Monday Poster Session
Category: Interventional Endoscopy
P3612 - The Outcomes of EUS-Guided Gastrojejunostomy in Patients With Gastric Outlet Obstruction
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Gopala Konduri, MD (he/him/his)
University of Missouri
Columbia, MO
Presenting Author(s)
Muhammad Nadeem Yousaf, MD1, Gopala Konduri, MD1, Ibukunoluwa Oshobu, MD, MPH2, Darian Fard, MD2, Ghassan Hammoud, MD2
1University of Missouri, Columbia, MO; 2University of Missouri Health Care, Columbia, MO
Introduction: Endoscopic ultrasound-guided gastrojejunostomy (EUS-GJ) is an emerging, minimally invasive technique for managing patients with gastric outlet obstruction (GOO). The clinical syndrome of GOO results from luminal obstruction with either benign or malignant etiologies. We aimed to evaluate the technical success, clinical success, and safety of EUS-GJ in patients with benign and malignant GOO.
Case Description/
Methods: This retrospective case series included all patients who underwent EUS-GJ between May 2022 and May 2025 at a single tertiary care center. Patients included had benign or malignant GOO. Primary outcomes were technical success and clinical success rate. Secondary outcomes were adverse events and the need for re-interventions. Technical success was defined as adequate positioning and deployment of the stent as seen on endoscopy and radiology imaging, while clinical success was defined as improvement in GOO Scoring System (GOOSS) grade.
Results: A total of 4 patients with GOO underwent EUS-GJ with a mean age of 65 ± 8.0 years (range 58-74 years), and 75% were female. The etiologies of GOO were benign strictures in 75% and malignant duodenal obstruction in 25% of patients. EUS-GJ was performed using the direct method technique with a 20mm x 10mm lumen-apposing metal stent (LAMS) in all patients. Both technical success and clinical success rate were 100% in all patients. The mean procedure time was 53.5 ± 11.5 min (range 38-64 min) and median length of hospital stay was 2.5 days (range 1-10 days). There were no immediate significant AEs encountered, nor was there a need for re-interventions in any patient following EUS-GJ. Prior to EUS-GJ, all patients were on total parenteral nutrition as they were unable to tolerate per-oral feeding. A significant improvement in patient’s symptoms and mean GOOSS grade from 0 to 2.7 was observed after EUS-GJ at short-term follow up. There were no recurrent symptoms on mean follow up of 5.5 ± 3.3 months. One patient experienced recurrent symptoms of GOO due to closure of GJ fistula 6 months after removal of LAMS.
Discussion: EUS-GJ demonstrates promising safety and feasibility for patients with benign and malignant GOO. Prospective clinical trials are needed to determine predictors of recurrent symptoms and long-term clinical outcomes of EUS-GJ.
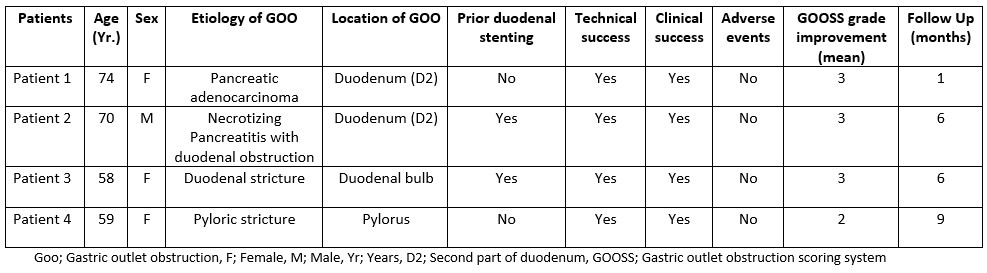
Figure: Patient’s characteristics and procedure outcomes
Disclosures:
Muhammad Nadeem Yousaf indicated no relevant financial relationships.
Gopala Konduri indicated no relevant financial relationships.
Ibukunoluwa Oshobu indicated no relevant financial relationships.
Darian Fard indicated no relevant financial relationships.
Ghassan Hammoud indicated no relevant financial relationships.
Muhammad Nadeem Yousaf, MD1, Gopala Konduri, MD1, Ibukunoluwa Oshobu, MD, MPH2, Darian Fard, MD2, Ghassan Hammoud, MD2. P3612 - The Outcomes of EUS-Guided Gastrojejunostomy in Patients With Gastric Outlet Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Missouri, Columbia, MO; 2University of Missouri Health Care, Columbia, MO
Introduction: Endoscopic ultrasound-guided gastrojejunostomy (EUS-GJ) is an emerging, minimally invasive technique for managing patients with gastric outlet obstruction (GOO). The clinical syndrome of GOO results from luminal obstruction with either benign or malignant etiologies. We aimed to evaluate the technical success, clinical success, and safety of EUS-GJ in patients with benign and malignant GOO.
Case Description/
Methods: This retrospective case series included all patients who underwent EUS-GJ between May 2022 and May 2025 at a single tertiary care center. Patients included had benign or malignant GOO. Primary outcomes were technical success and clinical success rate. Secondary outcomes were adverse events and the need for re-interventions. Technical success was defined as adequate positioning and deployment of the stent as seen on endoscopy and radiology imaging, while clinical success was defined as improvement in GOO Scoring System (GOOSS) grade.
Results: A total of 4 patients with GOO underwent EUS-GJ with a mean age of 65 ± 8.0 years (range 58-74 years), and 75% were female. The etiologies of GOO were benign strictures in 75% and malignant duodenal obstruction in 25% of patients. EUS-GJ was performed using the direct method technique with a 20mm x 10mm lumen-apposing metal stent (LAMS) in all patients. Both technical success and clinical success rate were 100% in all patients. The mean procedure time was 53.5 ± 11.5 min (range 38-64 min) and median length of hospital stay was 2.5 days (range 1-10 days). There were no immediate significant AEs encountered, nor was there a need for re-interventions in any patient following EUS-GJ. Prior to EUS-GJ, all patients were on total parenteral nutrition as they were unable to tolerate per-oral feeding. A significant improvement in patient’s symptoms and mean GOOSS grade from 0 to 2.7 was observed after EUS-GJ at short-term follow up. There were no recurrent symptoms on mean follow up of 5.5 ± 3.3 months. One patient experienced recurrent symptoms of GOO due to closure of GJ fistula 6 months after removal of LAMS.
Discussion: EUS-GJ demonstrates promising safety and feasibility for patients with benign and malignant GOO. Prospective clinical trials are needed to determine predictors of recurrent symptoms and long-term clinical outcomes of EUS-GJ.
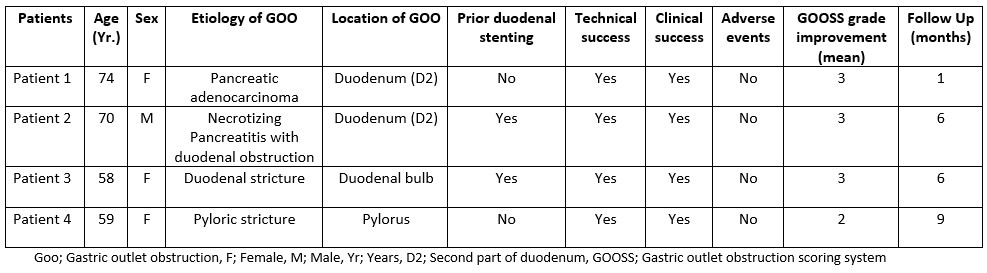
Figure: Patient’s characteristics and procedure outcomes
Disclosures:
Muhammad Nadeem Yousaf indicated no relevant financial relationships.
Gopala Konduri indicated no relevant financial relationships.
Ibukunoluwa Oshobu indicated no relevant financial relationships.
Darian Fard indicated no relevant financial relationships.
Ghassan Hammoud indicated no relevant financial relationships.
Muhammad Nadeem Yousaf, MD1, Gopala Konduri, MD1, Ibukunoluwa Oshobu, MD, MPH2, Darian Fard, MD2, Ghassan Hammoud, MD2. P3612 - The Outcomes of EUS-Guided Gastrojejunostomy in Patients With Gastric Outlet Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
