Monday Poster Session
Category: Liver
P3657 - Prevalence of Osteoporosis and Screening Compliance in Primary Biliary Cholangitis: A Multicenter Matched Cohort
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Leandro Sierra, MD (he/him/his)
Department of Internal Medicine, Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Leandro Sierra, MD1, Hussam Kawas, MD2, Rachel McNulty, MD3, Sara Valencia, MD2, Juan Armijos, MD4, Xaralambos Zervos, DO4, Omar Sims, PhD5, John McMichael, PhD2, Dian Jung Chiang, MD6
1Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic Akron General, Akron, OH; 4Cleveland Clinic Florida, Weston, FL; 5Cleveland Clinic Foundation, Hoover, AL; 6Cleveland Clinic, Cleveland, OH
Introduction: Osteoporosis is one of the most common extrahepatic complications of primary biliary cholangitis (PBC). Dual-energy X-ray absorptiometry (DXA) is recommended at the time of PBC diagnosis and every two years thereafter There is limited data on screening compliance and risk of osteoporosis in PBC.
Methods: We performed a retrospective study (2005 –2025) using data from two large tertiary referral centers in the US. Adults meeting AASLD criteria for PBC were identified and stratified by age upon PBC diagnosis (< 65 years vs. ≥65 years). Patients with prior liver transplant, cirrhosis, or non-PBC liver disease were excluded. The primary outcome was DXA screening compliance rate. The secondary outcomes were DXA surveillance rate after initial screening DXA and prevalence of osteoporosis across age groups. A control cohort of postmenopausal women (≥ 65 years) without PBC was selected as controls, using coarsened exact matching (CEM) on age, BMI, and race for the comparison.
Results: In our cohort, 219 patients were diagnosed with PBC before 65 years old and 206 patients were diagnosed at or after 65 years old. Prevalence of osteoporosis did not differ significantly between early and late-onset PBC groups (35.0% vs 39.6%, p > 0.05), nor did osteopenia rates (59.5% vs 52.8%, p > 0.05). Baseline DXA screening was lower in PBC patients with early-onset PBC vs late-onset PBC (44% vs 55%, p = 0.03), while the surveillance rate (22% vs 27%, p > 0.05) and median interval to surveillance DXA (3.3 vs 3.5 years, p > 0.05) were similar. In the CEM-matched cohort of 206 late-onset PBC patients and 422 postmenopausal controls, the compliance of DXA screening was comparable though PBC patients had a higher osteoporosis risk compared to postmenopausal controls (39.6% vs 29.7%, p = 0.05).
Discussion: The prevalence of osteoporosis is high among PBC patients across age of PBC diagnosis. Compliance to DXA screening at time of PBC diagnosis and surveillance afterwards remains low, especially in patients diagnosed with PBC at a younger age (age < 65 years old). However, our data revealed comparable osteoporosis burden across PBC age groups and a significantly higher prevalence of osteoporosis than age-matched post-menopausal controls. DXA surveillance was also underutilized in PBC patients in our study. These findings underscore suboptimal osteoporosis screening and surveillance in PBC patients. Further studies to identify barriers to screening and surveillance is needed to improve care in this population.
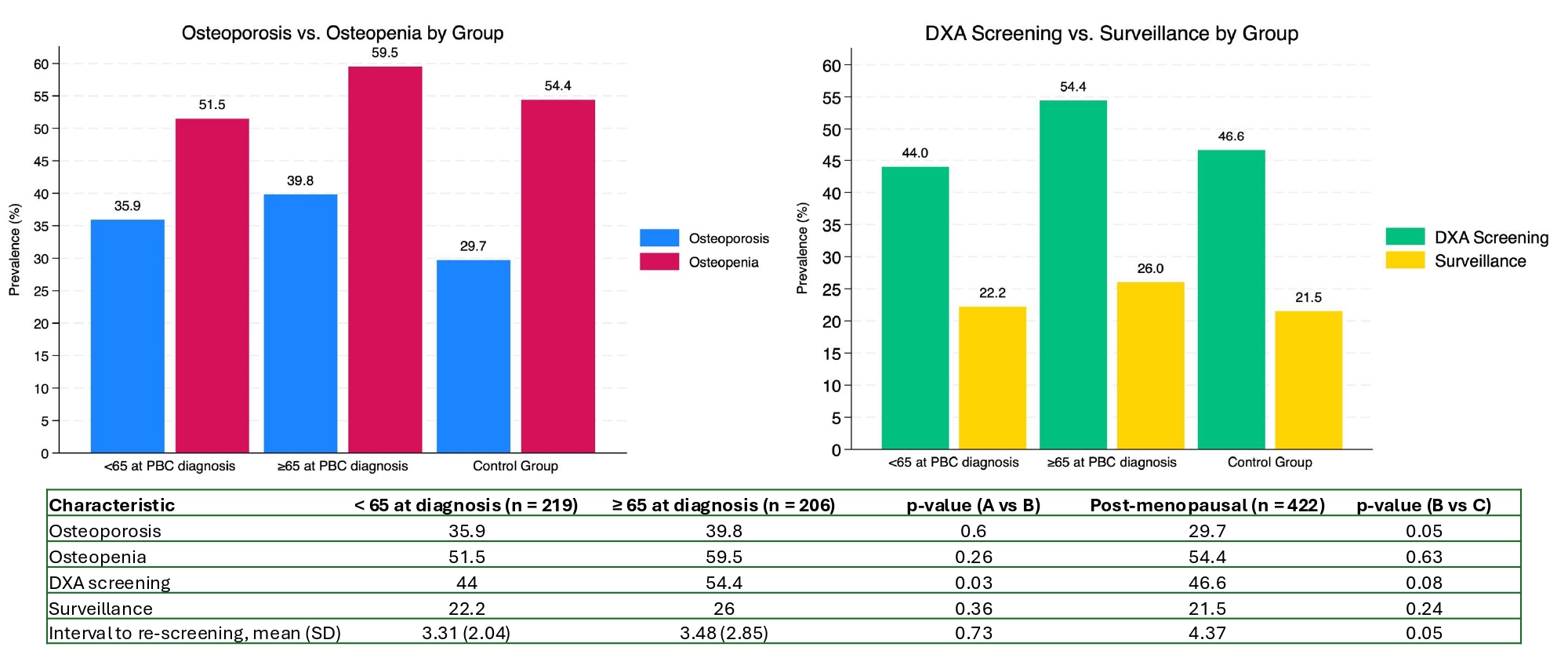
Figure: Osteoporosis and osteopenia prevalence and DXA screening and surveillance in primary biliary cholangitis vs. controls
Disclosures:
Leandro Sierra indicated no relevant financial relationships.
Hussam Kawas indicated no relevant financial relationships.
Rachel McNulty indicated no relevant financial relationships.
Sara Valencia indicated no relevant financial relationships.
Juan Armijos indicated no relevant financial relationships.
Xaralambos Zervos indicated no relevant financial relationships.
Omar Sims indicated no relevant financial relationships.
John McMichael indicated no relevant financial relationships.
Dian Jung Chiang: Ipsen – Advisory Committee/Board Member.
Leandro Sierra, MD1, Hussam Kawas, MD2, Rachel McNulty, MD3, Sara Valencia, MD2, Juan Armijos, MD4, Xaralambos Zervos, DO4, Omar Sims, PhD5, John McMichael, PhD2, Dian Jung Chiang, MD6. P3657 - Prevalence of Osteoporosis and Screening Compliance in Primary Biliary Cholangitis: A Multicenter Matched Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Cleveland Clinic Akron General, Akron, OH; 4Cleveland Clinic Florida, Weston, FL; 5Cleveland Clinic Foundation, Hoover, AL; 6Cleveland Clinic, Cleveland, OH
Introduction: Osteoporosis is one of the most common extrahepatic complications of primary biliary cholangitis (PBC). Dual-energy X-ray absorptiometry (DXA) is recommended at the time of PBC diagnosis and every two years thereafter There is limited data on screening compliance and risk of osteoporosis in PBC.
Methods: We performed a retrospective study (2005 –2025) using data from two large tertiary referral centers in the US. Adults meeting AASLD criteria for PBC were identified and stratified by age upon PBC diagnosis (< 65 years vs. ≥65 years). Patients with prior liver transplant, cirrhosis, or non-PBC liver disease were excluded. The primary outcome was DXA screening compliance rate. The secondary outcomes were DXA surveillance rate after initial screening DXA and prevalence of osteoporosis across age groups. A control cohort of postmenopausal women (≥ 65 years) without PBC was selected as controls, using coarsened exact matching (CEM) on age, BMI, and race for the comparison.
Results: In our cohort, 219 patients were diagnosed with PBC before 65 years old and 206 patients were diagnosed at or after 65 years old. Prevalence of osteoporosis did not differ significantly between early and late-onset PBC groups (35.0% vs 39.6%, p > 0.05), nor did osteopenia rates (59.5% vs 52.8%, p > 0.05). Baseline DXA screening was lower in PBC patients with early-onset PBC vs late-onset PBC (44% vs 55%, p = 0.03), while the surveillance rate (22% vs 27%, p > 0.05) and median interval to surveillance DXA (3.3 vs 3.5 years, p > 0.05) were similar. In the CEM-matched cohort of 206 late-onset PBC patients and 422 postmenopausal controls, the compliance of DXA screening was comparable though PBC patients had a higher osteoporosis risk compared to postmenopausal controls (39.6% vs 29.7%, p = 0.05).
Discussion: The prevalence of osteoporosis is high among PBC patients across age of PBC diagnosis. Compliance to DXA screening at time of PBC diagnosis and surveillance afterwards remains low, especially in patients diagnosed with PBC at a younger age (age < 65 years old). However, our data revealed comparable osteoporosis burden across PBC age groups and a significantly higher prevalence of osteoporosis than age-matched post-menopausal controls. DXA surveillance was also underutilized in PBC patients in our study. These findings underscore suboptimal osteoporosis screening and surveillance in PBC patients. Further studies to identify barriers to screening and surveillance is needed to improve care in this population.
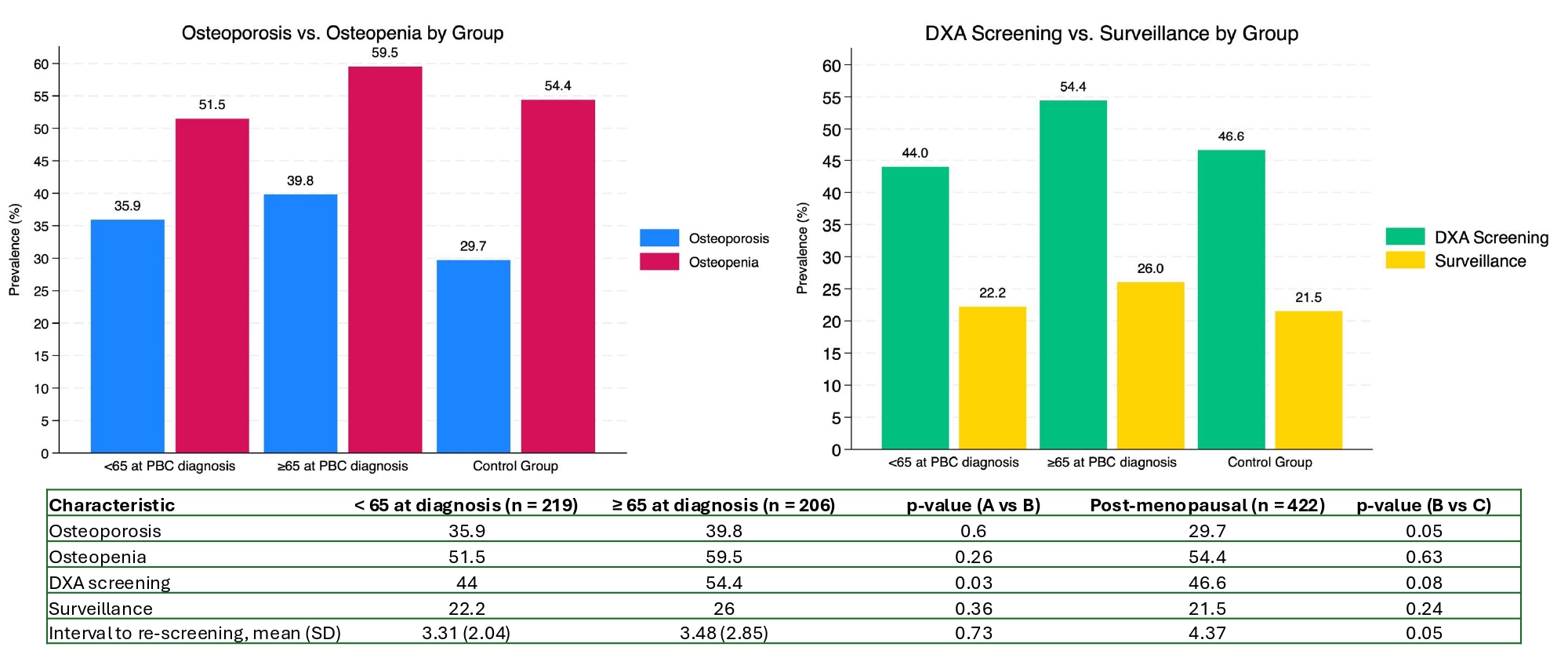
Figure: Osteoporosis and osteopenia prevalence and DXA screening and surveillance in primary biliary cholangitis vs. controls
Disclosures:
Leandro Sierra indicated no relevant financial relationships.
Hussam Kawas indicated no relevant financial relationships.
Rachel McNulty indicated no relevant financial relationships.
Sara Valencia indicated no relevant financial relationships.
Juan Armijos indicated no relevant financial relationships.
Xaralambos Zervos indicated no relevant financial relationships.
Omar Sims indicated no relevant financial relationships.
John McMichael indicated no relevant financial relationships.
Dian Jung Chiang: Ipsen – Advisory Committee/Board Member.
Leandro Sierra, MD1, Hussam Kawas, MD2, Rachel McNulty, MD3, Sara Valencia, MD2, Juan Armijos, MD4, Xaralambos Zervos, DO4, Omar Sims, PhD5, John McMichael, PhD2, Dian Jung Chiang, MD6. P3657 - Prevalence of Osteoporosis and Screening Compliance in Primary Biliary Cholangitis: A Multicenter Matched Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

