Monday Poster Session
Category: Interventional Endoscopy
P3619 - Salvage of Choledochoduodenostomy Attempt via Novel Stent-In-Stent Endoscopic Approach: A Case Report
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anil Bhatnagar, MD
Penn State Health Milton S. Hershey Medical Center
Hershey, PA
Presenting Author(s)
Award: ACG Presidential Poster Award
Anil Bhatnagar, MD, Justin Canakis, DO, Hadie Razjouyan, MD
Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is standard for biliary drainage in malignant obstruction but fails in up to 8% of cases. Endoscopic ultrasound guided biliary drainage (EUS-BD) is second line, with endoscopic ultrasound guided choledochoduodenostomy (EUS-CDS) favored for distal obstruction. EUS-CDS carries technical risk; when stent maldeployment occurs, prompt salvage with covered or lumen apposing metal stents (LAMS) improves outcomes. Alternatives include percutaneous biliary drainage (PTBD), EUS-guided hepaticogastrostomy (EUS-HGS), or surgery. We describe a failed EUS-CDS salvaged via a novel stent-in-stent ERCP approach, offering less invasive rescue.
Case Description/
Methods: An 88-year-old man was transferred to our tertiary care center for two weeks of obstructive jaundice. CT showed a 3.5cm pancreatic head mass and ductal dilation.
With ERCP, multiple cannulation attempts only accessed the ventral pancreatic duct with 0.025in wire. Despite pancreatic access, precut sphincterotomy, and additional advanced endoscopic consultation, standard ERCP failed at biliary access due to the obstructing mass. EUS showed a 3.4cm mass with 18mm common bile duct (CBD) dilation. Rapid onsite evaluation confirmed pancreatic adenocarcinoma. EUS-CDS was attempted and 10mm LAMS was placed transduodenally into CBD; bile drained through. Follow-up CT showed biliary decompression but concern for LAMS malposition with one end not in CBD.
Repeat ERCP showed LAMS protruding into duodenum. A 0.025in wire was placed through LAMS but coiled in the closed space. Contrast evaluation showed the stent deployed into the retroperitoneum, confirmed with ultra-slim gastroscope through LAMS showing puncture side of CBD draining into retroperitoneum. With direct view and fluoroscopy, a guide wire was placed into proximal bile duct. A 1T channel scope was exchanged over wire and 10Fr x 4cm double pigtail plastic biliary stent was placed through LAMS into CBD yielding bile flow. Liver enzymes normalized.
Discussion: While LAMS improved success of EUS-BD, failure rates up to 8% underscore need for alternatives. EUS-HGS and PTBD are effective but carry higher risks and may not be available.
Our stent-in-stent approach allows successful cannulation of the biliary system via the maldeployed LAMS, enabling decompression without more invasive intervention. This novel endoscopic rescue technique after LAMS maldeployment during EUS-CDS may be a valuable salvage option in centers with advanced endoscopic expertise.
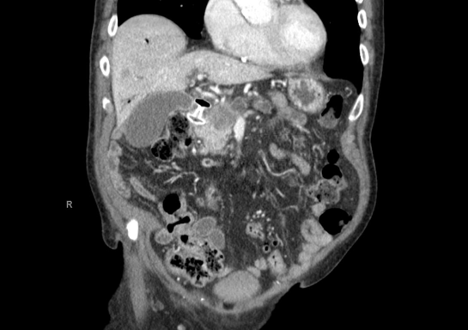
Figure: Figure 1. CT Abdomen (Coronal View) demonstrating one end of LAMS in duodenum the other end not clearly visualized in CBD.

Figure: Figure 2. Fluoroscopy demonstrating biliary leak after LAMS maldeployment (left), access with deep biliary cannulation (center), and double pigtail plastic stent placement through LAMS (right).
Disclosures:
Anil Bhatnagar indicated no relevant financial relationships.
Justin Canakis indicated no relevant financial relationships.
Hadie Razjouyan indicated no relevant financial relationships.
Anil Bhatnagar, MD, Justin Canakis, DO, Hadie Razjouyan, MD. P3619 - Salvage of Choledochoduodenostomy Attempt via Novel Stent-In-Stent Endoscopic Approach: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Anil Bhatnagar, MD, Justin Canakis, DO, Hadie Razjouyan, MD
Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is standard for biliary drainage in malignant obstruction but fails in up to 8% of cases. Endoscopic ultrasound guided biliary drainage (EUS-BD) is second line, with endoscopic ultrasound guided choledochoduodenostomy (EUS-CDS) favored for distal obstruction. EUS-CDS carries technical risk; when stent maldeployment occurs, prompt salvage with covered or lumen apposing metal stents (LAMS) improves outcomes. Alternatives include percutaneous biliary drainage (PTBD), EUS-guided hepaticogastrostomy (EUS-HGS), or surgery. We describe a failed EUS-CDS salvaged via a novel stent-in-stent ERCP approach, offering less invasive rescue.
Case Description/
Methods: An 88-year-old man was transferred to our tertiary care center for two weeks of obstructive jaundice. CT showed a 3.5cm pancreatic head mass and ductal dilation.
With ERCP, multiple cannulation attempts only accessed the ventral pancreatic duct with 0.025in wire. Despite pancreatic access, precut sphincterotomy, and additional advanced endoscopic consultation, standard ERCP failed at biliary access due to the obstructing mass. EUS showed a 3.4cm mass with 18mm common bile duct (CBD) dilation. Rapid onsite evaluation confirmed pancreatic adenocarcinoma. EUS-CDS was attempted and 10mm LAMS was placed transduodenally into CBD; bile drained through. Follow-up CT showed biliary decompression but concern for LAMS malposition with one end not in CBD.
Repeat ERCP showed LAMS protruding into duodenum. A 0.025in wire was placed through LAMS but coiled in the closed space. Contrast evaluation showed the stent deployed into the retroperitoneum, confirmed with ultra-slim gastroscope through LAMS showing puncture side of CBD draining into retroperitoneum. With direct view and fluoroscopy, a guide wire was placed into proximal bile duct. A 1T channel scope was exchanged over wire and 10Fr x 4cm double pigtail plastic biliary stent was placed through LAMS into CBD yielding bile flow. Liver enzymes normalized.
Discussion: While LAMS improved success of EUS-BD, failure rates up to 8% underscore need for alternatives. EUS-HGS and PTBD are effective but carry higher risks and may not be available.
Our stent-in-stent approach allows successful cannulation of the biliary system via the maldeployed LAMS, enabling decompression without more invasive intervention. This novel endoscopic rescue technique after LAMS maldeployment during EUS-CDS may be a valuable salvage option in centers with advanced endoscopic expertise.
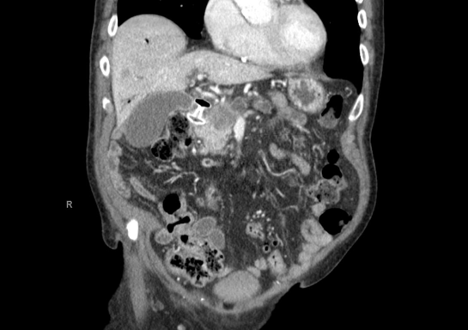
Figure: Figure 1. CT Abdomen (Coronal View) demonstrating one end of LAMS in duodenum the other end not clearly visualized in CBD.

Figure: Figure 2. Fluoroscopy demonstrating biliary leak after LAMS maldeployment (left), access with deep biliary cannulation (center), and double pigtail plastic stent placement through LAMS (right).
Disclosures:
Anil Bhatnagar indicated no relevant financial relationships.
Justin Canakis indicated no relevant financial relationships.
Hadie Razjouyan indicated no relevant financial relationships.
Anil Bhatnagar, MD, Justin Canakis, DO, Hadie Razjouyan, MD. P3619 - Salvage of Choledochoduodenostomy Attempt via Novel Stent-In-Stent Endoscopic Approach: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

