Monday Poster Session
Category: Interventional Endoscopy
P3610 - Endoscopic Coloenteric Anastomosis Using Lumen-Apposing Metal Stent for Malignant Small Bowel Obstruction in Metastatic Colon Adenocarcinoma: When to Intervene and When to Reconsider
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Pearl Aggarwal, MD (she/her/hers)
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Pearl Aggarwal, MD1, Farah Khraisat, MD2, Saqr Alsakarneh, MD, MSc3, Fatema Dinary, 4, Ibrahim Maghari, MD5, Sara Saleh, MD6, Fazel Dinary, MD7
1Cleveland Clinic, Cleveland, OH; 2University of Florida, Jacksonville, FL; 3Mayo Clinic, Rochester, MN; 4Case Western Reserve University, Westlake, OH; 5Parkview Medical Center, Fort Wayne, IN; 6Hashemite University, Zarqa, Az Zarqa', Jordan; 7University Hospital, Cleveland, OH
Introduction: Malignant small bowel obstruction (MSBO) is a common complication of advanced gastrointestinal malignancies, particularly in the setting of peritoneal carcinomatosis. When surgery and conventional stenting are not feasible, endoscopic palliation using lumen-apposing metal stents (LAMS) offers a minimally invasive strategy for bowel decompression and symptom control.
Case Description/
Methods:
A 76-year-old woman with recurrent stage IV colon adenocarcinoma and peritoneal carcinomatosis presented with abdominal pain, nausea, and obstipation. Vital signs were stable. Physical exam revealed abdominal distention, tenderness, and hypoactive bowel sounds. Labs showed WBC 8.4 × 10³/μL, hemoglobin 8.4 g/dL (baseline), and normal liver and renal function.
CT of the abdomen and pelvis demonstrated high-grade small bowel obstruction at a prior ileocolonic anastomosis with dilated proximal loops (Image 1A). She was deemed a poor surgical candidate. Palliative options included venting gastrostomy with TPN versus endoscopic bypass. The patient elected for endoscopic intervention.
Colonoscopy revealed high-grade, non-traversable malignant strictures at the sigmoid colon and ileocolonic anastomosis (Image 1B). Attempts at conventional stenting failed. A lower EUS-guided coloenteric anastomosis using LAMS was performed. A linear echoendoscope was advanced into the proximal sigmoid colon, where a dilated small bowel loop was identified. Under EUS and fluoroscopic guidance, a 15 mm × 10 mm electrocautery-enhanced LAMS (AXIOS) was deployed, creating a coloenteric anastomosis. Immediate feculent drainage confirmed technical success. The procedure was well-tolerated.
Post-procedural CT showed decompression and proper stent position (Image 2). The patient resumed oral intake within 24 hours and was discharged with sustained symptom relief.
Discussion: This case highlights LAMS as a feasible and effective palliative option in MSBO when traditional endoscopic or surgical interventions are not viable. Emerging data support its use in malignant obstruction with high technical and clinical success rates. In this patient with extensive peritoneal disease and failed prior therapies, endoscopic coloenteric bypass provided meaningful symptom control. Multidisciplinary planning and careful patient selection are essential to optimize outcomes (Demarest et al., 2023; van der Merwe et al., 2022).
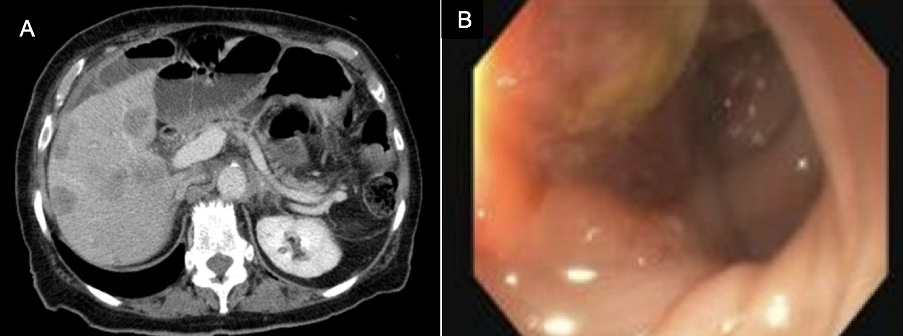
Figure: Image 1: A Computed Tomography of the abdomen/pelvis; B: endoscopic view revealed high-grade small bowel obstruction at a prior ileocolonic anastomosis, with dilated proximal loops

Figure: Image 2: Computed Tomography of the abdomen/pelvis confirming immediate feculent drainage confirmed successful stent placement.
Disclosures:
Pearl Aggarwal indicated no relevant financial relationships.
Farah Khraisat indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Fatema Dinary indicated no relevant financial relationships.
Ibrahim Maghari indicated no relevant financial relationships.
Sara Saleh indicated no relevant financial relationships.
Fazel Dinary indicated no relevant financial relationships.
Pearl Aggarwal, MD1, Farah Khraisat, MD2, Saqr Alsakarneh, MD, MSc3, Fatema Dinary, 4, Ibrahim Maghari, MD5, Sara Saleh, MD6, Fazel Dinary, MD7. P3610 - Endoscopic Coloenteric Anastomosis Using Lumen-Apposing Metal Stent for Malignant Small Bowel Obstruction in Metastatic Colon Adenocarcinoma: When to Intervene and When to Reconsider, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2University of Florida, Jacksonville, FL; 3Mayo Clinic, Rochester, MN; 4Case Western Reserve University, Westlake, OH; 5Parkview Medical Center, Fort Wayne, IN; 6Hashemite University, Zarqa, Az Zarqa', Jordan; 7University Hospital, Cleveland, OH
Introduction: Malignant small bowel obstruction (MSBO) is a common complication of advanced gastrointestinal malignancies, particularly in the setting of peritoneal carcinomatosis. When surgery and conventional stenting are not feasible, endoscopic palliation using lumen-apposing metal stents (LAMS) offers a minimally invasive strategy for bowel decompression and symptom control.
Case Description/
Methods:
A 76-year-old woman with recurrent stage IV colon adenocarcinoma and peritoneal carcinomatosis presented with abdominal pain, nausea, and obstipation. Vital signs were stable. Physical exam revealed abdominal distention, tenderness, and hypoactive bowel sounds. Labs showed WBC 8.4 × 10³/μL, hemoglobin 8.4 g/dL (baseline), and normal liver and renal function.
CT of the abdomen and pelvis demonstrated high-grade small bowel obstruction at a prior ileocolonic anastomosis with dilated proximal loops (Image 1A). She was deemed a poor surgical candidate. Palliative options included venting gastrostomy with TPN versus endoscopic bypass. The patient elected for endoscopic intervention.
Colonoscopy revealed high-grade, non-traversable malignant strictures at the sigmoid colon and ileocolonic anastomosis (Image 1B). Attempts at conventional stenting failed. A lower EUS-guided coloenteric anastomosis using LAMS was performed. A linear echoendoscope was advanced into the proximal sigmoid colon, where a dilated small bowel loop was identified. Under EUS and fluoroscopic guidance, a 15 mm × 10 mm electrocautery-enhanced LAMS (AXIOS) was deployed, creating a coloenteric anastomosis. Immediate feculent drainage confirmed technical success. The procedure was well-tolerated.
Post-procedural CT showed decompression and proper stent position (Image 2). The patient resumed oral intake within 24 hours and was discharged with sustained symptom relief.
Discussion: This case highlights LAMS as a feasible and effective palliative option in MSBO when traditional endoscopic or surgical interventions are not viable. Emerging data support its use in malignant obstruction with high technical and clinical success rates. In this patient with extensive peritoneal disease and failed prior therapies, endoscopic coloenteric bypass provided meaningful symptom control. Multidisciplinary planning and careful patient selection are essential to optimize outcomes (Demarest et al., 2023; van der Merwe et al., 2022).
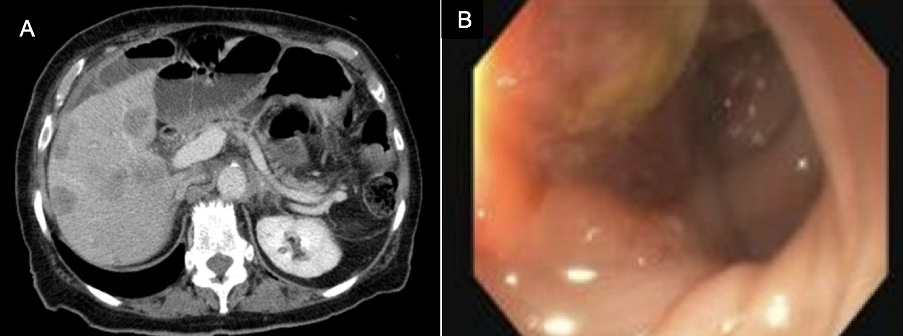
Figure: Image 1: A Computed Tomography of the abdomen/pelvis; B: endoscopic view revealed high-grade small bowel obstruction at a prior ileocolonic anastomosis, with dilated proximal loops

Figure: Image 2: Computed Tomography of the abdomen/pelvis confirming immediate feculent drainage confirmed successful stent placement.
Disclosures:
Pearl Aggarwal indicated no relevant financial relationships.
Farah Khraisat indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Fatema Dinary indicated no relevant financial relationships.
Ibrahim Maghari indicated no relevant financial relationships.
Sara Saleh indicated no relevant financial relationships.
Fazel Dinary indicated no relevant financial relationships.
Pearl Aggarwal, MD1, Farah Khraisat, MD2, Saqr Alsakarneh, MD, MSc3, Fatema Dinary, 4, Ibrahim Maghari, MD5, Sara Saleh, MD6, Fazel Dinary, MD7. P3610 - Endoscopic Coloenteric Anastomosis Using Lumen-Apposing Metal Stent for Malignant Small Bowel Obstruction in Metastatic Colon Adenocarcinoma: When to Intervene and When to Reconsider, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
