Monday Poster Session
Category: Interventional Endoscopy
P3618 - Hidden Hemorrhage: A Case of a Symptomatic Pancreatic Pseudoaneurysm Discovered by Endoscopic Ultrasound
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Anvit Reddy, DO (he/him/his)
University of Florida College of Medicine - 655 W 8th St Jacksonville, FL 32221UNITED STATES - Jacksonville, FL
Jacksonville, FL
Presenting Author(s)
Anvit Reddy, DO1, Radhika Sharma, DO2, Nirmal Onteddu, MD2, Bruno Ribeiro, MD2
1University of Florida College of Medicine - 655 W 8th St Jacksonville, FL 32221UNITED STATES - Jacksonville, FL, Jacksonville, FL; 2University of Florida College of Medicine, Jacksonville, FL
Introduction: Pancreatic pseudocysts are common complications of pancreatitis that are managed conservatively if asymptomatic, or with endoscopic drainage if symptomatic. Rarely, pseudoaneurysms form in patients with pseudocysts. They cannot be drained endoscopically, especially if there is intracystic hemorrhage, as this can be lethal. Diagnosis via angiography is the gold standard, however, EUS with Doppler is appropriate, especially in large extravasations.
Case Description/
Methods: A 55-year-old male with a past medical history of polysubstance abuse disorder initially presented to the hospital with abdominal pain and tenderness, where a computed tomography of the abdomen and pelvis (CTAP) revealed an 8.5 x 10 x 9.6 cm pancreatic pseudocyst with different fluid densities concerning for hemorrhage. Interventional radiology (IR) performed an angiogram that showed no evidence of active extravasation, and he was discharged home after symptom relief.
Two weeks later, he returned to the hospital with the same chief complaints. Laboratory evaluation included a white blood cell count of 11.01 THOU/CUMM, hemoglobin 8.9 G/DL (baseline 10-11 G/DL), and lipase of 131 U/L. CTAP showed an 18.9 cm multilobulated cystic-appearing fluid collection around the pancreatic head and neck (Figure 1A, 1B). Based on previous IR images showing no active extravasation, gastroenterology (GI) was consulted for endoscopic ultrasound (EUS) and fine needle aspiration. GI performed an EUS with the intent of drainage; however, the procedure was aborted after Doppler revealed a fluid-filled cavity with clear communication between the splenic vessels, consistent with intracystic hemorrhage (Figure 2). IR performed an angiogram, which showed an irregularity of the gastroduodenal artery with no active extravasation. Based on EUS findings, the gastroduodenal and proximal splenic arteries were embolized with coils across the pancreaticoduodenal and duodenal bulb branches. He was managed supportively and was discharged in a stable condition.
Discussion: It is important to consider intracystic hemorrhage when a patient with a known pseudocyst presents to the hospital with abdominal pain and acute anemia. Although angiography is sensitive for the diagnosis and management of hemorrhagic pancreatic pseudoaneurysm, EUS with Doppler should be performed before any pancreatic pseudocyst drainage is attempted. In cases where bleeding is suspected, it is imperative to confirm the absence of extravasation with EUS to avoid fatal complications.
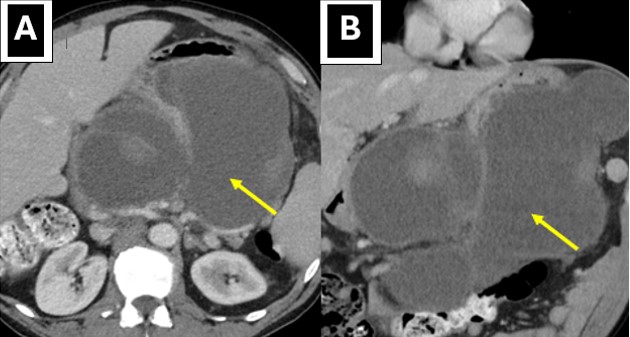
Figure: Figure 1A: Computed tomography of the abdomen showing pancreatic pseudocyst in axial view
Figure 1B: Computed tomography of the abdomen showing pancreatic pseudocyst in coronal view
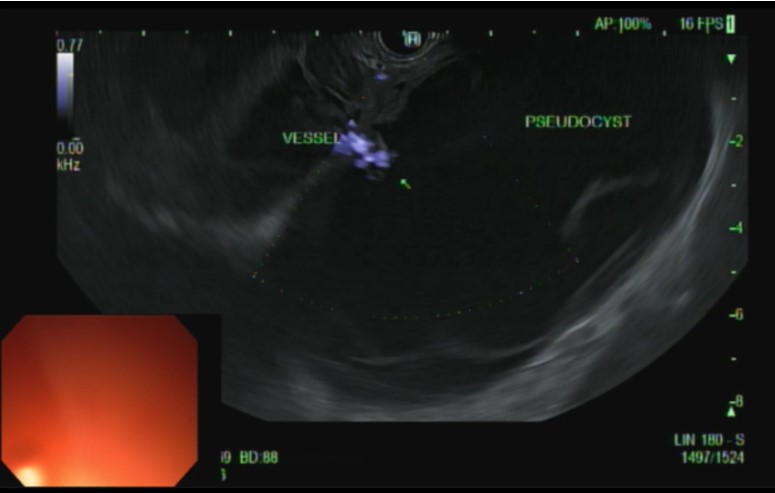
Figure: Figure 2: Endoscopic ultrasound with doppler demonstrating communication between splenic vessel and pseudocyst
Disclosures:
Anvit Reddy indicated no relevant financial relationships.
Radhika Sharma indicated no relevant financial relationships.
Nirmal Onteddu indicated no relevant financial relationships.
Bruno Ribeiro indicated no relevant financial relationships.
Anvit Reddy, DO1, Radhika Sharma, DO2, Nirmal Onteddu, MD2, Bruno Ribeiro, MD2. P3618 - Hidden Hemorrhage: A Case of a Symptomatic Pancreatic Pseudoaneurysm Discovered by Endoscopic Ultrasound, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Florida College of Medicine - 655 W 8th St Jacksonville, FL 32221UNITED STATES - Jacksonville, FL, Jacksonville, FL; 2University of Florida College of Medicine, Jacksonville, FL
Introduction: Pancreatic pseudocysts are common complications of pancreatitis that are managed conservatively if asymptomatic, or with endoscopic drainage if symptomatic. Rarely, pseudoaneurysms form in patients with pseudocysts. They cannot be drained endoscopically, especially if there is intracystic hemorrhage, as this can be lethal. Diagnosis via angiography is the gold standard, however, EUS with Doppler is appropriate, especially in large extravasations.
Case Description/
Methods: A 55-year-old male with a past medical history of polysubstance abuse disorder initially presented to the hospital with abdominal pain and tenderness, where a computed tomography of the abdomen and pelvis (CTAP) revealed an 8.5 x 10 x 9.6 cm pancreatic pseudocyst with different fluid densities concerning for hemorrhage. Interventional radiology (IR) performed an angiogram that showed no evidence of active extravasation, and he was discharged home after symptom relief.
Two weeks later, he returned to the hospital with the same chief complaints. Laboratory evaluation included a white blood cell count of 11.01 THOU/CUMM, hemoglobin 8.9 G/DL (baseline 10-11 G/DL), and lipase of 131 U/L. CTAP showed an 18.9 cm multilobulated cystic-appearing fluid collection around the pancreatic head and neck (Figure 1A, 1B). Based on previous IR images showing no active extravasation, gastroenterology (GI) was consulted for endoscopic ultrasound (EUS) and fine needle aspiration. GI performed an EUS with the intent of drainage; however, the procedure was aborted after Doppler revealed a fluid-filled cavity with clear communication between the splenic vessels, consistent with intracystic hemorrhage (Figure 2). IR performed an angiogram, which showed an irregularity of the gastroduodenal artery with no active extravasation. Based on EUS findings, the gastroduodenal and proximal splenic arteries were embolized with coils across the pancreaticoduodenal and duodenal bulb branches. He was managed supportively and was discharged in a stable condition.
Discussion: It is important to consider intracystic hemorrhage when a patient with a known pseudocyst presents to the hospital with abdominal pain and acute anemia. Although angiography is sensitive for the diagnosis and management of hemorrhagic pancreatic pseudoaneurysm, EUS with Doppler should be performed before any pancreatic pseudocyst drainage is attempted. In cases where bleeding is suspected, it is imperative to confirm the absence of extravasation with EUS to avoid fatal complications.
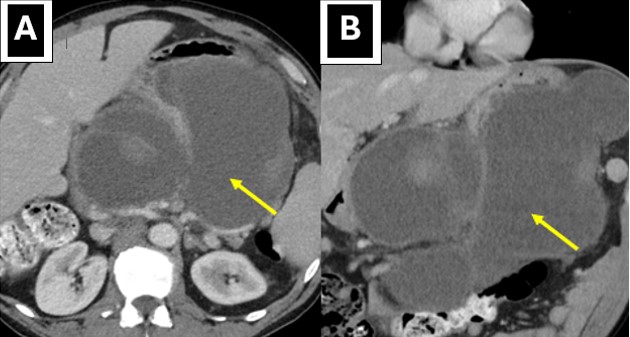
Figure: Figure 1A: Computed tomography of the abdomen showing pancreatic pseudocyst in axial view
Figure 1B: Computed tomography of the abdomen showing pancreatic pseudocyst in coronal view
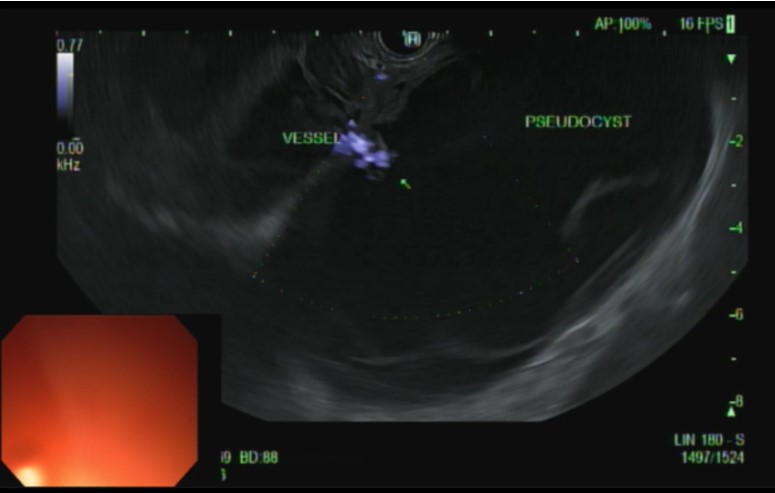
Figure: Figure 2: Endoscopic ultrasound with doppler demonstrating communication between splenic vessel and pseudocyst
Disclosures:
Anvit Reddy indicated no relevant financial relationships.
Radhika Sharma indicated no relevant financial relationships.
Nirmal Onteddu indicated no relevant financial relationships.
Bruno Ribeiro indicated no relevant financial relationships.
Anvit Reddy, DO1, Radhika Sharma, DO2, Nirmal Onteddu, MD2, Bruno Ribeiro, MD2. P3618 - Hidden Hemorrhage: A Case of a Symptomatic Pancreatic Pseudoaneurysm Discovered by Endoscopic Ultrasound, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
