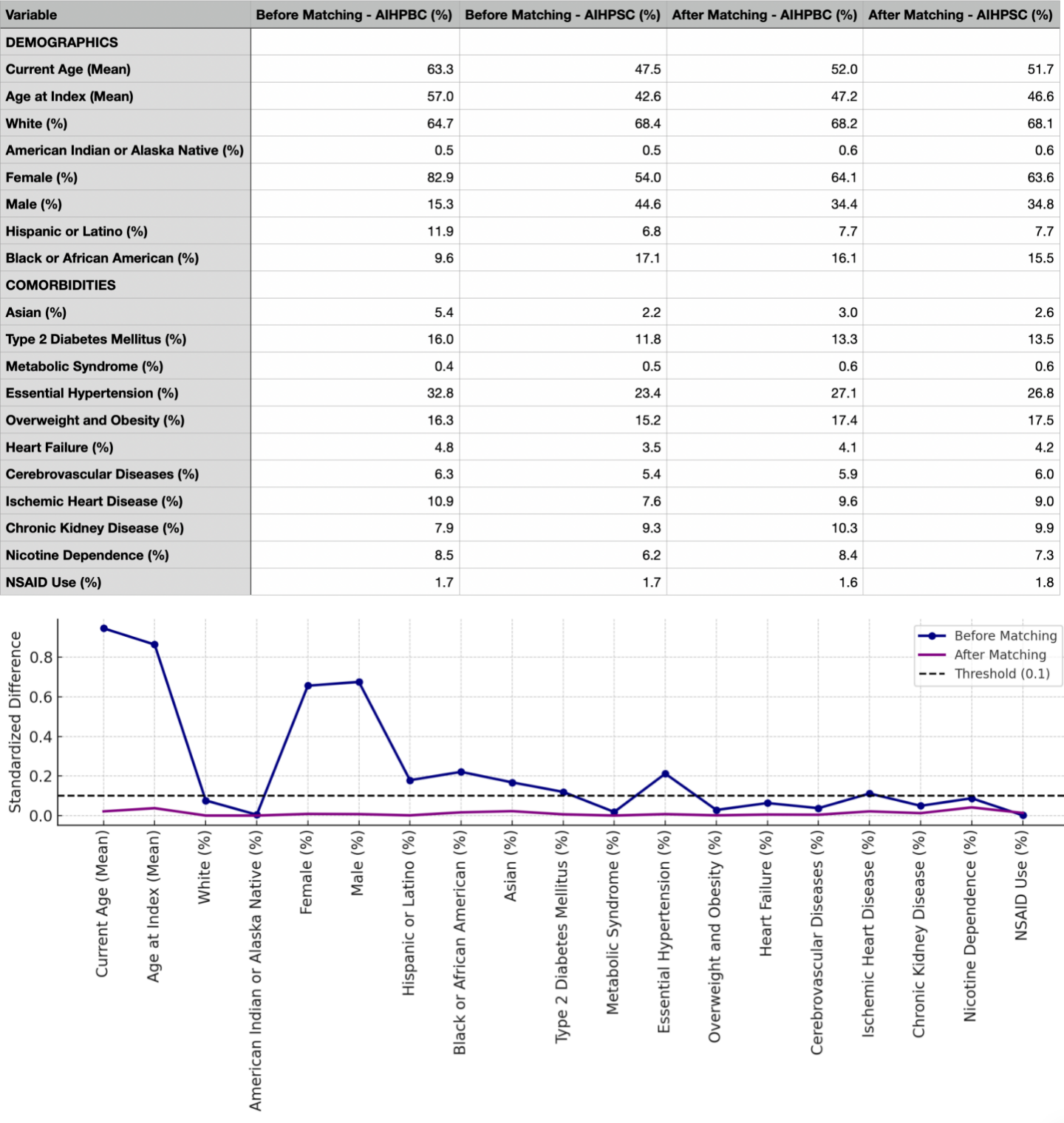
Figure: Figure 1: Baseline Characteristics of the Study Population and Standardized Mean Differences Before and After Propensity Score Matching,
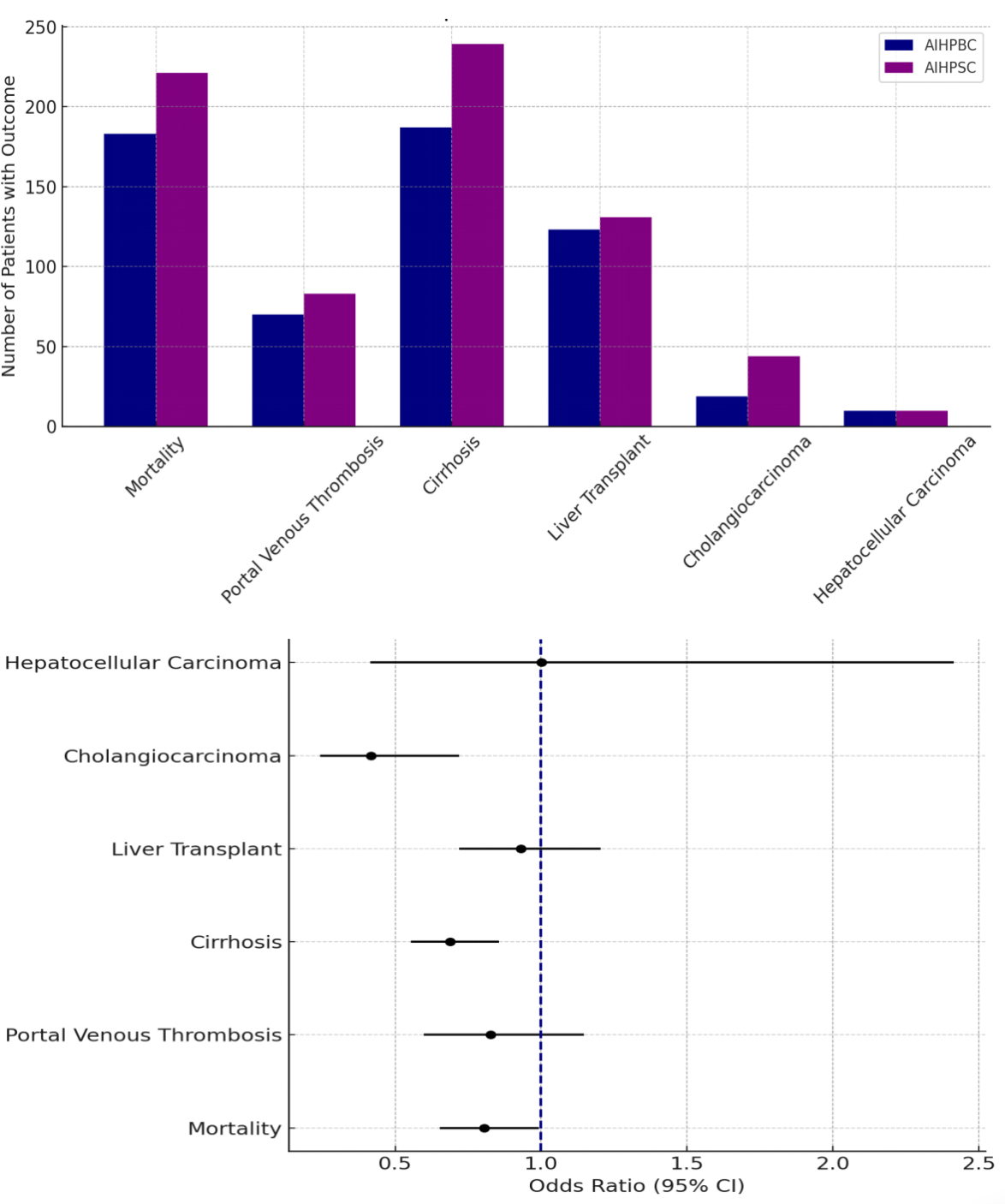
Figure: Figure 2: Comparative Outcomes Between AIH-PBC and AIH-PSC Groups, Including Forest Plot of Odds Ratios
Disclosures:
Chidera Onwuzo indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Emmanuel Otabor indicated no relevant financial relationships.
Alvina indicated no relevant financial relationships.
Laith Alomari indicated no relevant financial relationships.
Vishal Busa indicated no relevant financial relationships.
Chidera Onwuzo, MBBS1, Somtochukwu Onwuzo, MD2, Kojo-Frimpong B. Awuah, MD3, Rashid Abdel-Razeq, MD4, Emmanuel Otabor, MBBS5, Alvina, MD1, Laith Alomari, MD5, Vishal Busa, MD1. P3690 - Autoimmune Hepatitis Overlaps: One-Year Outcome Differences Between PBC and PSC Variants, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
