Monday Poster Session
Category: Liver
P3625 - Statin Use After Liver Transplantation Is Associated With Decreased Liver Rejection and Mortality
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hussein Baydoun, MD (he/him/his)
Indiana University
Indianapolis, IN
Presenting Author(s)
Award: ACG Presidential Poster Award
Hussein Baydoun, MD1, Andrej Sikoski, MD1, Ahdy Helmy, MBBS1, John Guardiola, MD2, Indira Bhavsar-Burke, MD3, John Holden, MD1
1Indiana University, Indianapolis, IN; 2Indiana University School of Medicine, Indianapolis, IN; 3University of Texas Southwestern School of Medicine, Dallas, TX
Introduction: Liver transplantation is a life-saving procedure for patients with end-stage liver disease, but long-term success remains limited by graft failure, acute rejection, and immunologic complications. Statins, beyond their lipid-lowering effects, possess immunomodulatory and anti-inflammatory properties that may influence transplant-related outcomes. However, their safety and efficacy in liver transplant recipients remain underexplored.
Methods: We obtained and analyzed retrospective data from the U.S. Collaborative Network on the TriNetX platform and identified patients who underwent liver transplantation. Patients were divided into two cohorts: those who initiated statin therapy within 1 year post-transplant (Statin group) and those who did not receive statins within 12 months (Control group). Propensity score matching was performed (1:1) on demographics, comorbidities, MELD-score and immunosuppressive medicaitons. The primary outcomes were liver transplant rejection and liver transplant failure. Secondary outcomes were major adverse cardiovascular events including myocardial infarction (MI) and stroke, biliary stricture, hepatic artery thrombosis, all-cause mortality, liver transplant infection, hepatotoxicity, rhabdomyolysis and myopathy. The risk of each outcome was calculated and expressed as an odds ratio (OR) with a 95% confidence interval (CI). Two-sided p-value < 0.05 was considered statistically significant.
Results: After PSM, 1,786 patients using statins were matched to 1,786 non-users (Table 1). Statin use was associated with a significantly decreased odds of liver rejection (OR 0.55, 95% CI 0.46-0.66, p< 0.0001), liver failure (OR 0.36, 95% CI 0.28-0.46, p< 0.0001), bile duct stricture (OR 0.69, 95% Cl 0.57-0.83, p< 0.0001), all-cause mortality (OR 0.69, 95% CI 0.53-0.90, p= 0.007), liver transplant infection (OR 0.67, 95% Cl 0.50-0.89, p= 0.006) and hepatotoxicity (OR 0.51, 95% Cl 0.39-0.9, p=0.019) (Figure 1). Other outcomes including MI, stroke, hepatic artery thrombosis, rhabdomyolysis and myopathy were statistically similar between the two cohorts.
Discussion: Statin use after liver transplantation is associated with improved liver transplantation outcomes including liver rejection, liver failure, liver infection, bile duct stricture and all-cause mortality, without evidence of increased hepatoxtocity or statin-induced rhabdomyolysis or myopathy. These findings support consideration of statins in post-liver transplant settings.
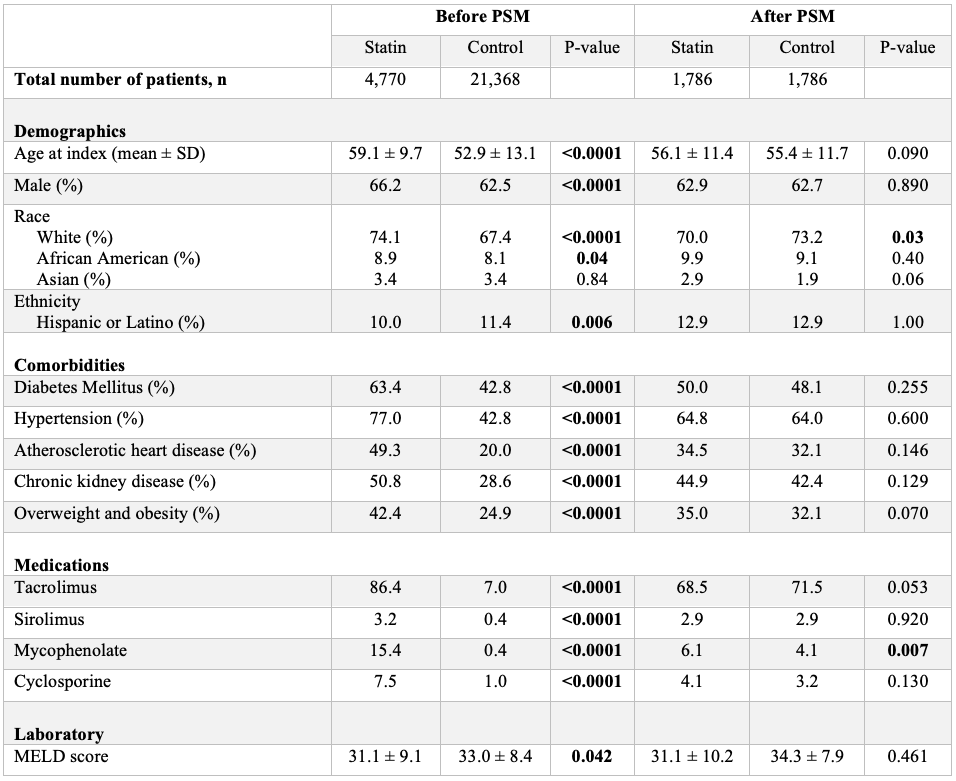
Figure: Table 1: Baseline patient characteristics before and after propensity-score matching (PSM).
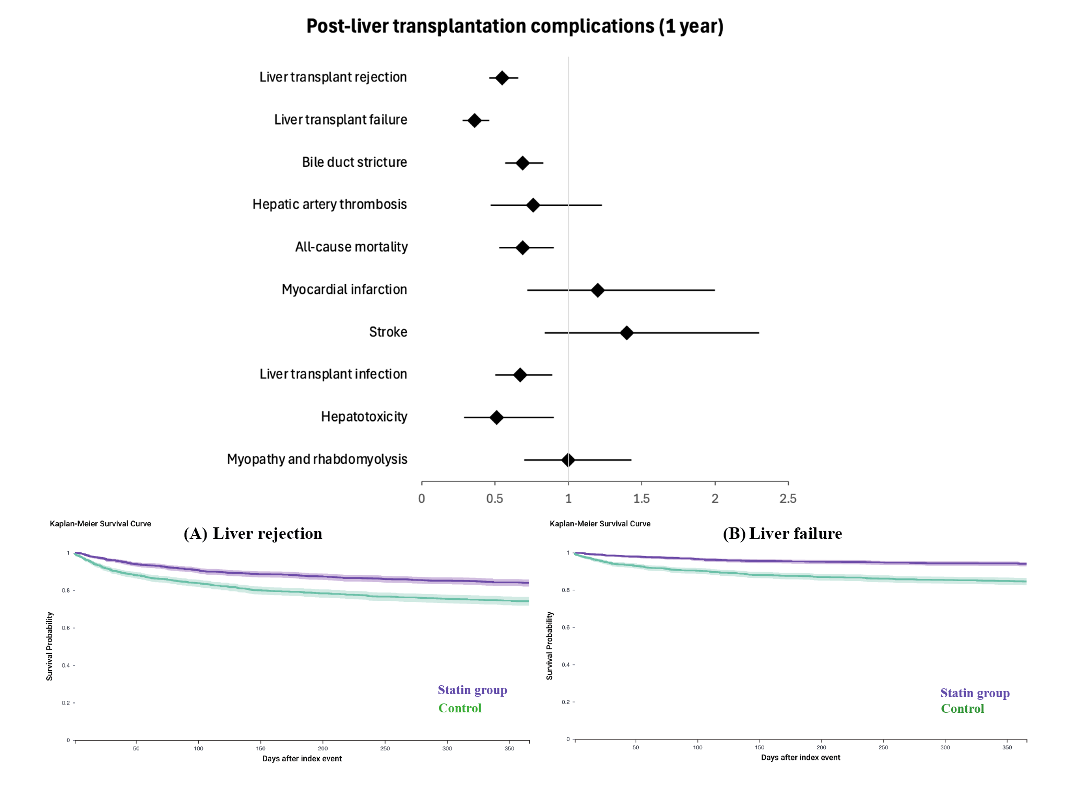
Figure: Figure 1: Post-liver transplantation complications after 1 year and Kaplan-Meier survival curves of our primary outcomes
Disclosures:
Hussein Baydoun indicated no relevant financial relationships.
Andrej Sikoski indicated no relevant financial relationships.
Ahdy Helmy indicated no relevant financial relationships.
John Guardiola indicated no relevant financial relationships.
Indira Bhavsar-Burke indicated no relevant financial relationships.
John Holden indicated no relevant financial relationships.
Hussein Baydoun, MD1, Andrej Sikoski, MD1, Ahdy Helmy, MBBS1, John Guardiola, MD2, Indira Bhavsar-Burke, MD3, John Holden, MD1. P3625 - Statin Use After Liver Transplantation Is Associated With Decreased Liver Rejection and Mortality, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Hussein Baydoun, MD1, Andrej Sikoski, MD1, Ahdy Helmy, MBBS1, John Guardiola, MD2, Indira Bhavsar-Burke, MD3, John Holden, MD1
1Indiana University, Indianapolis, IN; 2Indiana University School of Medicine, Indianapolis, IN; 3University of Texas Southwestern School of Medicine, Dallas, TX
Introduction: Liver transplantation is a life-saving procedure for patients with end-stage liver disease, but long-term success remains limited by graft failure, acute rejection, and immunologic complications. Statins, beyond their lipid-lowering effects, possess immunomodulatory and anti-inflammatory properties that may influence transplant-related outcomes. However, their safety and efficacy in liver transplant recipients remain underexplored.
Methods: We obtained and analyzed retrospective data from the U.S. Collaborative Network on the TriNetX platform and identified patients who underwent liver transplantation. Patients were divided into two cohorts: those who initiated statin therapy within 1 year post-transplant (Statin group) and those who did not receive statins within 12 months (Control group). Propensity score matching was performed (1:1) on demographics, comorbidities, MELD-score and immunosuppressive medicaitons. The primary outcomes were liver transplant rejection and liver transplant failure. Secondary outcomes were major adverse cardiovascular events including myocardial infarction (MI) and stroke, biliary stricture, hepatic artery thrombosis, all-cause mortality, liver transplant infection, hepatotoxicity, rhabdomyolysis and myopathy. The risk of each outcome was calculated and expressed as an odds ratio (OR) with a 95% confidence interval (CI). Two-sided p-value < 0.05 was considered statistically significant.
Results: After PSM, 1,786 patients using statins were matched to 1,786 non-users (Table 1). Statin use was associated with a significantly decreased odds of liver rejection (OR 0.55, 95% CI 0.46-0.66, p< 0.0001), liver failure (OR 0.36, 95% CI 0.28-0.46, p< 0.0001), bile duct stricture (OR 0.69, 95% Cl 0.57-0.83, p< 0.0001), all-cause mortality (OR 0.69, 95% CI 0.53-0.90, p= 0.007), liver transplant infection (OR 0.67, 95% Cl 0.50-0.89, p= 0.006) and hepatotoxicity (OR 0.51, 95% Cl 0.39-0.9, p=0.019) (Figure 1). Other outcomes including MI, stroke, hepatic artery thrombosis, rhabdomyolysis and myopathy were statistically similar between the two cohorts.
Discussion: Statin use after liver transplantation is associated with improved liver transplantation outcomes including liver rejection, liver failure, liver infection, bile duct stricture and all-cause mortality, without evidence of increased hepatoxtocity or statin-induced rhabdomyolysis or myopathy. These findings support consideration of statins in post-liver transplant settings.
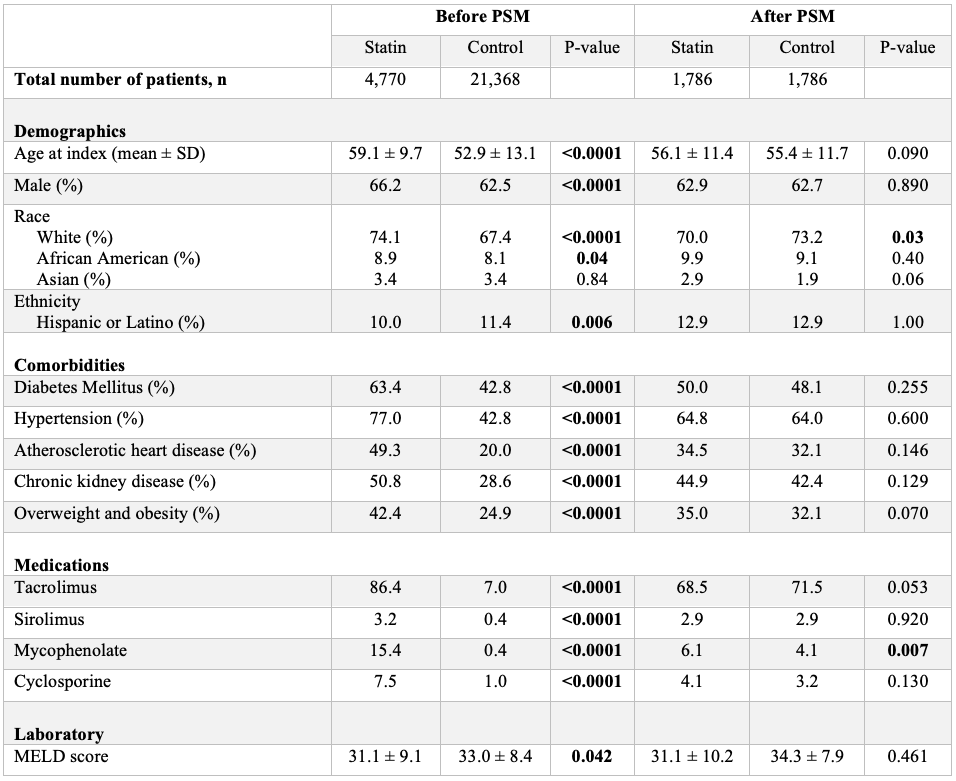
Figure: Table 1: Baseline patient characteristics before and after propensity-score matching (PSM).
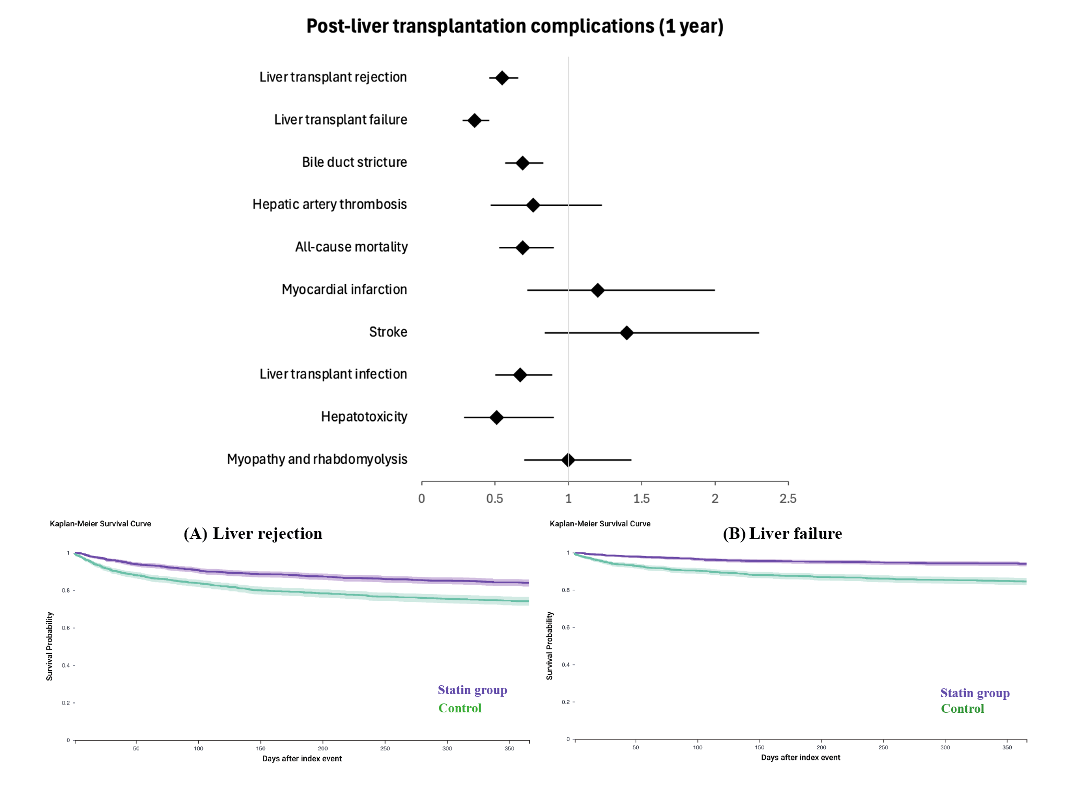
Figure: Figure 1: Post-liver transplantation complications after 1 year and Kaplan-Meier survival curves of our primary outcomes
Disclosures:
Hussein Baydoun indicated no relevant financial relationships.
Andrej Sikoski indicated no relevant financial relationships.
Ahdy Helmy indicated no relevant financial relationships.
John Guardiola indicated no relevant financial relationships.
Indira Bhavsar-Burke indicated no relevant financial relationships.
John Holden indicated no relevant financial relationships.
Hussein Baydoun, MD1, Andrej Sikoski, MD1, Ahdy Helmy, MBBS1, John Guardiola, MD2, Indira Bhavsar-Burke, MD3, John Holden, MD1. P3625 - Statin Use After Liver Transplantation Is Associated With Decreased Liver Rejection and Mortality, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


