Monday Poster Session
Category: Interventional Endoscopy
P3568 - Obscure Yet Deadly: Case-Based Review of Gastric Dieulafoy’s Lesion and the Role of Early Endoscopic Management
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Arshiya Shabnam, MD
New York Medical College
Denville, NJ
Presenting Author(s)
Arshiya Shabnam, MD1, Amjed Abdel Al, MD2, Ameera Ince, MBBS3, Rayees A. Konduru, MD4, Frank Ruiz, MD5
1New York Medical College, Denville, NJ; 2Jordan University of Science and Technology, Alramtha, Irbid, Jordan; 3Victoria University of Barbados, School of Medicine, Warrens, Saint Michael, Barbados; 4NewYork-Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 5New York Medical College, Rutherford, NJ
Introduction: Dieulafoy lesions (DLs) are uncommon causes of upper gastrointestinal bleeding, seen in 1–2% of cases. First described by Georges Dieulafoy in 1898, they are large submucosal arteries eroding through a small mucosal defect. The proximal stomach, especially the lesser curvature near the gastroesophageal junction, is the most common site . Though DLs can occur in the duodenum, jejunum, colon, and rectum. DLs typically present with hematemesis or melena in patients over 50 years of age, with a 2:1 male predominance. Around 90% have comorbidities such as cardiovascular disease, hypertension, renal disease, or alcohol use disorder. Diagnosis can be challenging due to its rarity, especially in obscure or recurrent GI bleeding. Endoscopy is the gold standard, with effective hemostasis via epinephrine injection, thermal coagulation, or hemoclipping.
Case Description/
Methods: Case 1: A 38-year-old Hispanic female with hypertension and peptic ulcer disease presented with hematemesis and reflux. She used NSAIDs. Labs showed anemia; EGD revealed oozing DLs in the gastric antrum. Hemostasis was achieved with epinephrine, bipolar coagulation, and hemoclipping. Biopsy confirmed H. pylori gastritis. She started PPIs, and follow-up EGD showed healing.
Case 2: A 54-year-old Hispanic male with GERD presented with persistent reflux, followed by hematemesis weeks after a colonoscopy. EGD revealed a spurting DL at the gastroesophageal junction. Hemostasis was achieved with epinephrine and clipping. Gastritis and non-bleeding gastric polyps were noted. Biopsies were taken. Treated with PPIs and no recurrence on follow up.
Discussion: DLs cause acute GI hemorrhage with minimal mucosal disruption. Though more common in older males, younger patients with NSAID use or H. pylori are also at risk . Case 1 shows successful early intervention. Case 2 highlights diagnostic challenges due to coexisting pathology.
Endoscopic therapy is effective in >90% of cases, though initial diagnostic rates vary (49–92%). Repeat endoscopy or imaging may be needed. Diagnosis relies on identifying a small mucosal defect with active bleeding, protruding vessel, or clot. Combination therapy is more effective than monotherapy. Both patients had favorable outcomes with no recurrence. H. pylori eradication and PPIs prompt recovery and reduce recurrence.
Despite its rarity, DLs should be considered in unexplained or recurrent upper GI bleeding. Prompt endoscopic identification and treatment reduce morbidity and mortality.
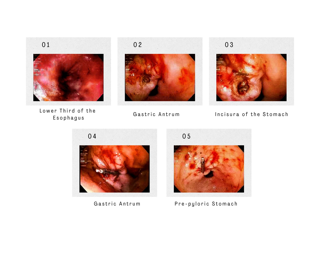
Figure: Dieulafoy lesion of the stomach, Case 1: The above images demonstrate the findings of a Dieulafoy lesion on upper Endoscopy with oozing bleeding and stigmata of recent bleeding on the gastric antrum of the stomach
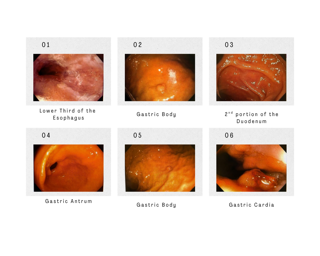
Figure: Dieulafoy lesion of the stomach, Case 2: The above images demonstrates the findings of a Dieulafoy lesion with spurting bleeding and stigmata of recent bleeding at the gastroesophageal junction
Disclosures:
Arshiya Shabnam indicated no relevant financial relationships.
Amjed Abdel Al indicated no relevant financial relationships.
Ameera Ince indicated no relevant financial relationships.
Rayees Konduru indicated no relevant financial relationships.
Frank Ruiz indicated no relevant financial relationships.
Arshiya Shabnam, MD1, Amjed Abdel Al, MD2, Ameera Ince, MBBS3, Rayees A. Konduru, MD4, Frank Ruiz, MD5. P3568 - Obscure Yet Deadly: Case-Based Review of Gastric Dieulafoy’s Lesion and the Role of Early Endoscopic Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1New York Medical College, Denville, NJ; 2Jordan University of Science and Technology, Alramtha, Irbid, Jordan; 3Victoria University of Barbados, School of Medicine, Warrens, Saint Michael, Barbados; 4NewYork-Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 5New York Medical College, Rutherford, NJ
Introduction: Dieulafoy lesions (DLs) are uncommon causes of upper gastrointestinal bleeding, seen in 1–2% of cases. First described by Georges Dieulafoy in 1898, they are large submucosal arteries eroding through a small mucosal defect. The proximal stomach, especially the lesser curvature near the gastroesophageal junction, is the most common site . Though DLs can occur in the duodenum, jejunum, colon, and rectum. DLs typically present with hematemesis or melena in patients over 50 years of age, with a 2:1 male predominance. Around 90% have comorbidities such as cardiovascular disease, hypertension, renal disease, or alcohol use disorder. Diagnosis can be challenging due to its rarity, especially in obscure or recurrent GI bleeding. Endoscopy is the gold standard, with effective hemostasis via epinephrine injection, thermal coagulation, or hemoclipping.
Case Description/
Methods: Case 1: A 38-year-old Hispanic female with hypertension and peptic ulcer disease presented with hematemesis and reflux. She used NSAIDs. Labs showed anemia; EGD revealed oozing DLs in the gastric antrum. Hemostasis was achieved with epinephrine, bipolar coagulation, and hemoclipping. Biopsy confirmed H. pylori gastritis. She started PPIs, and follow-up EGD showed healing.
Case 2: A 54-year-old Hispanic male with GERD presented with persistent reflux, followed by hematemesis weeks after a colonoscopy. EGD revealed a spurting DL at the gastroesophageal junction. Hemostasis was achieved with epinephrine and clipping. Gastritis and non-bleeding gastric polyps were noted. Biopsies were taken. Treated with PPIs and no recurrence on follow up.
Discussion: DLs cause acute GI hemorrhage with minimal mucosal disruption. Though more common in older males, younger patients with NSAID use or H. pylori are also at risk . Case 1 shows successful early intervention. Case 2 highlights diagnostic challenges due to coexisting pathology.
Endoscopic therapy is effective in >90% of cases, though initial diagnostic rates vary (49–92%). Repeat endoscopy or imaging may be needed. Diagnosis relies on identifying a small mucosal defect with active bleeding, protruding vessel, or clot. Combination therapy is more effective than monotherapy. Both patients had favorable outcomes with no recurrence. H. pylori eradication and PPIs prompt recovery and reduce recurrence.
Despite its rarity, DLs should be considered in unexplained or recurrent upper GI bleeding. Prompt endoscopic identification and treatment reduce morbidity and mortality.
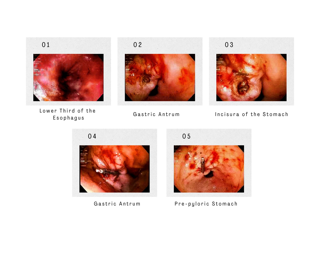
Figure: Dieulafoy lesion of the stomach, Case 1: The above images demonstrate the findings of a Dieulafoy lesion on upper Endoscopy with oozing bleeding and stigmata of recent bleeding on the gastric antrum of the stomach
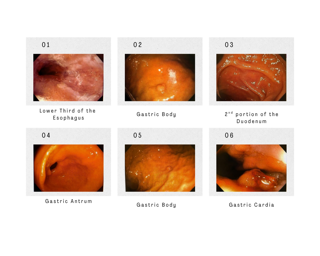
Figure: Dieulafoy lesion of the stomach, Case 2: The above images demonstrates the findings of a Dieulafoy lesion with spurting bleeding and stigmata of recent bleeding at the gastroesophageal junction
Disclosures:
Arshiya Shabnam indicated no relevant financial relationships.
Amjed Abdel Al indicated no relevant financial relationships.
Ameera Ince indicated no relevant financial relationships.
Rayees Konduru indicated no relevant financial relationships.
Frank Ruiz indicated no relevant financial relationships.
Arshiya Shabnam, MD1, Amjed Abdel Al, MD2, Ameera Ince, MBBS3, Rayees A. Konduru, MD4, Frank Ruiz, MD5. P3568 - Obscure Yet Deadly: Case-Based Review of Gastric Dieulafoy’s Lesion and the Role of Early Endoscopic Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
