Monday Poster Session
Category: Interventional Endoscopy
P3598 - Persistence Prevails: A Multistage Battle of Bouveret Syndrome
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Jeffrey Nguyen, MD
Scripps Green Hospital
La Jolla, CA
Presenting Author(s)
Jeffrey Nguyen, MD, Olivia Lanser, MD, Sushrut Thiruvengadam, MD, Matthew Skinner, MD
Scripps Green Hospital, La Jolla, CA
Introduction: Bouveret syndrome is a special variant of gallstone ileus causing gastric outlet obstruction (GOO) due to a large gallstone impacted in the duodenum or pylorus via a cholecystoenteric fistula. Endoscopic management is typically first-line though success is variable, sometimes requiring surgical intervention which is associated with higher morbidity/mortality. This case highlights the value of persistence in endoscopic management of Bouveret syndrome.
Case Description/
Methods: A 73-year-old man with remote asymptomatic cholelithiasis presented with worsening epigastric pain, nausea/vomiting and unintentional weight loss. Labs revealed WBC 13.1, alkaline phosphatase 202 and AST/ALT 62/78. CT scan showed a cholecystoduodenal fistula, a 4.9cm gallstone in the duodenum and gastric distention concerning for GOO from Bouveret syndrome. Initial EGD revealed a large dense crystalline stone lodged at the distal antrum/duodenal bulb, prolapsing through the pylorus making electrohydraulic lithotripsy (EHL) very challenging. Each upper endoscopy was limited by the number of probes available, however after 4 attempts, with the use of 29 EHL probes applied on high settings, rat-tooth/biopsy forceps, basket crusher and roth net, the obstructive stone was successfully fragmented and retrieved with an intact duodenal wall without ulceration or perforation. Given that the stone spanned the pelvic channel, the appropriate technical approach may have been challenging to determine surgically.
Discussion: Bouveret syndrome causes GOO due to gallstone impaction in the duodenum or pylorus via a cholecystoenteric fistula. It represents 1-3% of gallstone ileus cases with risk factors of advanced age, female sex, recurrent cholelithiasis or stones >2cm. Symptoms include abdominal pain, nausea/vomiting with imaging often revealing Rigler’s triad: pneumobilia, ectopic gallstone and obstruction. Management includes endoscopic lithotripsy (mechanical, laser, ESWL or EHL) or surgery (enterolithotomy, gastrotomy or complex procedures like Whipple). Surgery treats both the stone and fistula, however the larger the stone, the longer the surgical incision to remove the stone, which increases the risk of morbidity due to leak. Endoscopic management like EHL has emerged as a less invasive alternative but may require multiple sessions. This case demonstrates the value of persistence, proving that multiple endoscopic sessions with EHL can successfully fragment larger stones, allowing for the avoidance of surgical intervention.
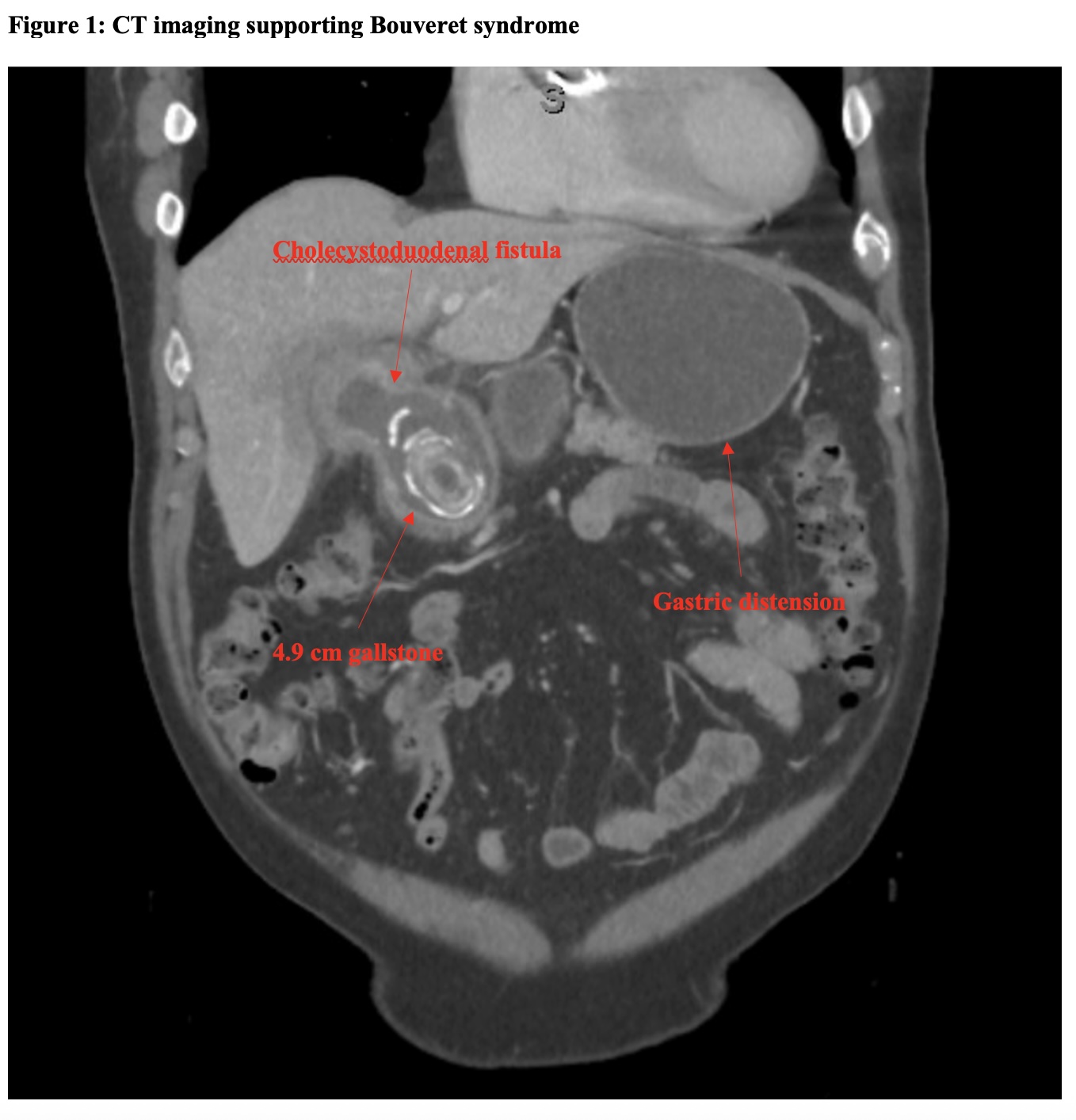
Figure: Figure 1: CT imaging supporting Bouveret syndrome
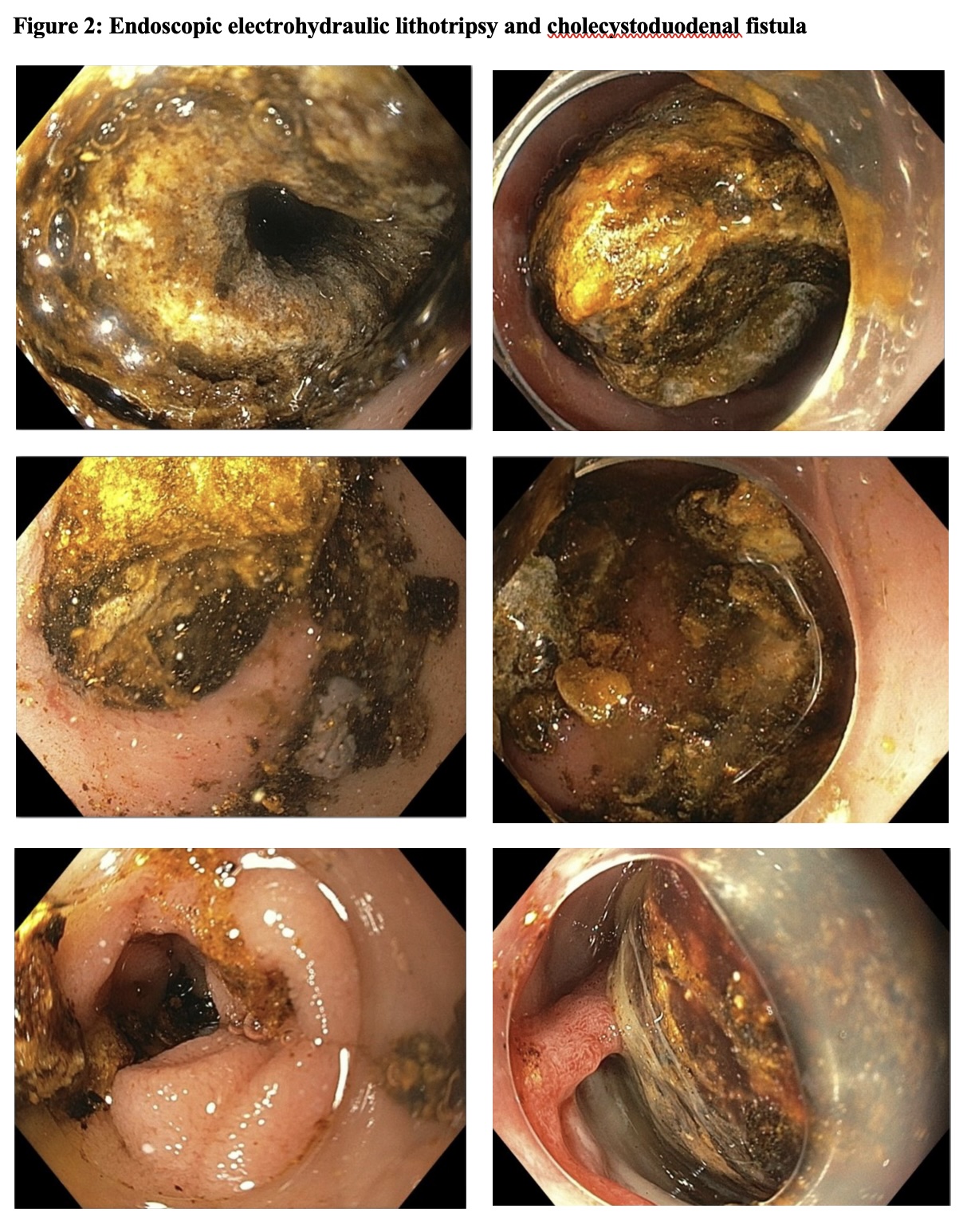
Figure: Figure 2: Endoscopic electrohydraulic lithotripsy and cholecystoduodenal fistula
Disclosures:
Jeffrey Nguyen indicated no relevant financial relationships.
Olivia Lanser indicated no relevant financial relationships.
Sushrut Thiruvengadam indicated no relevant financial relationships.
Matthew Skinner: Boston scientific – Consultant. Microtech – Consultant.
Jeffrey Nguyen, MD, Olivia Lanser, MD, Sushrut Thiruvengadam, MD, Matthew Skinner, MD. P3598 - Persistence Prevails: A Multistage Battle of Bouveret Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Scripps Green Hospital, La Jolla, CA
Introduction: Bouveret syndrome is a special variant of gallstone ileus causing gastric outlet obstruction (GOO) due to a large gallstone impacted in the duodenum or pylorus via a cholecystoenteric fistula. Endoscopic management is typically first-line though success is variable, sometimes requiring surgical intervention which is associated with higher morbidity/mortality. This case highlights the value of persistence in endoscopic management of Bouveret syndrome.
Case Description/
Methods: A 73-year-old man with remote asymptomatic cholelithiasis presented with worsening epigastric pain, nausea/vomiting and unintentional weight loss. Labs revealed WBC 13.1, alkaline phosphatase 202 and AST/ALT 62/78. CT scan showed a cholecystoduodenal fistula, a 4.9cm gallstone in the duodenum and gastric distention concerning for GOO from Bouveret syndrome. Initial EGD revealed a large dense crystalline stone lodged at the distal antrum/duodenal bulb, prolapsing through the pylorus making electrohydraulic lithotripsy (EHL) very challenging. Each upper endoscopy was limited by the number of probes available, however after 4 attempts, with the use of 29 EHL probes applied on high settings, rat-tooth/biopsy forceps, basket crusher and roth net, the obstructive stone was successfully fragmented and retrieved with an intact duodenal wall without ulceration or perforation. Given that the stone spanned the pelvic channel, the appropriate technical approach may have been challenging to determine surgically.
Discussion: Bouveret syndrome causes GOO due to gallstone impaction in the duodenum or pylorus via a cholecystoenteric fistula. It represents 1-3% of gallstone ileus cases with risk factors of advanced age, female sex, recurrent cholelithiasis or stones >2cm. Symptoms include abdominal pain, nausea/vomiting with imaging often revealing Rigler’s triad: pneumobilia, ectopic gallstone and obstruction. Management includes endoscopic lithotripsy (mechanical, laser, ESWL or EHL) or surgery (enterolithotomy, gastrotomy or complex procedures like Whipple). Surgery treats both the stone and fistula, however the larger the stone, the longer the surgical incision to remove the stone, which increases the risk of morbidity due to leak. Endoscopic management like EHL has emerged as a less invasive alternative but may require multiple sessions. This case demonstrates the value of persistence, proving that multiple endoscopic sessions with EHL can successfully fragment larger stones, allowing for the avoidance of surgical intervention.
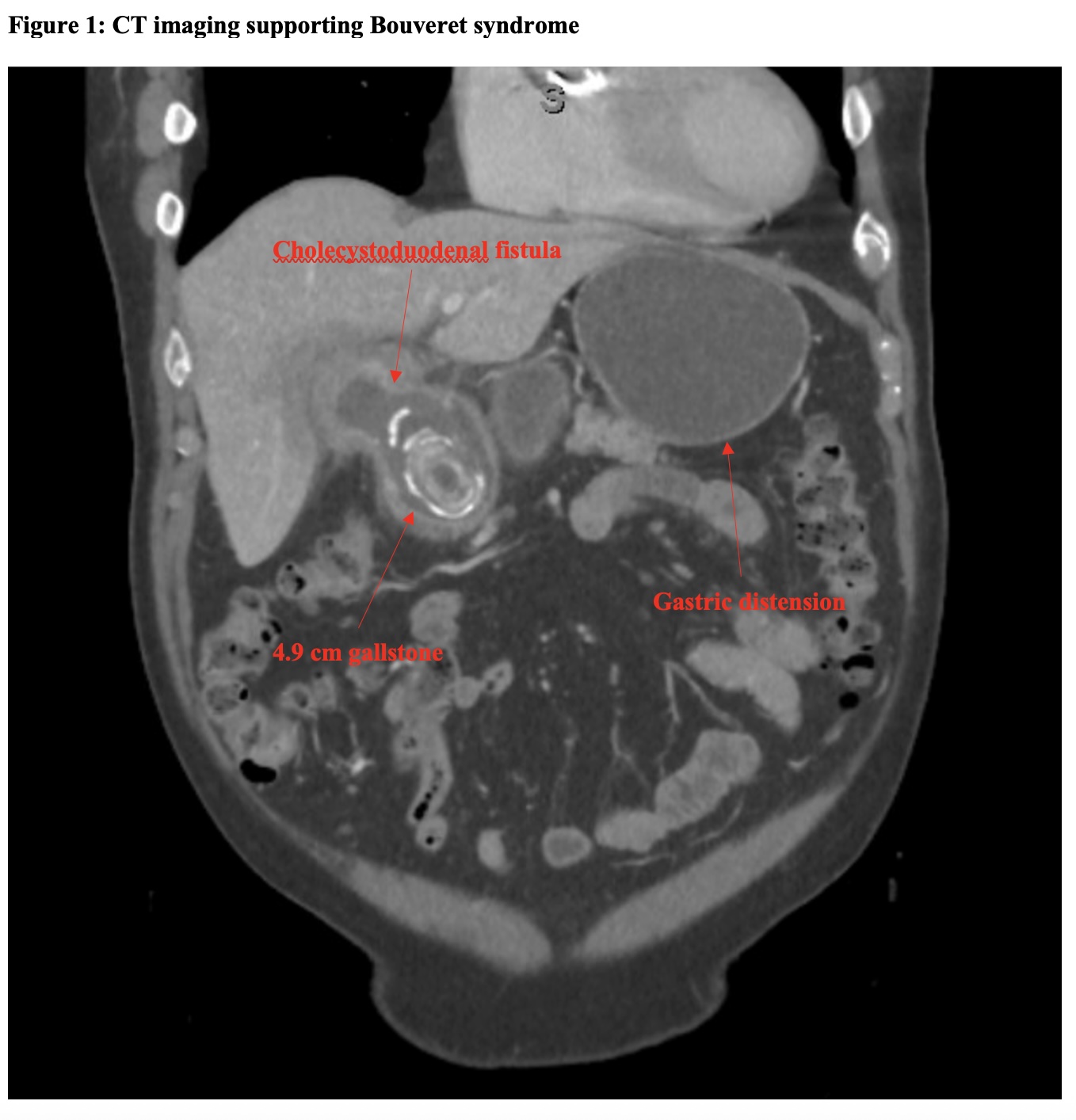
Figure: Figure 1: CT imaging supporting Bouveret syndrome
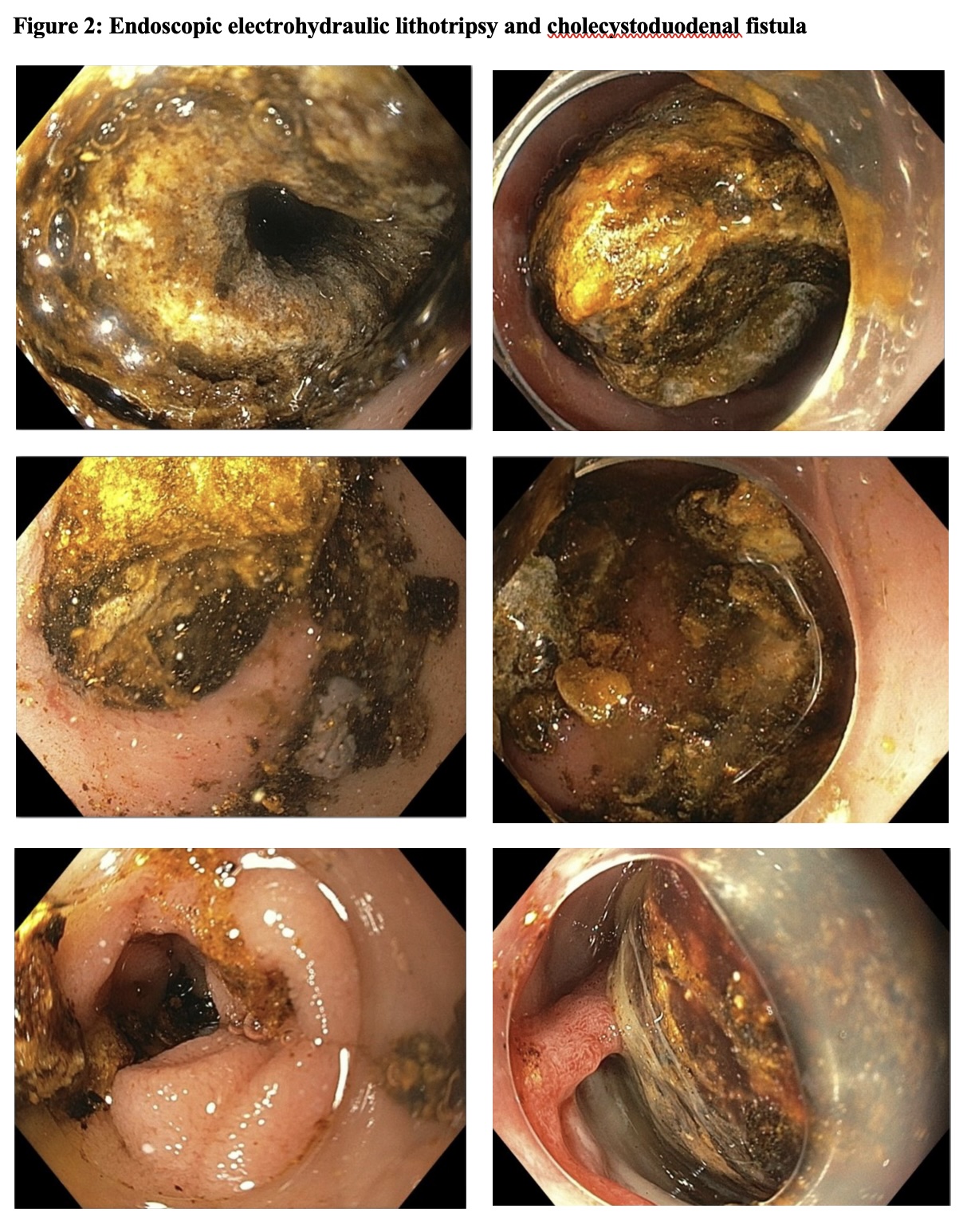
Figure: Figure 2: Endoscopic electrohydraulic lithotripsy and cholecystoduodenal fistula
Disclosures:
Jeffrey Nguyen indicated no relevant financial relationships.
Olivia Lanser indicated no relevant financial relationships.
Sushrut Thiruvengadam indicated no relevant financial relationships.
Matthew Skinner: Boston scientific – Consultant. Microtech – Consultant.
Jeffrey Nguyen, MD, Olivia Lanser, MD, Sushrut Thiruvengadam, MD, Matthew Skinner, MD. P3598 - Persistence Prevails: A Multistage Battle of Bouveret Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
