Monday Poster Session
Category: Liver
P3660 - Impact of Metabolic Liver Disease on Clinical Outcomes of Intrahepatic Cholangiocarcinoma
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Eugene Annor, MD, MPH
University of Illinois College of Medicine
Morton, IL
Presenting Author(s)
Eugene Annor, MD, MPH1, Nneoma Ubah, MD, MPH2, Chidiebube Ugwu, MD, MPH3, Joseph A. Atarere, MBChB, MPH4, Yusuf Kagzi, MD5, Salman Ahsan, MD5, Sonu Dhillon, MD5
1University of Illinois College of Medicine, Morton, IL; 2Montefiore St. Luke's, Newburgh, NY; 3Jefferson Health, Philadelphia, PA; 4MedStar Georgetown University Hospital, Baltimore, MD; 5University of Illinois College of Medicine, Peoria, IL
Introduction: Non-alcoholic fatty liver disease (NAFLD) is an increasingly prevalent condition associated with metabolic syndrome and chronic liver injury. Non-alcoholic steatohepatitis (NASH) represents a more severe, inflammatory subtype of NAFLD that accelerates hepatic fibrosis. NAFLD and NASH are known risk factors for liver disease progression. However, there is limited data on the impact of NAFLD and NASH on intrahepatic cholangiocarcinoma (IHCC) outcomes. This study aimed to compare clinical outcomes in IHCC patients with and without NAFLD/NASH using a large, real-world patient population.
Methods: A retrospective cohort study was conducted using TriNetX which provides de-identified real-world data from electronic medical records. Patients with alcoholic fatty liver disease, viral hepatitis of any type and autoimmune hepatitis were excluded. Adults (≥18 years) diagnosed with IHCC were identified and divided into two cohorts: patients with NAFLD/NASH (11,914) and those without it (24,028) with 9443 in each group after propensity score matching by age, race, body mass index (BMI), hypertension and diabetes mellitus. Outcomes assessed included cirrhosis, fibrosis, mortality, and hospitalization. Risk ratio (RR), 95% Confidence interval, hazard ratios and p-values were calculated. Kaplan-Meier survival analysis was also done. Data analysis was done using the TrinetX platform.
Results: Mean ages for IHCC and NAFLD/NASH vs IHCC alone were 67.3 ± 11.7 years and 67.4 ± 12.6 years respectively. Patients with IHCC and NAFLD/NASH had a significantly higher risk of developing cirrhosis (RR = 2.18; 95% CI: 1.92–2.48; p < 0.001) and hepatic fibrosis (RR = 3.08; 95% CI: 2.47–3.84; p < 0.001), as well as increased hospitalization rates (RR = 1.14; 95% CI: 1.08–1.20; p < 0.001) compared to patients with IHCC without NAFLD/NASH. However, there was no statistically significant difference in mortality between the two groups (RR = 1.04; 95% CI: 0.96–1.12; p = 0.35). Kaplan-Meier analysis showed comparable survival between the two groups (76.59% vs 67.14%; HR = 0.83; p=0.79).
Discussion: NAFLD/NASH in patients with IHCC patients is associated with increased risk of cirrhosis, fibrosis, and hospitalization, but not with increased mortality. These findings highlight the impact of NAFLD/NASH on clinical outcomes in patients with IHCC and may help guide treatment strategies.
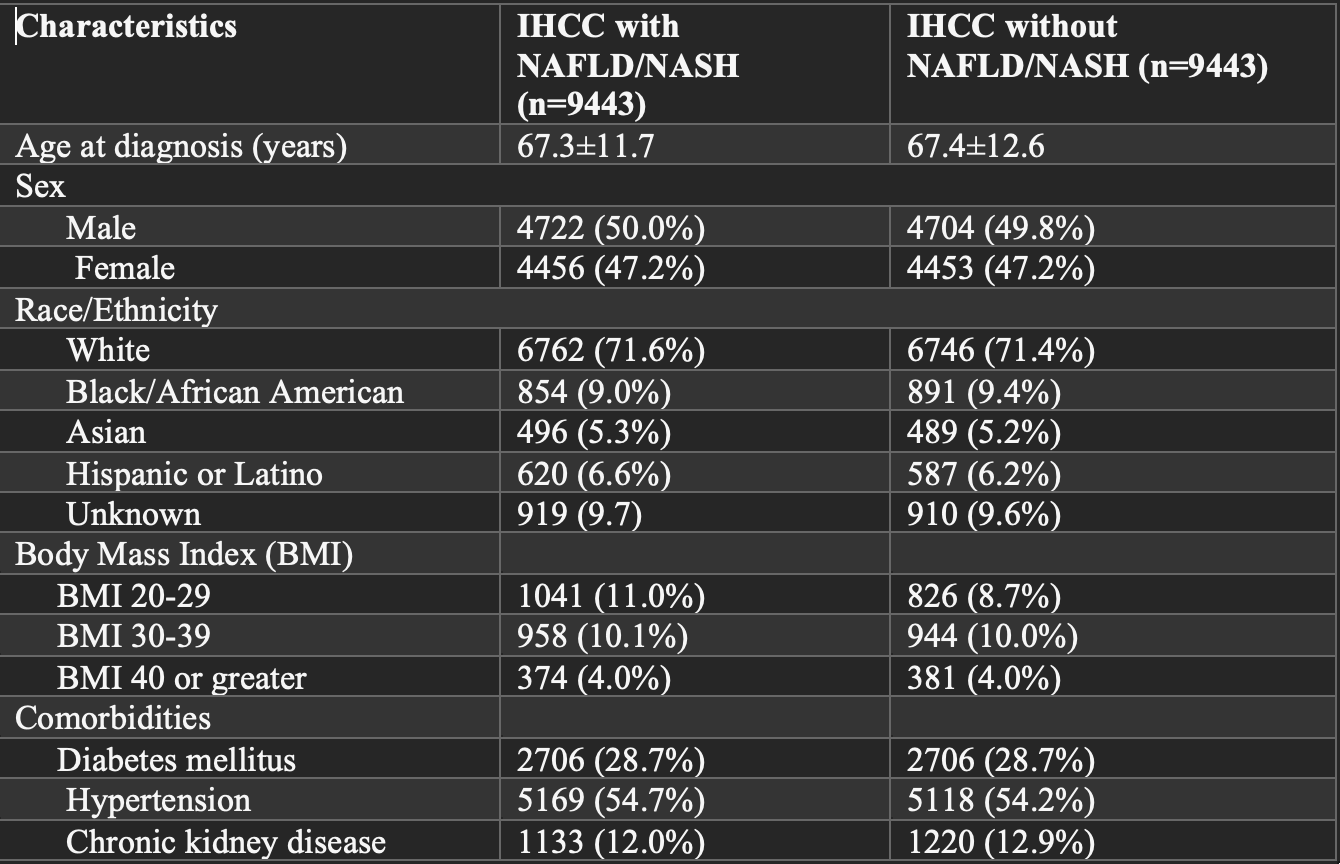
Figure: Table 1: Baseline Characteristics of Study Participants after Propensity Matching
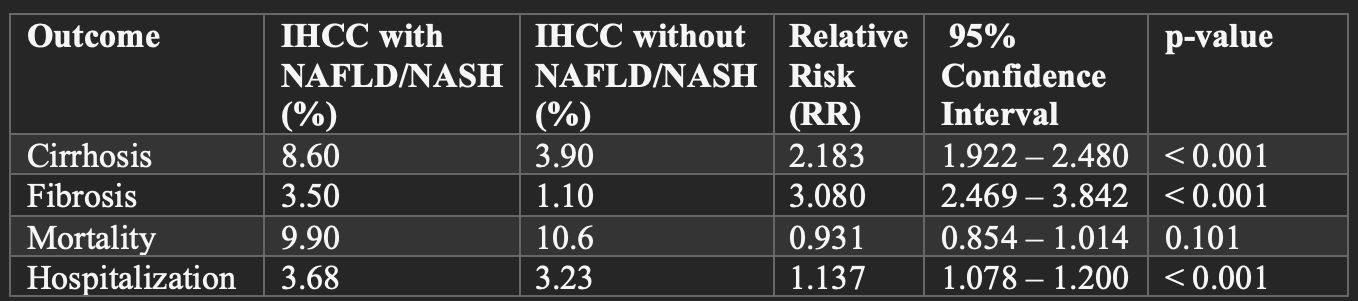
Figure: Table 2: Incidence and Risk of Clinical outcomes of IHCC and NAFLD/NASH and IHCC alone
Disclosures:
Eugene Annor indicated no relevant financial relationships.
Nneoma Ubah indicated no relevant financial relationships.
Chidiebube Ugwu indicated no relevant financial relationships.
Joseph Atarere indicated no relevant financial relationships.
Yusuf Kagzi indicated no relevant financial relationships.
Salman Ahsan indicated no relevant financial relationships.
Sonu Dhillon indicated no relevant financial relationships.
Eugene Annor, MD, MPH1, Nneoma Ubah, MD, MPH2, Chidiebube Ugwu, MD, MPH3, Joseph A. Atarere, MBChB, MPH4, Yusuf Kagzi, MD5, Salman Ahsan, MD5, Sonu Dhillon, MD5. P3660 - Impact of Metabolic Liver Disease on Clinical Outcomes of Intrahepatic Cholangiocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Illinois College of Medicine, Morton, IL; 2Montefiore St. Luke's, Newburgh, NY; 3Jefferson Health, Philadelphia, PA; 4MedStar Georgetown University Hospital, Baltimore, MD; 5University of Illinois College of Medicine, Peoria, IL
Introduction: Non-alcoholic fatty liver disease (NAFLD) is an increasingly prevalent condition associated with metabolic syndrome and chronic liver injury. Non-alcoholic steatohepatitis (NASH) represents a more severe, inflammatory subtype of NAFLD that accelerates hepatic fibrosis. NAFLD and NASH are known risk factors for liver disease progression. However, there is limited data on the impact of NAFLD and NASH on intrahepatic cholangiocarcinoma (IHCC) outcomes. This study aimed to compare clinical outcomes in IHCC patients with and without NAFLD/NASH using a large, real-world patient population.
Methods: A retrospective cohort study was conducted using TriNetX which provides de-identified real-world data from electronic medical records. Patients with alcoholic fatty liver disease, viral hepatitis of any type and autoimmune hepatitis were excluded. Adults (≥18 years) diagnosed with IHCC were identified and divided into two cohorts: patients with NAFLD/NASH (11,914) and those without it (24,028) with 9443 in each group after propensity score matching by age, race, body mass index (BMI), hypertension and diabetes mellitus. Outcomes assessed included cirrhosis, fibrosis, mortality, and hospitalization. Risk ratio (RR), 95% Confidence interval, hazard ratios and p-values were calculated. Kaplan-Meier survival analysis was also done. Data analysis was done using the TrinetX platform.
Results: Mean ages for IHCC and NAFLD/NASH vs IHCC alone were 67.3 ± 11.7 years and 67.4 ± 12.6 years respectively. Patients with IHCC and NAFLD/NASH had a significantly higher risk of developing cirrhosis (RR = 2.18; 95% CI: 1.92–2.48; p < 0.001) and hepatic fibrosis (RR = 3.08; 95% CI: 2.47–3.84; p < 0.001), as well as increased hospitalization rates (RR = 1.14; 95% CI: 1.08–1.20; p < 0.001) compared to patients with IHCC without NAFLD/NASH. However, there was no statistically significant difference in mortality between the two groups (RR = 1.04; 95% CI: 0.96–1.12; p = 0.35). Kaplan-Meier analysis showed comparable survival between the two groups (76.59% vs 67.14%; HR = 0.83; p=0.79).
Discussion: NAFLD/NASH in patients with IHCC patients is associated with increased risk of cirrhosis, fibrosis, and hospitalization, but not with increased mortality. These findings highlight the impact of NAFLD/NASH on clinical outcomes in patients with IHCC and may help guide treatment strategies.
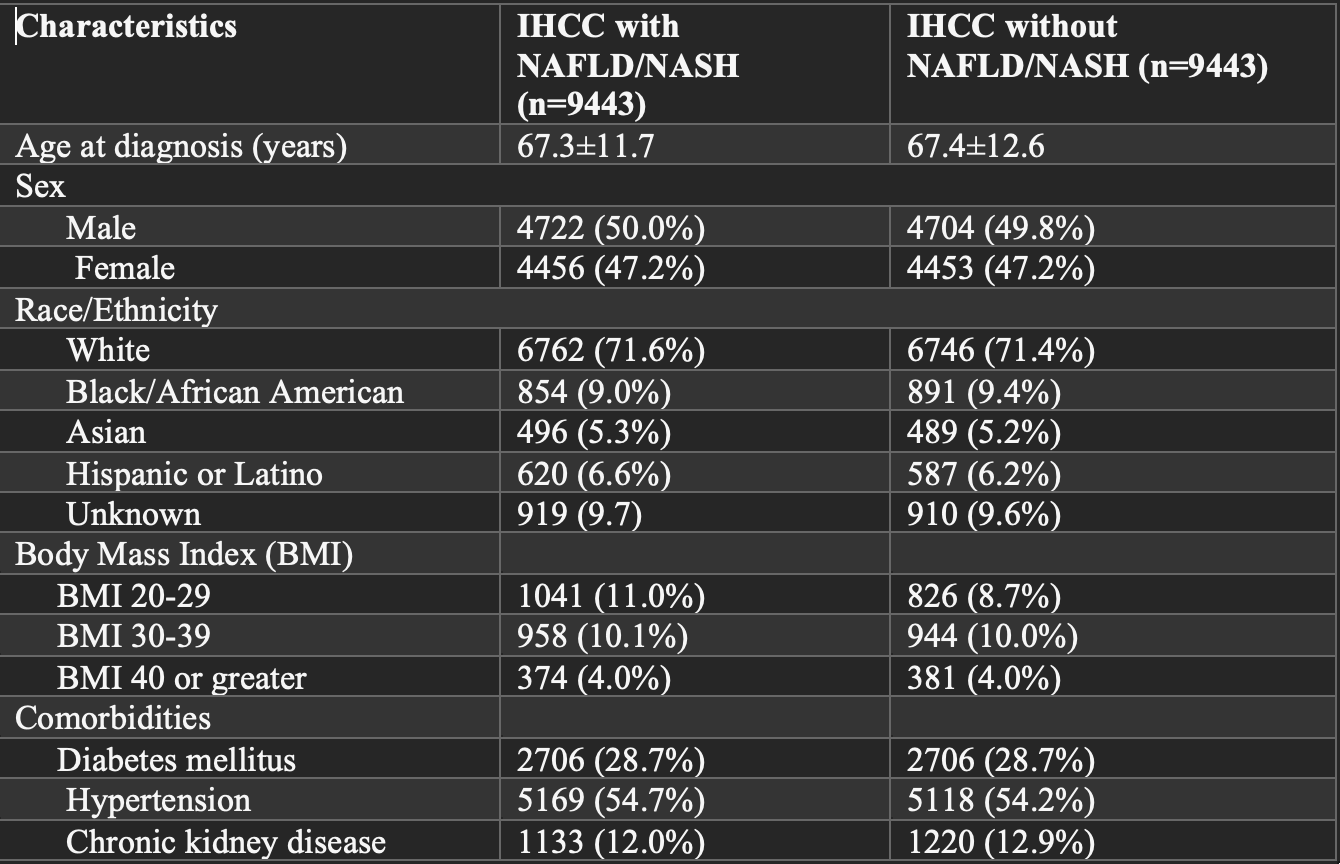
Figure: Table 1: Baseline Characteristics of Study Participants after Propensity Matching
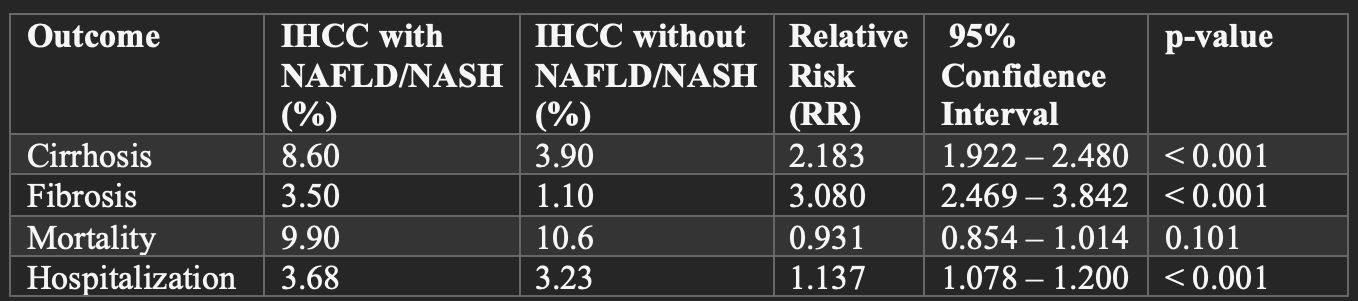
Figure: Table 2: Incidence and Risk of Clinical outcomes of IHCC and NAFLD/NASH and IHCC alone
Disclosures:
Eugene Annor indicated no relevant financial relationships.
Nneoma Ubah indicated no relevant financial relationships.
Chidiebube Ugwu indicated no relevant financial relationships.
Joseph Atarere indicated no relevant financial relationships.
Yusuf Kagzi indicated no relevant financial relationships.
Salman Ahsan indicated no relevant financial relationships.
Sonu Dhillon indicated no relevant financial relationships.
Eugene Annor, MD, MPH1, Nneoma Ubah, MD, MPH2, Chidiebube Ugwu, MD, MPH3, Joseph A. Atarere, MBChB, MPH4, Yusuf Kagzi, MD5, Salman Ahsan, MD5, Sonu Dhillon, MD5. P3660 - Impact of Metabolic Liver Disease on Clinical Outcomes of Intrahepatic Cholangiocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
