Monday Poster Session
Category: Liver
P3626 - Comparison of Hepatocellular Carcinoma Risk in MASH vs MASLD With Normal Liver Enzymes: A Retrospective Cohort Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmad Abdulraheem, MD (he/him/his)
MedStar Washington Hospital Center-Georgetown University
Washington, DC
Presenting Author(s)
Ahmad Abdulraheem, MD1, Omar Abureesh, MD2, Abdellatif Ismail, MD3, Mohammed Aloqaily, MD4, Dania Qarkash, MD5, Spyros Peppas, MD1, Nadera Altork, MD1, Mohammed Al-Aquily, MD6, Laith Alomari, MD7, Seunghee Han, MBChB8, Emma Antall, 9, Won Cho, MD10
1MedStar Washington Hospital Center-Georgetown University, Washington, DC; 2Staten Island University Hospital, Northwell Health, Staten Island, NY; 3University of Maryland, Baltimore, MD; 4University of Maryland Medical Center Midtown Campus, Baltimore, MD; 5University of Jordan, Washington, DC; 6Norwalk Hospital/Yale University, Norwalk, CT; 7Thomas Jefferson University, Philadelphia, PA; 8MedStar Georgetown University Hospital, Baltimore, MD; 9MedStar Georgetown University Hospital, Washington, DC; 10Georgetown University School of Medicine, Washington, DC
Introduction: The incidence of hepatocellular carcinoma (HCC) in patients with metabolic dysfunction-associated steatotic liver disease (MASLD) is rising, including in those without cirrhosis or abnormal liver enzymes. Current AASLD guidelines recommend HCC surveillance every six months with ultrasound and AFP only for patients with cirrhosis or chronic hepatitis B. However, up to 30-40% of MASLD-related HCC cases occur in non-cirrhotic livers, challenging these guidelines. Although AFP alone has limited sensitivity and specificity, levels above 200-400 ng/mL may improve diagnostic accuracy when combined with imaging. This study compares HCC risk in patients with metabolic dysfunction-associated steatohepatitis (MASH) versus MASLD with normal liver enzymes.
Methods: A retrospective cohort study using the TriNetX US Collaborative Network included adults ≥18 years with MASH (elevated AST/ALT >30 U/L plus ≥1 metabolic risk factor: BMI >25, prediabetes/diabetes, hypertension, triglycerides >150 mg/dL, or HDL < 40 mg/dL) or MASLD (normal AST/ALT with the same metabolic criteria). Patients with other chronic liver diseases were excluded. Propensity score matching was done for age, sex, race, BMI, A1C, creatinine, and liver function tests. The primary outcome was HCC development; secondary outcomes were AFP >100 and >400 ng/mL. Statistical significance was set at p < 0.05.
Results: After propensity score matching, 342,391 patients in Cohort 1 and 342,464 in Cohort 2 were included Table 1. Mean age was 49.9 ± 14.8 vs. 50.0 ± 14.8 years, White patients 70.2% vs. 70.6%, and males 53.2% in both. HCC occurred in 0.088% of Cohort 1 versus 0.050% of Cohort 2 (OR 1.757; 95% CI: 1.457-2.119). AFP >100 ng/mL was found in 0.011% vs. 0.008% (OR 1.310; 95% CI: 0.808-2.125), and AFP >400 ng/mL in 0.006% vs. 0.004% (OR 1.538; 95% CI: 0.765-3.093).
Discussion: Our study showed that the cohort primarily consisted of middle-aged White male patients. Patients with MASH had a significantly higher risk of developing HCC, demonstrating a 1.8-fold increase compared to MASLD patients with normal liver enzymes. Although AFP elevations were more common in the MASH group, these differences did not reach statistical significance. These findings highlight the need for prospective studies to evaluate surveillance strategies in metabolically high-risk populations, incorporating demographic factors, metabolic disease severity, non-invasive fibrosis scores, and AFP levels to enhance risk stratification and enable early detection of HCC.
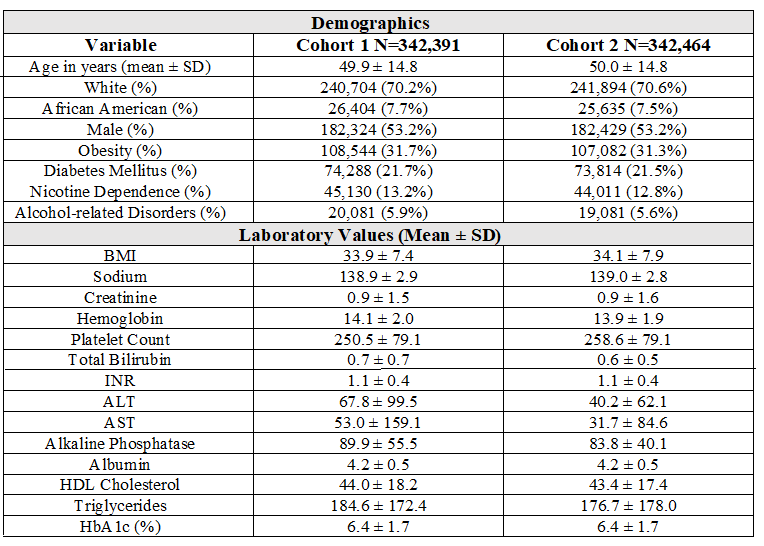
Figure: Table 1. Characteristics of Cohort 1 and Cohort 2 After Propensity Score Matching
Disclosures:
Ahmad Abdulraheem indicated no relevant financial relationships.
Omar Abureesh indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Mohammed Aloqaily indicated no relevant financial relationships.
Dania Qarkash indicated no relevant financial relationships.
Spyros Peppas indicated no relevant financial relationships.
Nadera Altork indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Laith Alomari indicated no relevant financial relationships.
Seunghee Han indicated no relevant financial relationships.
Emma Antall indicated no relevant financial relationships.
Won Cho indicated no relevant financial relationships.
Ahmad Abdulraheem, MD1, Omar Abureesh, MD2, Abdellatif Ismail, MD3, Mohammed Aloqaily, MD4, Dania Qarkash, MD5, Spyros Peppas, MD1, Nadera Altork, MD1, Mohammed Al-Aquily, MD6, Laith Alomari, MD7, Seunghee Han, MBChB8, Emma Antall, 9, Won Cho, MD10. P3626 - Comparison of Hepatocellular Carcinoma Risk in MASH vs MASLD With Normal Liver Enzymes: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1MedStar Washington Hospital Center-Georgetown University, Washington, DC; 2Staten Island University Hospital, Northwell Health, Staten Island, NY; 3University of Maryland, Baltimore, MD; 4University of Maryland Medical Center Midtown Campus, Baltimore, MD; 5University of Jordan, Washington, DC; 6Norwalk Hospital/Yale University, Norwalk, CT; 7Thomas Jefferson University, Philadelphia, PA; 8MedStar Georgetown University Hospital, Baltimore, MD; 9MedStar Georgetown University Hospital, Washington, DC; 10Georgetown University School of Medicine, Washington, DC
Introduction: The incidence of hepatocellular carcinoma (HCC) in patients with metabolic dysfunction-associated steatotic liver disease (MASLD) is rising, including in those without cirrhosis or abnormal liver enzymes. Current AASLD guidelines recommend HCC surveillance every six months with ultrasound and AFP only for patients with cirrhosis or chronic hepatitis B. However, up to 30-40% of MASLD-related HCC cases occur in non-cirrhotic livers, challenging these guidelines. Although AFP alone has limited sensitivity and specificity, levels above 200-400 ng/mL may improve diagnostic accuracy when combined with imaging. This study compares HCC risk in patients with metabolic dysfunction-associated steatohepatitis (MASH) versus MASLD with normal liver enzymes.
Methods: A retrospective cohort study using the TriNetX US Collaborative Network included adults ≥18 years with MASH (elevated AST/ALT >30 U/L plus ≥1 metabolic risk factor: BMI >25, prediabetes/diabetes, hypertension, triglycerides >150 mg/dL, or HDL < 40 mg/dL) or MASLD (normal AST/ALT with the same metabolic criteria). Patients with other chronic liver diseases were excluded. Propensity score matching was done for age, sex, race, BMI, A1C, creatinine, and liver function tests. The primary outcome was HCC development; secondary outcomes were AFP >100 and >400 ng/mL. Statistical significance was set at p < 0.05.
Results: After propensity score matching, 342,391 patients in Cohort 1 and 342,464 in Cohort 2 were included Table 1. Mean age was 49.9 ± 14.8 vs. 50.0 ± 14.8 years, White patients 70.2% vs. 70.6%, and males 53.2% in both. HCC occurred in 0.088% of Cohort 1 versus 0.050% of Cohort 2 (OR 1.757; 95% CI: 1.457-2.119). AFP >100 ng/mL was found in 0.011% vs. 0.008% (OR 1.310; 95% CI: 0.808-2.125), and AFP >400 ng/mL in 0.006% vs. 0.004% (OR 1.538; 95% CI: 0.765-3.093).
Discussion: Our study showed that the cohort primarily consisted of middle-aged White male patients. Patients with MASH had a significantly higher risk of developing HCC, demonstrating a 1.8-fold increase compared to MASLD patients with normal liver enzymes. Although AFP elevations were more common in the MASH group, these differences did not reach statistical significance. These findings highlight the need for prospective studies to evaluate surveillance strategies in metabolically high-risk populations, incorporating demographic factors, metabolic disease severity, non-invasive fibrosis scores, and AFP levels to enhance risk stratification and enable early detection of HCC.
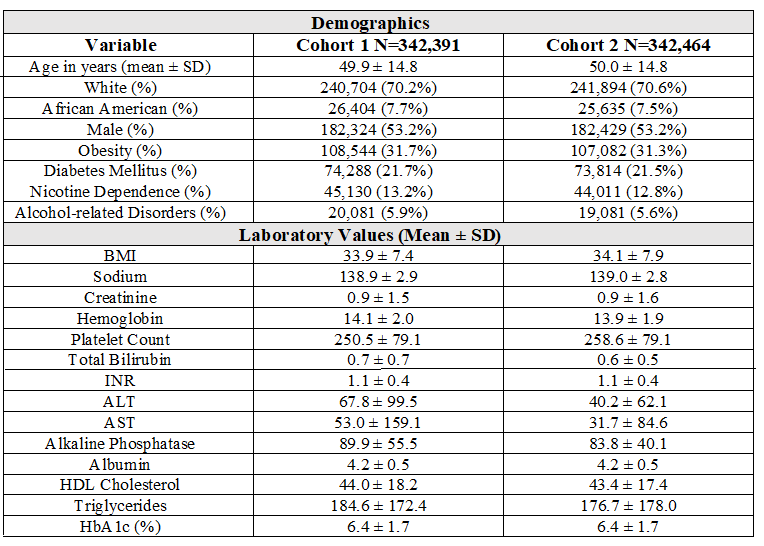
Figure: Table 1. Characteristics of Cohort 1 and Cohort 2 After Propensity Score Matching
Disclosures:
Ahmad Abdulraheem indicated no relevant financial relationships.
Omar Abureesh indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Mohammed Aloqaily indicated no relevant financial relationships.
Dania Qarkash indicated no relevant financial relationships.
Spyros Peppas indicated no relevant financial relationships.
Nadera Altork indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Laith Alomari indicated no relevant financial relationships.
Seunghee Han indicated no relevant financial relationships.
Emma Antall indicated no relevant financial relationships.
Won Cho indicated no relevant financial relationships.
Ahmad Abdulraheem, MD1, Omar Abureesh, MD2, Abdellatif Ismail, MD3, Mohammed Aloqaily, MD4, Dania Qarkash, MD5, Spyros Peppas, MD1, Nadera Altork, MD1, Mohammed Al-Aquily, MD6, Laith Alomari, MD7, Seunghee Han, MBChB8, Emma Antall, 9, Won Cho, MD10. P3626 - Comparison of Hepatocellular Carcinoma Risk in MASH vs MASLD With Normal Liver Enzymes: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
