Monday Poster Session
Category: Liver
P3656 - Underuse of GLP-1 Receptor Agonists Despite Promising Evidence in Managing Post-Liver Transplant Alcohol Recidivism in Alcohol Associated Liver Disease
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Leandro Sierra, MD (he/him/his)
Department of Internal Medicine, Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Leandro Sierra, MD1, Himsikhar Khataniar, MD2, Renuka Verma, MD3, Mohamad Mahdi Osman, DO4, Sajid Jalil, MD5, Nikki Duong, MD6
1Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 2Allegheny General Hospital, Pittsburgh, PA; 3Allegheny Health Network, Pittsburgh, PA; 4Cleveland Clinic, Cleveland, OH; 5Stanford University, Palo Alto, CA; 6Stanford University, Stanford, CA
Introduction: Alcohol-related liver disease (ALD) is the leading indication for liver transplantation in the US, yet relapse occurs in up to 20% of patients. Recent studies suggest that incretin-based therapies (IBTs), particularly glucagon-like peptide-1 receptor agonists (GLP-1 RA), may modulate the dopamine reward pathway and enhance central gamma-aminobutyric acid (GABA) release, potentially mitigating AUD recurrence.
This study aims to characterize the prevalence of GLP-1 RA initiation post-liver transplant in patients with ALD and assess its potential association with AUD recurrence.
Methods: This case series utilized data from a single center tertiary U.S. transplant center and evaluated adult patients diagnosed with ALD who underwent liver transplantation between 2015 and 2025. Patients with other liver diseases, malignancies, prior organ transplants, or usage of dipeptidyl peptidase-4 inhibitors or sodium-glucose cotransporter-2 inhibitors were excluded. Primary outcomes included alcohol-related diagnoses (dependence, abuse, or any use), ALD recurrence, transplant rejection, and initiation of GLP-1 RA therapy within 1 month to 5 years post-transplant.
Results: Among 802 patients (mean age 53.7 years; 33.9% female; mean Charlson comorbidity score 5.6), 46.5% experienced ALD recurrence, 48.9% had documented alcohol use, 37.2% had alcohol dependence, and 21.6% had documented alcohol abuse. Transplant rejection occurred in 15.8% of cases, with 7.0% developing graft failure requiring re-transplant.
Despite robust preclinical evidence supporting the potential role of GLP-1RA in managing AUD, only 1.5% (n=12) of the cohort received GLP-1 RA therapy within one-year post-transplant. Among them, only 0.5% (n=4) had documented alcohol use after initiating GLP-1 RA therapy.
Discussion: Recurrence of AUD and related complications post-transplant remains a significant burden among patients with ALD. Although data exists supporting the use of GLP-1 RA, there is a strikingly low prevalence of GLP-1 RA utilization. These findings underscore a missed opportunity and support the need for future prospective studies to evaluate the benefit of GLP-1 RAs in reducing alcohol relapse after transplant.
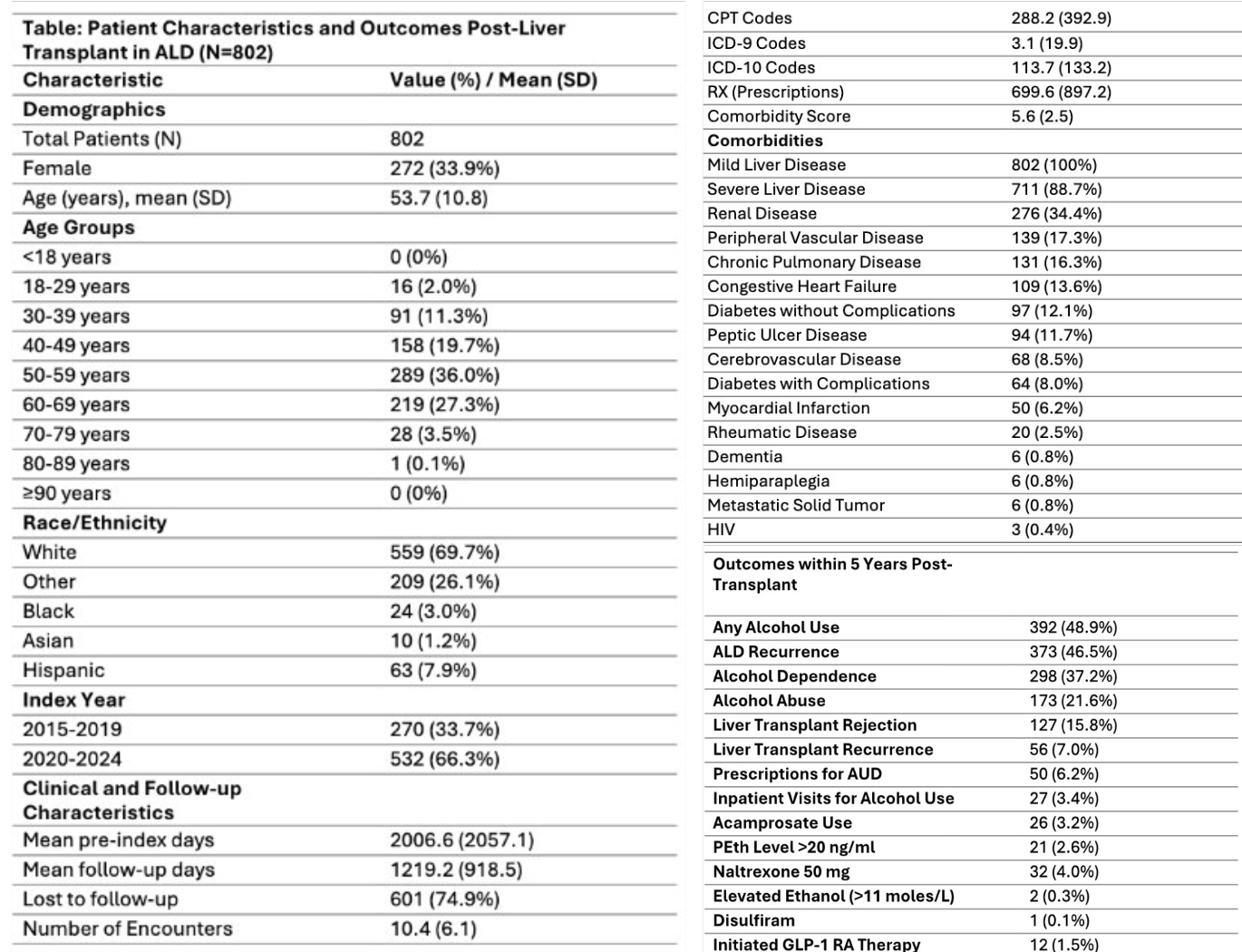
Figure: Patient Characteristics and Outcomes Post-Liver Transplant in ALD
Disclosures:
Leandro Sierra indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Renuka Verma indicated no relevant financial relationships.
Mohamad Mahdi Osman indicated no relevant financial relationships.
Sajid Jalil indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Leandro Sierra, MD1, Himsikhar Khataniar, MD2, Renuka Verma, MD3, Mohamad Mahdi Osman, DO4, Sajid Jalil, MD5, Nikki Duong, MD6. P3656 - Underuse of GLP-1 Receptor Agonists Despite Promising Evidence in Managing Post-Liver Transplant Alcohol Recidivism in Alcohol Associated Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 2Allegheny General Hospital, Pittsburgh, PA; 3Allegheny Health Network, Pittsburgh, PA; 4Cleveland Clinic, Cleveland, OH; 5Stanford University, Palo Alto, CA; 6Stanford University, Stanford, CA
Introduction: Alcohol-related liver disease (ALD) is the leading indication for liver transplantation in the US, yet relapse occurs in up to 20% of patients. Recent studies suggest that incretin-based therapies (IBTs), particularly glucagon-like peptide-1 receptor agonists (GLP-1 RA), may modulate the dopamine reward pathway and enhance central gamma-aminobutyric acid (GABA) release, potentially mitigating AUD recurrence.
This study aims to characterize the prevalence of GLP-1 RA initiation post-liver transplant in patients with ALD and assess its potential association with AUD recurrence.
Methods: This case series utilized data from a single center tertiary U.S. transplant center and evaluated adult patients diagnosed with ALD who underwent liver transplantation between 2015 and 2025. Patients with other liver diseases, malignancies, prior organ transplants, or usage of dipeptidyl peptidase-4 inhibitors or sodium-glucose cotransporter-2 inhibitors were excluded. Primary outcomes included alcohol-related diagnoses (dependence, abuse, or any use), ALD recurrence, transplant rejection, and initiation of GLP-1 RA therapy within 1 month to 5 years post-transplant.
Results: Among 802 patients (mean age 53.7 years; 33.9% female; mean Charlson comorbidity score 5.6), 46.5% experienced ALD recurrence, 48.9% had documented alcohol use, 37.2% had alcohol dependence, and 21.6% had documented alcohol abuse. Transplant rejection occurred in 15.8% of cases, with 7.0% developing graft failure requiring re-transplant.
Despite robust preclinical evidence supporting the potential role of GLP-1RA in managing AUD, only 1.5% (n=12) of the cohort received GLP-1 RA therapy within one-year post-transplant. Among them, only 0.5% (n=4) had documented alcohol use after initiating GLP-1 RA therapy.
Discussion: Recurrence of AUD and related complications post-transplant remains a significant burden among patients with ALD. Although data exists supporting the use of GLP-1 RA, there is a strikingly low prevalence of GLP-1 RA utilization. These findings underscore a missed opportunity and support the need for future prospective studies to evaluate the benefit of GLP-1 RAs in reducing alcohol relapse after transplant.
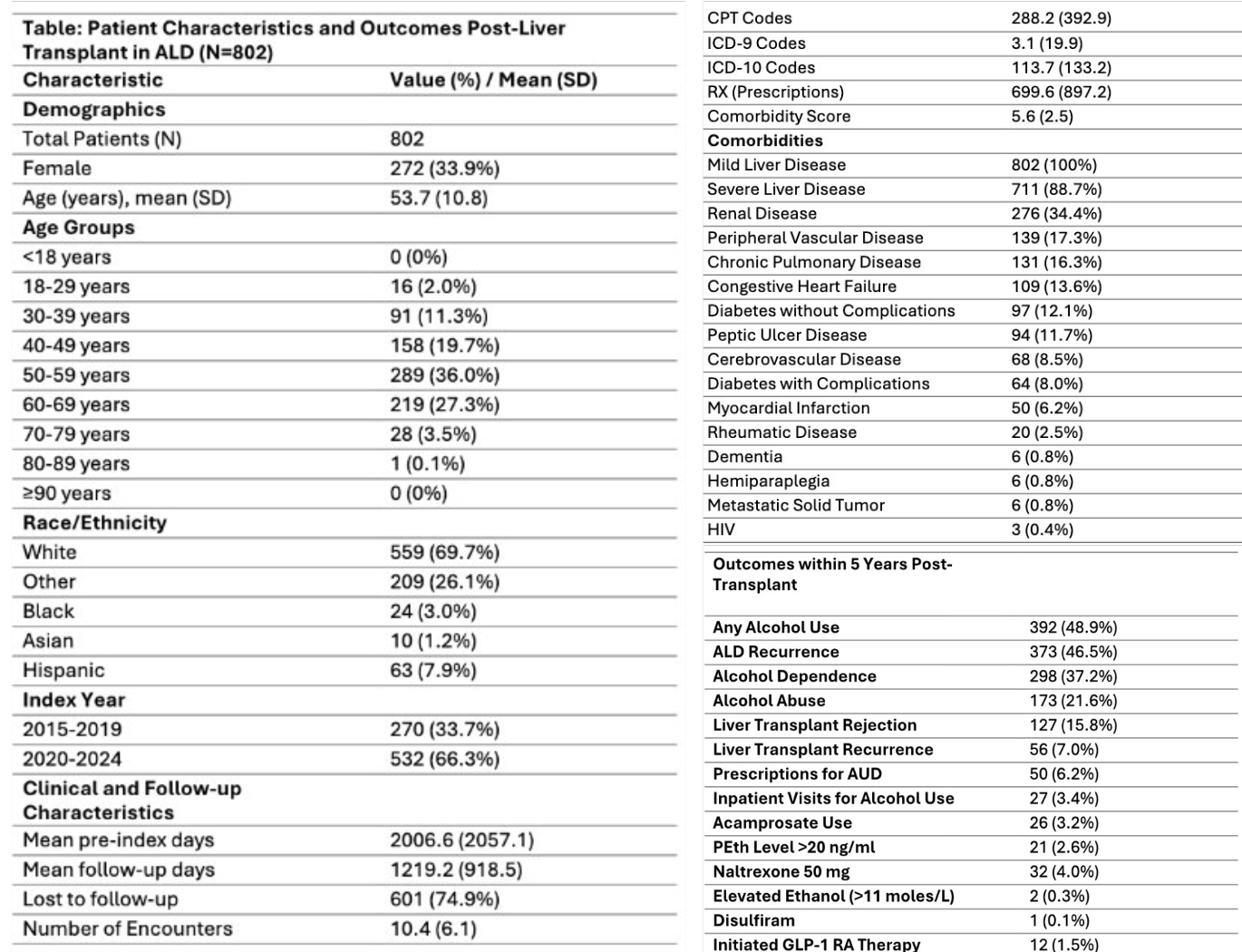
Figure: Patient Characteristics and Outcomes Post-Liver Transplant in ALD
Disclosures:
Leandro Sierra indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Renuka Verma indicated no relevant financial relationships.
Mohamad Mahdi Osman indicated no relevant financial relationships.
Sajid Jalil indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Leandro Sierra, MD1, Himsikhar Khataniar, MD2, Renuka Verma, MD3, Mohamad Mahdi Osman, DO4, Sajid Jalil, MD5, Nikki Duong, MD6. P3656 - Underuse of GLP-1 Receptor Agonists Despite Promising Evidence in Managing Post-Liver Transplant Alcohol Recidivism in Alcohol Associated Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
