Monday Poster Session
Category: Interventional Endoscopy
P3611 - ERCP in Billroth II Anatomy: Navigating the Challenges of Surgically Altered Gastrointestinal Anatomy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Pearl Aggarwal, MD (she/her/hers)
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Pearl Aggarwal, MD1, Michael Liu, MD2, Fatema Dinary, 3, Sara Saleh, MD4, Ibrahim Maghari, MD5, Fazel Dinary, MD6
1Cleveland Clinic, Rocky River, OH; 2University Hospitals Cleveland Medical Center, Case Western Reserve University, Westlake, OH; 3Case Western Reserve University, Westlake, OH; 4Hashemite University, Zarqa, Az Zarqa', Jordan; 5Parkview Medical Center, Fort Wayne, IN; 6University Hospital, Cleveland, OH
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) remains a cornerstone in managing biliary disorders. However, surgically altered gastrointestinal anatomy introduces significant technical challenges. Early recognition of anatomic variations is critical for procedural planning. We present a case of a rare Billroth II variant performed in the 1960s, which generated substantial clinical interest.
Case Description/
Methods: A 63-year-old male presented with persistent nausea and vomiting. His medical history included a partial gastrectomy with Billroth II reconstruction in the neonatal period for gastric atresia. Laboratory evaluation revealed leukocytosis (15,000/µL) and a cholestatic liver profile: alkaline phosphatase 140 U/L, AST 241 U/L, ALT 275 U/L, total bilirubin 5.5 mg/dL, and direct bilirubin 2.1 mg/dL. Magnetic resonance cholangiopancreatography (MRCP) demonstrated intrahepatic biliary dilation and a filling defect in the distal common bile duct (CBD) (Image 1). Initial ERCP using a single-balloon enteroscope (SBE) with a distal cap was unsuccessful due to the inability to locate the major papilla. With worsening cholestasis (total bilirubin 9.4 mg/dL, direct bilirubin 6.0 mg/dL), a repeat ERCP was performed using a fluoroscopy-guided rendezvous approach in collaboration with interventional radiology. Endoscopy confirmed a Billroth II anatomy with an elongated afferent limb measuring 160 cm from the incisors. Using SBE with a distal cap, the papilla was accessed and cannulated. Cholangiography revealed an obstructing stone. A sphincterotomy was performed, followed by placement of a fully covered self-expanding metal stent (SEMS). A tattoo was placed near the biliary limb to aid future access (Image 2). At follow-up ERCP, the biliary limb was readily identified via the tattoo. The SEMS remained widely patent. Cannulation through the stent allowed balloon extraction of copious sludge and an 8 mm stone. The stent was then removed. The patient remained asymptomatic with no recurrence at one-month follow-up.
Discussion: This case illustrates the diagnostic and therapeutic complexities of ERCP in patients with surgically altered anatomy. A detailed pre-procedural review of history and imaging is vital to recognizing anatomical variants and guiding endoscopic strategy. Tailored approaches and multidisciplinary collaboration are essential for optimizing outcomes in this technically challenging population.
References: Li JS et al. Saudi J Gastroenterol. 2019. Pribadi RR et al. J Dig Dis. 2019.
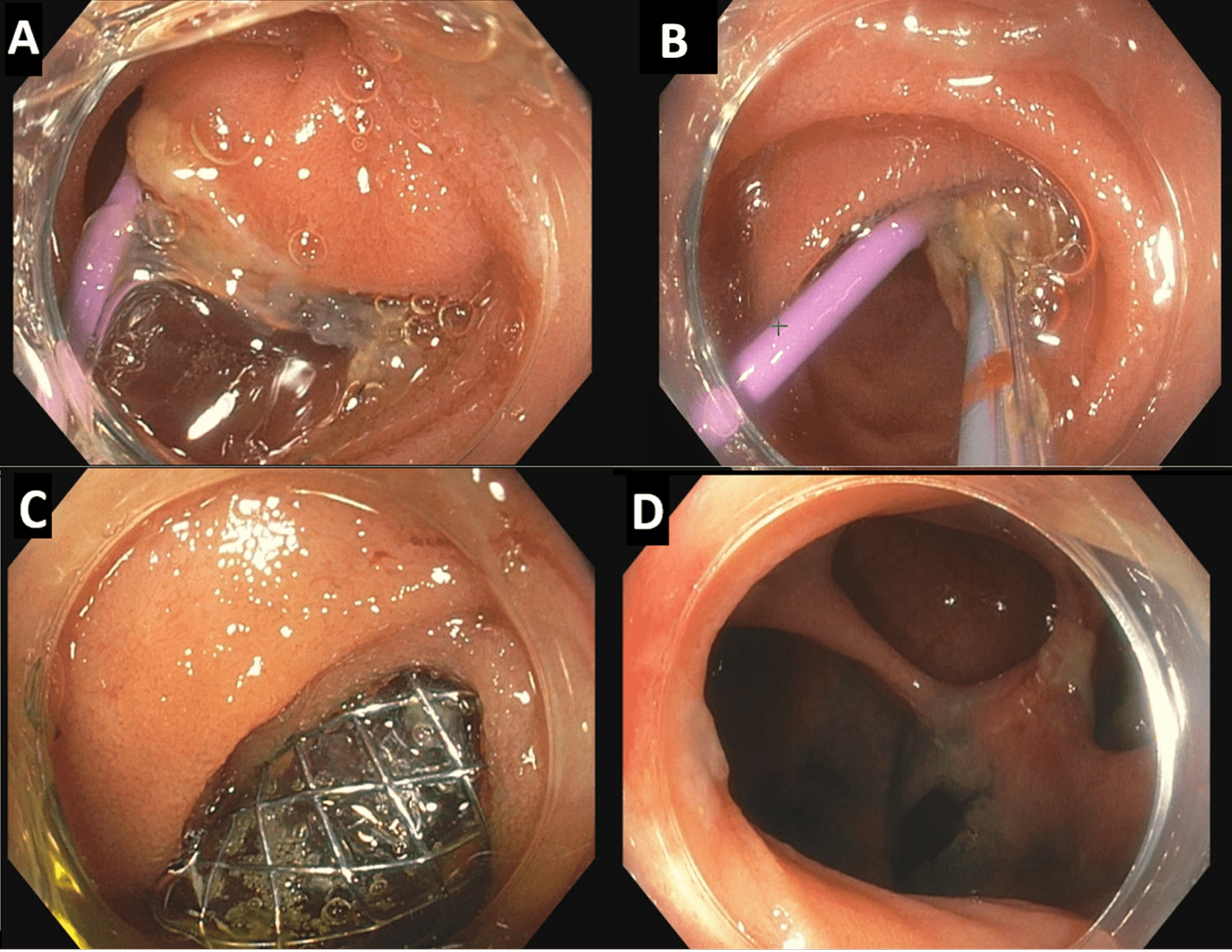
Figure: Image 1: A) Magnetic resonance imaging showing biliary duct dilation . B) Magnetic resonance cholangiopancreatography (MRCP) showing common bile duct filling defects
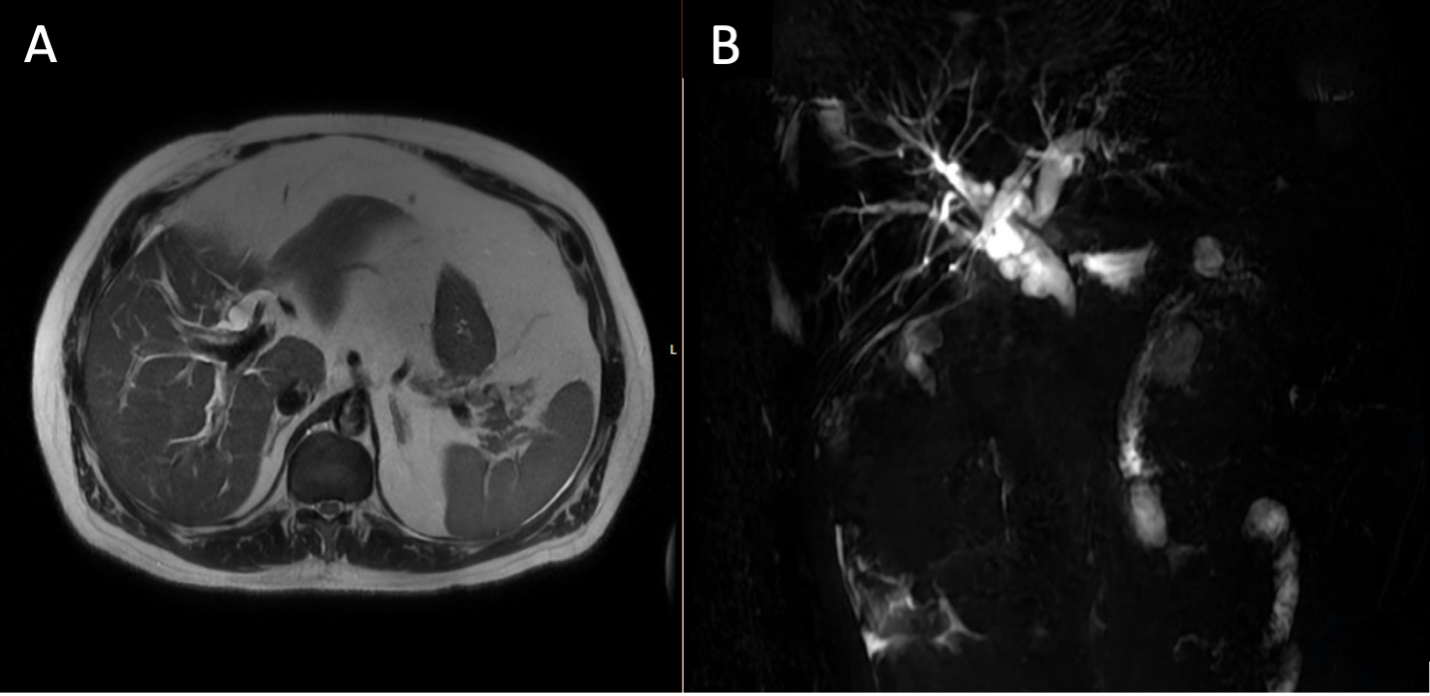
Figure: Image 2: Endoscopic retrograde cholangiopancreatography (ERCP) A) Major ampulla at the blind end of the biliary limb with Interventional Radiology rendezvous catheter (~ 160 cm from the incisors). B) Biliary Cannulation achieved via retrograde approach using sphincterotome. C) Placement of fully covered metal stent. D) The proximal part of the biliary limb tattooed for repeated ERCP
Disclosures:
Pearl Aggarwal indicated no relevant financial relationships.
Michael Liu indicated no relevant financial relationships.
Fatema Dinary indicated no relevant financial relationships.
Sara Saleh indicated no relevant financial relationships.
Ibrahim Maghari indicated no relevant financial relationships.
Fazel Dinary indicated no relevant financial relationships.
Pearl Aggarwal, MD1, Michael Liu, MD2, Fatema Dinary, 3, Sara Saleh, MD4, Ibrahim Maghari, MD5, Fazel Dinary, MD6. P3611 - ERCP in Billroth II Anatomy: Navigating the Challenges of Surgically Altered Gastrointestinal Anatomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic, Rocky River, OH; 2University Hospitals Cleveland Medical Center, Case Western Reserve University, Westlake, OH; 3Case Western Reserve University, Westlake, OH; 4Hashemite University, Zarqa, Az Zarqa', Jordan; 5Parkview Medical Center, Fort Wayne, IN; 6University Hospital, Cleveland, OH
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) remains a cornerstone in managing biliary disorders. However, surgically altered gastrointestinal anatomy introduces significant technical challenges. Early recognition of anatomic variations is critical for procedural planning. We present a case of a rare Billroth II variant performed in the 1960s, which generated substantial clinical interest.
Case Description/
Methods: A 63-year-old male presented with persistent nausea and vomiting. His medical history included a partial gastrectomy with Billroth II reconstruction in the neonatal period for gastric atresia. Laboratory evaluation revealed leukocytosis (15,000/µL) and a cholestatic liver profile: alkaline phosphatase 140 U/L, AST 241 U/L, ALT 275 U/L, total bilirubin 5.5 mg/dL, and direct bilirubin 2.1 mg/dL. Magnetic resonance cholangiopancreatography (MRCP) demonstrated intrahepatic biliary dilation and a filling defect in the distal common bile duct (CBD) (Image 1). Initial ERCP using a single-balloon enteroscope (SBE) with a distal cap was unsuccessful due to the inability to locate the major papilla. With worsening cholestasis (total bilirubin 9.4 mg/dL, direct bilirubin 6.0 mg/dL), a repeat ERCP was performed using a fluoroscopy-guided rendezvous approach in collaboration with interventional radiology. Endoscopy confirmed a Billroth II anatomy with an elongated afferent limb measuring 160 cm from the incisors. Using SBE with a distal cap, the papilla was accessed and cannulated. Cholangiography revealed an obstructing stone. A sphincterotomy was performed, followed by placement of a fully covered self-expanding metal stent (SEMS). A tattoo was placed near the biliary limb to aid future access (Image 2). At follow-up ERCP, the biliary limb was readily identified via the tattoo. The SEMS remained widely patent. Cannulation through the stent allowed balloon extraction of copious sludge and an 8 mm stone. The stent was then removed. The patient remained asymptomatic with no recurrence at one-month follow-up.
Discussion: This case illustrates the diagnostic and therapeutic complexities of ERCP in patients with surgically altered anatomy. A detailed pre-procedural review of history and imaging is vital to recognizing anatomical variants and guiding endoscopic strategy. Tailored approaches and multidisciplinary collaboration are essential for optimizing outcomes in this technically challenging population.
References: Li JS et al. Saudi J Gastroenterol. 2019. Pribadi RR et al. J Dig Dis. 2019.
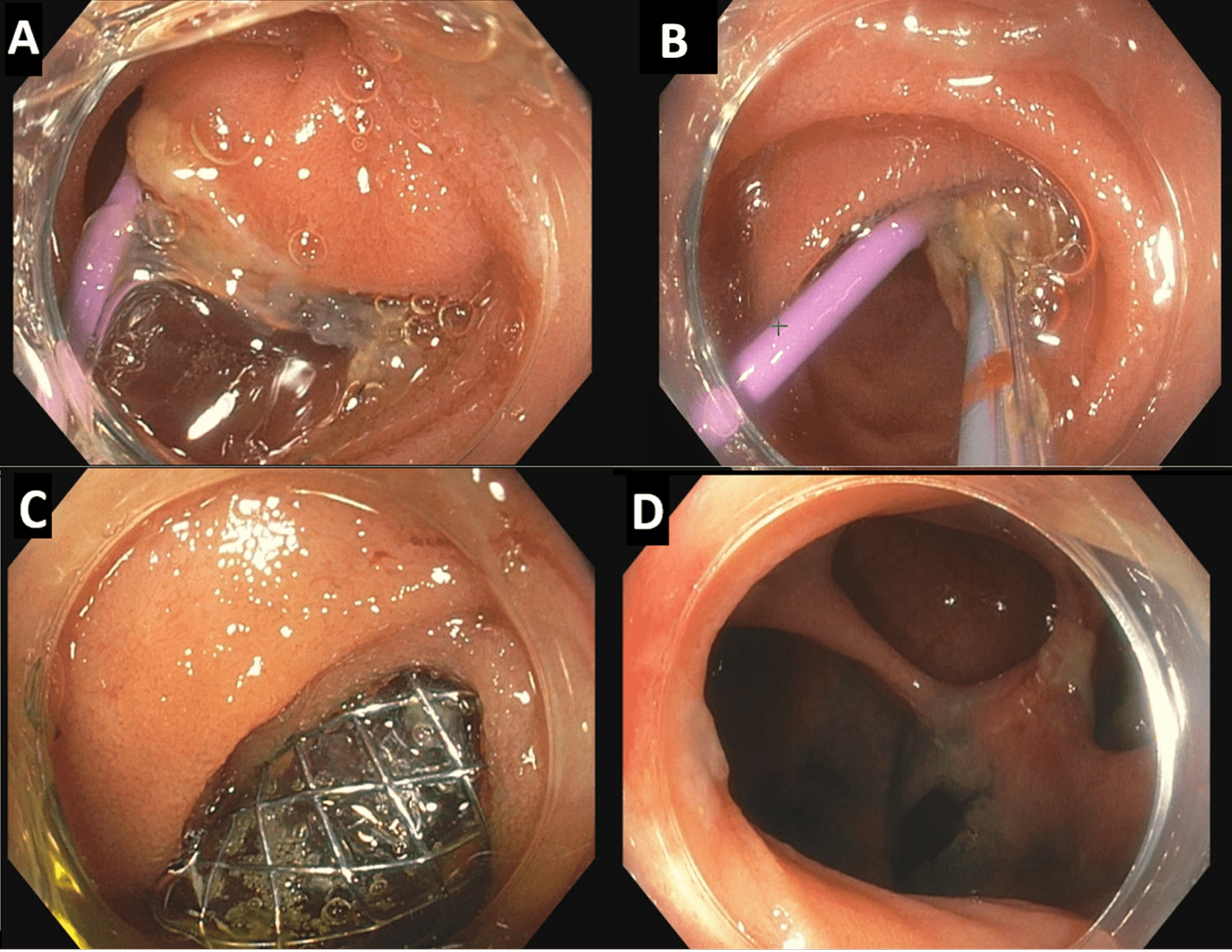
Figure: Image 1: A) Magnetic resonance imaging showing biliary duct dilation . B) Magnetic resonance cholangiopancreatography (MRCP) showing common bile duct filling defects
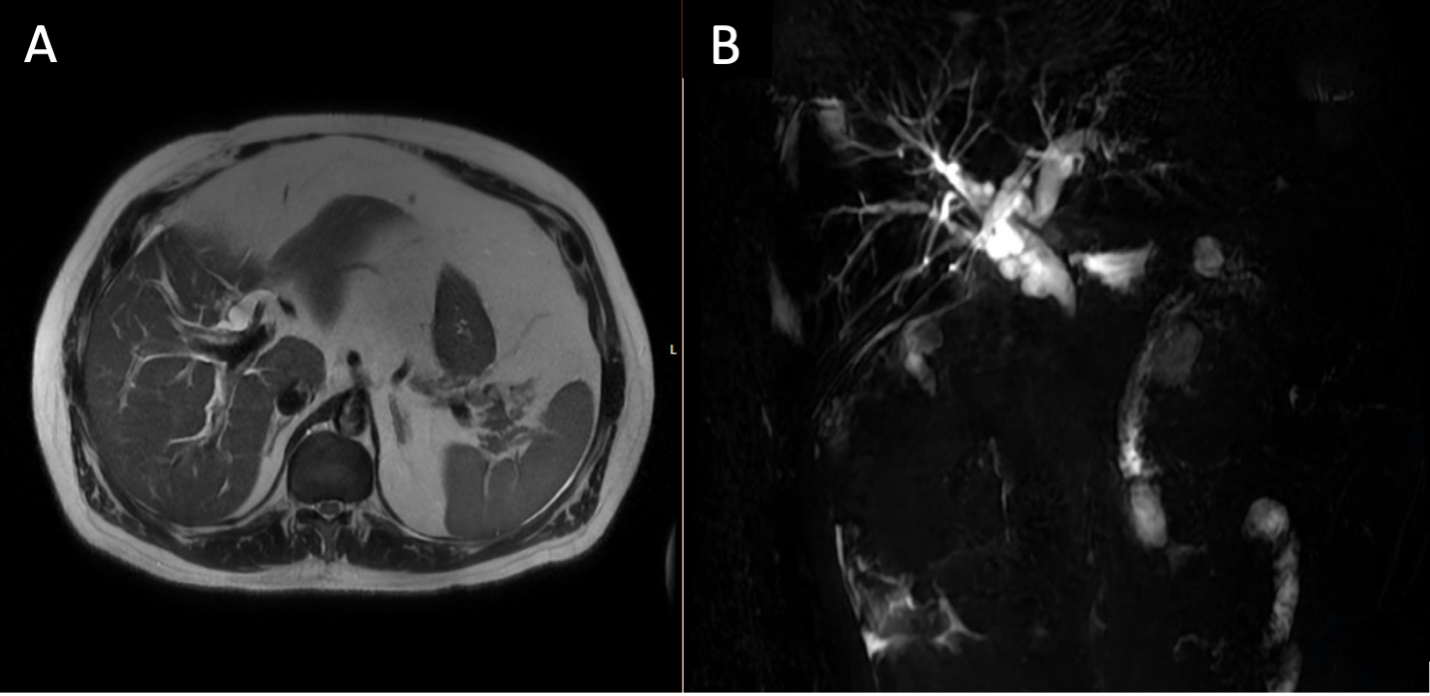
Figure: Image 2: Endoscopic retrograde cholangiopancreatography (ERCP) A) Major ampulla at the blind end of the biliary limb with Interventional Radiology rendezvous catheter (~ 160 cm from the incisors). B) Biliary Cannulation achieved via retrograde approach using sphincterotome. C) Placement of fully covered metal stent. D) The proximal part of the biliary limb tattooed for repeated ERCP
Disclosures:
Pearl Aggarwal indicated no relevant financial relationships.
Michael Liu indicated no relevant financial relationships.
Fatema Dinary indicated no relevant financial relationships.
Sara Saleh indicated no relevant financial relationships.
Ibrahim Maghari indicated no relevant financial relationships.
Fazel Dinary indicated no relevant financial relationships.
Pearl Aggarwal, MD1, Michael Liu, MD2, Fatema Dinary, 3, Sara Saleh, MD4, Ibrahim Maghari, MD5, Fazel Dinary, MD6. P3611 - ERCP in Billroth II Anatomy: Navigating the Challenges of Surgically Altered Gastrointestinal Anatomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
