Monday Poster Session
Category: Interventional Endoscopy
P3600 - Novel Use of EUS-Guided Diverting Gastroduodenostomy in a Patient With Chronic Gastric Outlet Obstruction and Ulcerations Due to Post-Surgical Deformity of the Stomach With Inverted J-Shaped Positioning
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Neil Chokshi, DO
Mount Sinai Medical Center
Miami Beach, FL
Presenting Author(s)
Neil Chokshi, DO, Mohamed Karam Douedari, MD, Manuel Berzosa, MD, Kfir Ben-David, MD, Rama Tarakji, MD, MPH
Mount Sinai Medical Center, Miami Beach, FL
Introduction: Retrosternal colonic interposition is a standard procedure for patients, particularly children, with damage/underdevelopment of the esophagus. However, many long-term complications have been reported, including gastric outlet obstruction (GOO). GOO may lead to ulceration, perforation, and fistula formation. Traditional surgical revisions can be challenging in patients with complex anatomy. We present a case highlighting the novel use of endoscopic ultrasound (EUS)-guided gastroenterostomy to treat GOO and a gastrocutaneous fistula in a patient with a significant post-surgical gastric deformity.
Case Description/
Methods: A 54-year-old woman with a history of esophagectomy and retrosternal colonic interposition following caustic ingestion as a toddler presented with one month of oral intolerance, abdominal pain, and chest wall erythema that progressed to a draining cutaneous opening. She had recently been diagnosed at another hospital with GOO and a gastrocutaneous fistula.
Initial esophagogastroduodenoscopy (EGD) showed an esophago-colonic anastomotic stricture (11mm) with ulceration. A second anastomosis at 38cm showed friable mucosa and a 5x5mm fistulous tract. Biopsies were benign. The stricture was dilated to 18mm. Fluoroscopy revealed severe gastric malpositioning, with the fundus displaced inferiorly toward the pelvis and the pylorus positioned superiorly and contralateral to the ulcerated site, forming an inverted J-shape (Figure 1).
EUS-guided gastroenterostomy was performed by accessing the most dependent portion of the stomach, puncturing the stomach wall and small bowel via 22-gauge needle, and deploying a 15x15mm lumen-apposing metal stent (LAMS) to create a gastrojejunostomy (Figure 2). Follow-up EGD showed the fistula, which was cauterized. Closer with an over-the-scope clip was unsuccessful due to fibrosis.
Discussion: The gastrojejunostomy effectively diverted gastric content away from the ulcerated anastomosis, allowing the fistula to close spontaneously. The patient remained on total parental nutrition (TPN) and proton pump inhibitors for three weeks before initiating oral intake. She gradually advanced to a full diet. Repeat EGD at two and four months showed a closed fistula and a well-positioned, patent LAMS.
This case demonstrates a successful, minimally invasive management strategy for post-surgical GOO and fistula formation in the setting of extreme gastric malrotation. EUS-guided bypass avoided the need for high-risk surgical intervention in a complex anatomical landscape.

Figure: Figure 1: Fluoroscopic image during EGD demonstrating severe gastric malpositioning. The stomach is configured in an inverted J-shape, with the fundus displaced inferiorly toward the pelvis and the pylorus located superiorly and contralateral to the ulcerated site leading to a looping of the scope
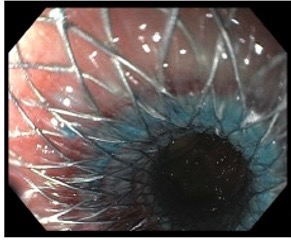
Figure: Figure 2: EGD status-post successful gastrojejunostomy with LAMS. Residual methylene blue solution can be seen traversing through the stent, demonstrating successful creation of a patent gastrojejunostomy
Disclosures:
Neil Chokshi indicated no relevant financial relationships.
Mohamed Karam Douedari indicated no relevant financial relationships.
Manuel Berzosa indicated no relevant financial relationships.
Kfir Ben-David indicated no relevant financial relationships.
Rama Tarakji indicated no relevant financial relationships.
Neil Chokshi, DO, Mohamed Karam Douedari, MD, Manuel Berzosa, MD, Kfir Ben-David, MD, Rama Tarakji, MD, MPH. P3600 - Novel Use of EUS-Guided Diverting Gastroduodenostomy in a Patient With Chronic Gastric Outlet Obstruction and Ulcerations Due to Post-Surgical Deformity of the Stomach With Inverted J-Shaped Positioning, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mount Sinai Medical Center, Miami Beach, FL
Introduction: Retrosternal colonic interposition is a standard procedure for patients, particularly children, with damage/underdevelopment of the esophagus. However, many long-term complications have been reported, including gastric outlet obstruction (GOO). GOO may lead to ulceration, perforation, and fistula formation. Traditional surgical revisions can be challenging in patients with complex anatomy. We present a case highlighting the novel use of endoscopic ultrasound (EUS)-guided gastroenterostomy to treat GOO and a gastrocutaneous fistula in a patient with a significant post-surgical gastric deformity.
Case Description/
Methods: A 54-year-old woman with a history of esophagectomy and retrosternal colonic interposition following caustic ingestion as a toddler presented with one month of oral intolerance, abdominal pain, and chest wall erythema that progressed to a draining cutaneous opening. She had recently been diagnosed at another hospital with GOO and a gastrocutaneous fistula.
Initial esophagogastroduodenoscopy (EGD) showed an esophago-colonic anastomotic stricture (11mm) with ulceration. A second anastomosis at 38cm showed friable mucosa and a 5x5mm fistulous tract. Biopsies were benign. The stricture was dilated to 18mm. Fluoroscopy revealed severe gastric malpositioning, with the fundus displaced inferiorly toward the pelvis and the pylorus positioned superiorly and contralateral to the ulcerated site, forming an inverted J-shape (Figure 1).
EUS-guided gastroenterostomy was performed by accessing the most dependent portion of the stomach, puncturing the stomach wall and small bowel via 22-gauge needle, and deploying a 15x15mm lumen-apposing metal stent (LAMS) to create a gastrojejunostomy (Figure 2). Follow-up EGD showed the fistula, which was cauterized. Closer with an over-the-scope clip was unsuccessful due to fibrosis.
Discussion: The gastrojejunostomy effectively diverted gastric content away from the ulcerated anastomosis, allowing the fistula to close spontaneously. The patient remained on total parental nutrition (TPN) and proton pump inhibitors for three weeks before initiating oral intake. She gradually advanced to a full diet. Repeat EGD at two and four months showed a closed fistula and a well-positioned, patent LAMS.
This case demonstrates a successful, minimally invasive management strategy for post-surgical GOO and fistula formation in the setting of extreme gastric malrotation. EUS-guided bypass avoided the need for high-risk surgical intervention in a complex anatomical landscape.

Figure: Figure 1: Fluoroscopic image during EGD demonstrating severe gastric malpositioning. The stomach is configured in an inverted J-shape, with the fundus displaced inferiorly toward the pelvis and the pylorus located superiorly and contralateral to the ulcerated site leading to a looping of the scope
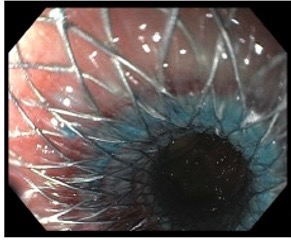
Figure: Figure 2: EGD status-post successful gastrojejunostomy with LAMS. Residual methylene blue solution can be seen traversing through the stent, demonstrating successful creation of a patent gastrojejunostomy
Disclosures:
Neil Chokshi indicated no relevant financial relationships.
Mohamed Karam Douedari indicated no relevant financial relationships.
Manuel Berzosa indicated no relevant financial relationships.
Kfir Ben-David indicated no relevant financial relationships.
Rama Tarakji indicated no relevant financial relationships.
Neil Chokshi, DO, Mohamed Karam Douedari, MD, Manuel Berzosa, MD, Kfir Ben-David, MD, Rama Tarakji, MD, MPH. P3600 - Novel Use of EUS-Guided Diverting Gastroduodenostomy in a Patient With Chronic Gastric Outlet Obstruction and Ulcerations Due to Post-Surgical Deformity of the Stomach With Inverted J-Shaped Positioning, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
