Monday Poster Session
Category: Interventional Endoscopy
P3531 - The Effect of Antiplatelet on Outcomes of Endoscopic Upper GI Balloon Dilation
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Omar Arman, MD, MPH
University at Buffalo
Depew, NY
Presenting Author(s)
Omar Arman, MD, MPH1, Shunsa Tarar, DO2, Osama Alshakhatreh, MD2, Ibrahim Mohammed, MD2, Khaled Elsokary, DO2, Seth Richter, MD, FACG2
1University at Buffalo, Buffalo, NY; 2Albany Medical Center, Albany, NY
Introduction: Upper endoscopy with balloon dilation is a minimally invasive procedure to widen narrowed regions within the upper GI tract. The risk of gastrointestinal bleeding or thrombotic events is particularly elevated in patients with cardiovascular risk factors and conditions requiring anticoagulants/antiplatelets (AP/AC). This study investigates the correlation of AP therapy and outcomes after upper endoscopic balloon dilation.
Methods: This retrospective cohort study utilized a global federated health research network database, TriNetX. Patients who underwent upper endoscopy with balloon dilation were stratified into two cohorts, those on AP vs those not on AP. AP use was defined as aspirin and P2Y12 inhibitors within 7 days prior to procedure. Use of AC was an exclusion criterion for both cohorts. Both cohorts were matched for baseline demographics and co-morbidities including CKD, thrombocytopenia, and PPI use. Incidence rates for 3 outcomes; GI bleed, hospitalization and requiring blood transfusion, were assessed at 30 days with evaluation of risk differences between the cohort groups. Falsification endpoints were analyzed to assess residual confounding.
Results: In the non-AP group 598 of 14,366 had a GI bleed after balloon dilation. In contrast, the AP group 892 of 14,366 had a GI bleed. Risk difference 2%, p< 0.001.
In the non-AP group 2,713 of 14,366 were hospitalized post-balloon dilation. In contrast, the AP group 5,662 of 14,366 were hospitalized. Risk difference 20.5%, p< 0.0001.
In the non-AP group 336 of 14,366 required transfusion after balloon dilation. In contrast, the AP group 575 of 14,366 required transfusion. Risk difference 1.7%, p< 0.001.
Discussion: Our findings show that patients on AP therapy had a significantly higher rate of adverse outcomes following balloon dilation. The incidence across all studied outcomes, GI bleeding, hospitalization and need for blood transfusion was higher in the group on AP therapy in comparison the group not on AP. This raises clinical concerns regarding peri-procedural management of patients on AP therapy, suggesting the potential need for longer washout periods.
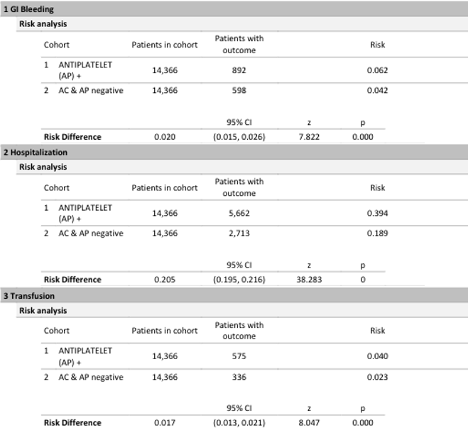
Figure: Table 1: Risk analysis for patients with and without AP with outcomes of GI bleed, hospitalization and transfusion.
Disclosures:
Omar Arman indicated no relevant financial relationships.
Shunsa Tarar indicated no relevant financial relationships.
Osama Alshakhatreh indicated no relevant financial relationships.
Ibrahim Mohammed indicated no relevant financial relationships.
Khaled Elsokary indicated no relevant financial relationships.
Seth Richter indicated no relevant financial relationships.
Omar Arman, MD, MPH1, Shunsa Tarar, DO2, Osama Alshakhatreh, MD2, Ibrahim Mohammed, MD2, Khaled Elsokary, DO2, Seth Richter, MD, FACG2. P3531 - The Effect of Antiplatelet on Outcomes of Endoscopic Upper GI Balloon Dilation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2Albany Medical Center, Albany, NY
Introduction: Upper endoscopy with balloon dilation is a minimally invasive procedure to widen narrowed regions within the upper GI tract. The risk of gastrointestinal bleeding or thrombotic events is particularly elevated in patients with cardiovascular risk factors and conditions requiring anticoagulants/antiplatelets (AP/AC). This study investigates the correlation of AP therapy and outcomes after upper endoscopic balloon dilation.
Methods: This retrospective cohort study utilized a global federated health research network database, TriNetX. Patients who underwent upper endoscopy with balloon dilation were stratified into two cohorts, those on AP vs those not on AP. AP use was defined as aspirin and P2Y12 inhibitors within 7 days prior to procedure. Use of AC was an exclusion criterion for both cohorts. Both cohorts were matched for baseline demographics and co-morbidities including CKD, thrombocytopenia, and PPI use. Incidence rates for 3 outcomes; GI bleed, hospitalization and requiring blood transfusion, were assessed at 30 days with evaluation of risk differences between the cohort groups. Falsification endpoints were analyzed to assess residual confounding.
Results: In the non-AP group 598 of 14,366 had a GI bleed after balloon dilation. In contrast, the AP group 892 of 14,366 had a GI bleed. Risk difference 2%, p< 0.001.
In the non-AP group 2,713 of 14,366 were hospitalized post-balloon dilation. In contrast, the AP group 5,662 of 14,366 were hospitalized. Risk difference 20.5%, p< 0.0001.
In the non-AP group 336 of 14,366 required transfusion after balloon dilation. In contrast, the AP group 575 of 14,366 required transfusion. Risk difference 1.7%, p< 0.001.
Discussion: Our findings show that patients on AP therapy had a significantly higher rate of adverse outcomes following balloon dilation. The incidence across all studied outcomes, GI bleeding, hospitalization and need for blood transfusion was higher in the group on AP therapy in comparison the group not on AP. This raises clinical concerns regarding peri-procedural management of patients on AP therapy, suggesting the potential need for longer washout periods.
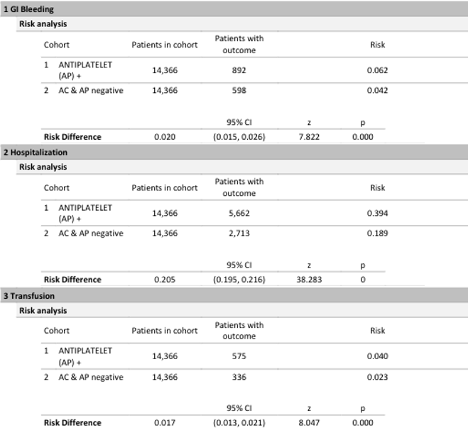
Figure: Table 1: Risk analysis for patients with and without AP with outcomes of GI bleed, hospitalization and transfusion.
Disclosures:
Omar Arman indicated no relevant financial relationships.
Shunsa Tarar indicated no relevant financial relationships.
Osama Alshakhatreh indicated no relevant financial relationships.
Ibrahim Mohammed indicated no relevant financial relationships.
Khaled Elsokary indicated no relevant financial relationships.
Seth Richter indicated no relevant financial relationships.
Omar Arman, MD, MPH1, Shunsa Tarar, DO2, Osama Alshakhatreh, MD2, Ibrahim Mohammed, MD2, Khaled Elsokary, DO2, Seth Richter, MD, FACG2. P3531 - The Effect of Antiplatelet on Outcomes of Endoscopic Upper GI Balloon Dilation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
