Monday Poster Session
Category: Interventional Endoscopy
P3592 - Hemostatic Hydrogel in Gastric Variceal Management
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rutvi Katariya, MD (she/her/hers)
Atrium Health Carolinas Medical Center
Charlotte, NC
Presenting Author(s)
Rutvi Katariya, MD, Andrew M. Dries, MD
Atrium Health Carolinas Medical Center, Charlotte, NC
Introduction: Gastric varices occur at a rate of 15-20% and are often associated with higher bleeding rates and worse patient outcomes compared to esophageal varices. Treatment options include band ligation, cyanoacrylate injection, endoscopic ultrasound (EUS) guided coiling, or a combination therapy of coiling and CYA. Here we use a hemostatic hydrogel, comprised of self-assembling peptides, in the treatment of gastric varices.
Case Description/
Methods: A 77-year-old female with recent NSAID overuse and cirrhosis without proper prior evaluation is admitted for two episodes of hematemesis and melenic stools. She was resuscitated with two units of packed red blood cells and CTA imaging showed no active bleeding. An EGD showed small non-bleeding grade 1 varices in the lower third esophagus and a larger type I isolated gastric varix with stigmata of recent hemorrhage. Initially, balloon-occluded retrograde transvenous obliteration (BRTO) was considered, however it was felt that the shunt was too small to intervene on. She underwent EUS which showed medium sized gastric varices with multiple collaterals but only one vessel in the submucosa measuring 7 mm in maximum diameter. The varix was punctured with a 19-gauge needle and an 8 mm coil was deployed in excellent position under direct visualization. Sclerosis was induced by a 3 mL intravariceal injection of hemostatic hydrogel with complete cessation of flow by doppler. After intervention, no further GI bleeding was noted in the days following.
Discussion: There are several available treatment approaches to gastric varices, of which cyanoacrylate (CYA) injection is the most utilized. The most feared complication of CYA is systemic embolization either as a stroke or pulmonary embolus. Here, we presented the use of hemostatic hydrogel which consists of synthetic peptides with acidic properties that, once in contact with blood, are neutralized and form a fibrin-mesh. It is currently used for management of bleeding after endoscopic submucosal resection. By mimicking the human extracellular matrix, coagulation is induced and a physical seal is created with subsequent cessation of intravariceal blood flow. Some forms currently on the market utilize peptides such as the RADA16 peptide, which is a 16-amino acid chain naturally occurring in the body. Novel approaches such as this hemostatic hydrogel may provide a safer management technique compared to current standard of care after additional testing and comparison for validated use.
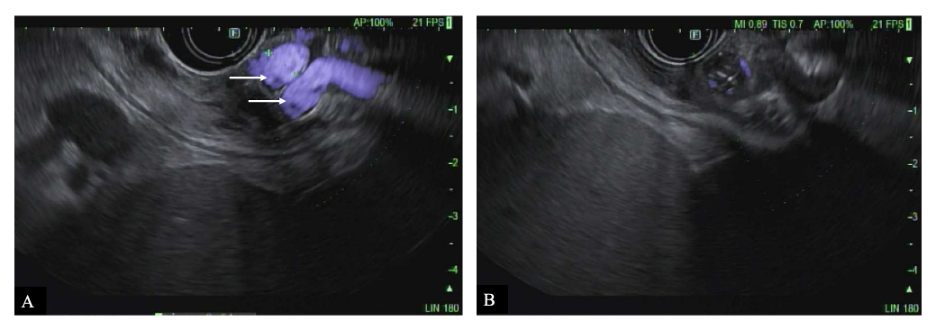
Figure: Figure 1: Endoscopic ultrasound-guided coil embolization and sclerotherapy with hydrostatic gel. (A) Endoscopic ultrasound image showing gastric collateral vessels (arrows); (B) Complete cessation of variceal flow after deployment of coil and injection of hemostatic hydrogel.
Disclosures:
Rutvi Katariya indicated no relevant financial relationships.
Andrew Dries indicated no relevant financial relationships.
Rutvi Katariya, MD, Andrew M. Dries, MD. P3592 - Hemostatic Hydrogel in Gastric Variceal Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Atrium Health Carolinas Medical Center, Charlotte, NC
Introduction: Gastric varices occur at a rate of 15-20% and are often associated with higher bleeding rates and worse patient outcomes compared to esophageal varices. Treatment options include band ligation, cyanoacrylate injection, endoscopic ultrasound (EUS) guided coiling, or a combination therapy of coiling and CYA. Here we use a hemostatic hydrogel, comprised of self-assembling peptides, in the treatment of gastric varices.
Case Description/
Methods: A 77-year-old female with recent NSAID overuse and cirrhosis without proper prior evaluation is admitted for two episodes of hematemesis and melenic stools. She was resuscitated with two units of packed red blood cells and CTA imaging showed no active bleeding. An EGD showed small non-bleeding grade 1 varices in the lower third esophagus and a larger type I isolated gastric varix with stigmata of recent hemorrhage. Initially, balloon-occluded retrograde transvenous obliteration (BRTO) was considered, however it was felt that the shunt was too small to intervene on. She underwent EUS which showed medium sized gastric varices with multiple collaterals but only one vessel in the submucosa measuring 7 mm in maximum diameter. The varix was punctured with a 19-gauge needle and an 8 mm coil was deployed in excellent position under direct visualization. Sclerosis was induced by a 3 mL intravariceal injection of hemostatic hydrogel with complete cessation of flow by doppler. After intervention, no further GI bleeding was noted in the days following.
Discussion: There are several available treatment approaches to gastric varices, of which cyanoacrylate (CYA) injection is the most utilized. The most feared complication of CYA is systemic embolization either as a stroke or pulmonary embolus. Here, we presented the use of hemostatic hydrogel which consists of synthetic peptides with acidic properties that, once in contact with blood, are neutralized and form a fibrin-mesh. It is currently used for management of bleeding after endoscopic submucosal resection. By mimicking the human extracellular matrix, coagulation is induced and a physical seal is created with subsequent cessation of intravariceal blood flow. Some forms currently on the market utilize peptides such as the RADA16 peptide, which is a 16-amino acid chain naturally occurring in the body. Novel approaches such as this hemostatic hydrogel may provide a safer management technique compared to current standard of care after additional testing and comparison for validated use.
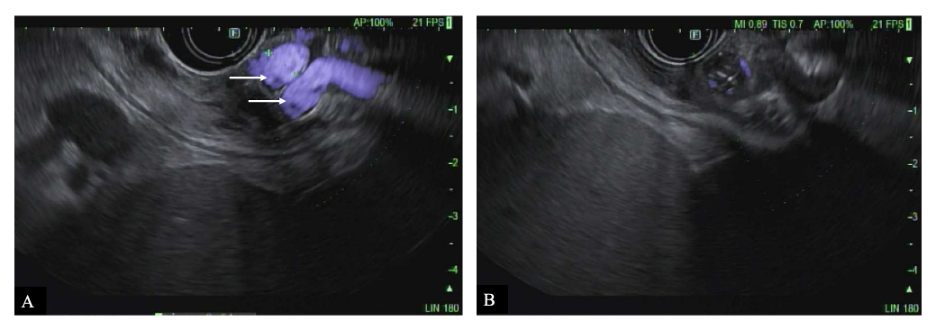
Figure: Figure 1: Endoscopic ultrasound-guided coil embolization and sclerotherapy with hydrostatic gel. (A) Endoscopic ultrasound image showing gastric collateral vessels (arrows); (B) Complete cessation of variceal flow after deployment of coil and injection of hemostatic hydrogel.
Disclosures:
Rutvi Katariya indicated no relevant financial relationships.
Andrew Dries indicated no relevant financial relationships.
Rutvi Katariya, MD, Andrew M. Dries, MD. P3592 - Hemostatic Hydrogel in Gastric Variceal Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
