Monday Poster Session
Category: Infections and Microbiome
P3496 - The Hidden Culprit: Colonic Tuberculosis Presenting as Refractory Anemia in a Dialysis Patient
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ahmad Alkurd, MD
LSU Health Shreveport
Houston, TX
Presenting Author(s)
Ahmad Alkurd, MD, Michael Meador, MD, David Okuampa, MD, Kelly Schulte, DO, Omar Khan, MD, Sarav Daid, MD
LSU Health Shreveport, Shreveport, LA
Introduction: Tuberculous colitis is a rare extrapulmonary manifestation of tuberculosis (TB), often mimicking inflammatory bowel disease. We present a unique case of colonic tuberculosis diagnosed in a patient with persistent anemia receiving dialysis and transfusions for end-stage renal disease (ESRD).
Case Description/
Methods: A 77-year-old African American male with ESRD, recently started on dialysis, was referred for evaluation of persistent normocytic anemia, despite receiving multiple iron and blood transfusions. His medical history included prostate cancer (treated with chemoradiation) and squamous cell carcinoma of the tongue (status post left glossectomy). He denied gastrointestinal symptoms or overt bleeding. There was no history of incarceration, travel to endemic regions, or known tuberculosis exposure. A prior colonoscopy five years earlier had been unremarkable. Labs indicated anemia of chronic disease. EGD revealed radiation-induced changes in the esophagus and patchy gastric erythema. Colonoscopy showed multiple aphthous ulcers in the terminal ileum, cecum, and right colon. Biopsies revealed chronic active colitis with non-necrotizing granulomas. Acid-fast bacilli were detected on staining, and Mycobacterium tuberculosis was confirmed by PCR testing of the biopsies. The patient tested negative for HIV and fungal pathogens. RIPE therapy was initiated.
Discussion: Intestinal TB is rare in industrialized countries and is typically associated with HIV or immigration from endemic regions. This patient had no classic risk factors but was relatively immunocompromised due to his ESRD and malignancy history. While anemia can occur in ESRD, persistence despite transfusions warrants further evaluation. Colonic TB most commonly involves the ileocecal region and may appear endoscopically similar to Crohn’s disease, making histological confirmation important. Histology typically shows chronic inflammation with granulomas. Although caseating granulomas are classic, non-caseating granulomas—as seen here—are also consistent. The diagnosis was confirmed by acid-fast bacilli on staining and positive mycobacterial PCR testing in our patient.
Intestinal tuberculosis should be considered in the differential diagnosis of persistent anemia in immunocompromised patients even in the absence of symptoms or classic risk factors. Early diagnosis through endoscopy can guide timely treatment. This case underscores the importance of endoscopic evaluation in unexplained anemia even when more common causes seem apparent.
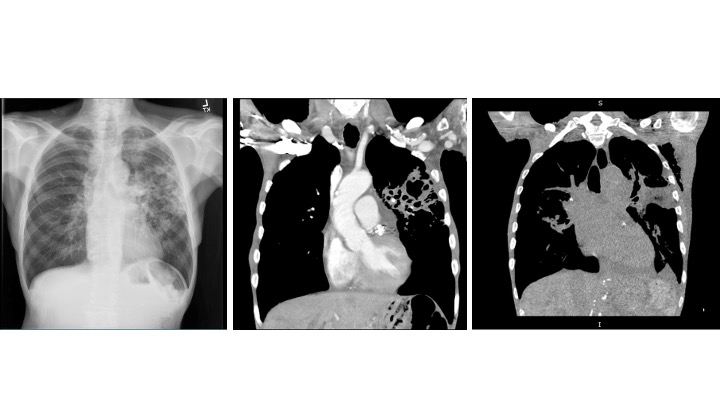
Figure: Endoscopic Pictures: Terminal Ileum Ulcers and Colonic Ulcers
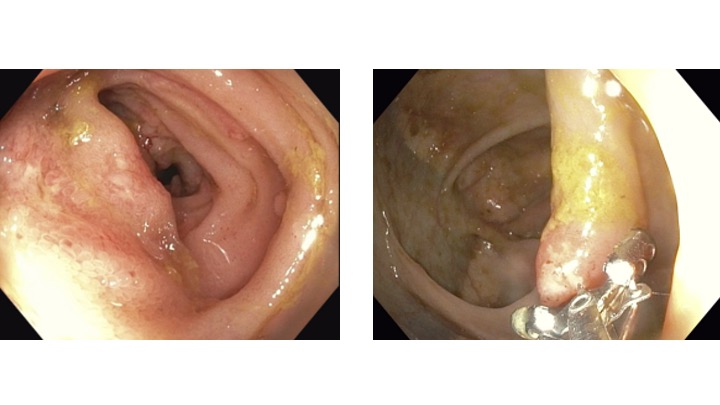
Figure: Chest Imaging
Disclosures:
Ahmad Alkurd indicated no relevant financial relationships.
Michael Meador indicated no relevant financial relationships.
David Okuampa indicated no relevant financial relationships.
Kelly Schulte indicated no relevant financial relationships.
Omar Khan indicated no relevant financial relationships.
Sarav Daid indicated no relevant financial relationships.
Ahmad Alkurd, MD, Michael Meador, MD, David Okuampa, MD, Kelly Schulte, DO, Omar Khan, MD, Sarav Daid, MD. P3496 - The Hidden Culprit: Colonic Tuberculosis Presenting as Refractory Anemia in a Dialysis Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
LSU Health Shreveport, Shreveport, LA
Introduction: Tuberculous colitis is a rare extrapulmonary manifestation of tuberculosis (TB), often mimicking inflammatory bowel disease. We present a unique case of colonic tuberculosis diagnosed in a patient with persistent anemia receiving dialysis and transfusions for end-stage renal disease (ESRD).
Case Description/
Methods: A 77-year-old African American male with ESRD, recently started on dialysis, was referred for evaluation of persistent normocytic anemia, despite receiving multiple iron and blood transfusions. His medical history included prostate cancer (treated with chemoradiation) and squamous cell carcinoma of the tongue (status post left glossectomy). He denied gastrointestinal symptoms or overt bleeding. There was no history of incarceration, travel to endemic regions, or known tuberculosis exposure. A prior colonoscopy five years earlier had been unremarkable. Labs indicated anemia of chronic disease. EGD revealed radiation-induced changes in the esophagus and patchy gastric erythema. Colonoscopy showed multiple aphthous ulcers in the terminal ileum, cecum, and right colon. Biopsies revealed chronic active colitis with non-necrotizing granulomas. Acid-fast bacilli were detected on staining, and Mycobacterium tuberculosis was confirmed by PCR testing of the biopsies. The patient tested negative for HIV and fungal pathogens. RIPE therapy was initiated.
Discussion: Intestinal TB is rare in industrialized countries and is typically associated with HIV or immigration from endemic regions. This patient had no classic risk factors but was relatively immunocompromised due to his ESRD and malignancy history. While anemia can occur in ESRD, persistence despite transfusions warrants further evaluation. Colonic TB most commonly involves the ileocecal region and may appear endoscopically similar to Crohn’s disease, making histological confirmation important. Histology typically shows chronic inflammation with granulomas. Although caseating granulomas are classic, non-caseating granulomas—as seen here—are also consistent. The diagnosis was confirmed by acid-fast bacilli on staining and positive mycobacterial PCR testing in our patient.
Intestinal tuberculosis should be considered in the differential diagnosis of persistent anemia in immunocompromised patients even in the absence of symptoms or classic risk factors. Early diagnosis through endoscopy can guide timely treatment. This case underscores the importance of endoscopic evaluation in unexplained anemia even when more common causes seem apparent.
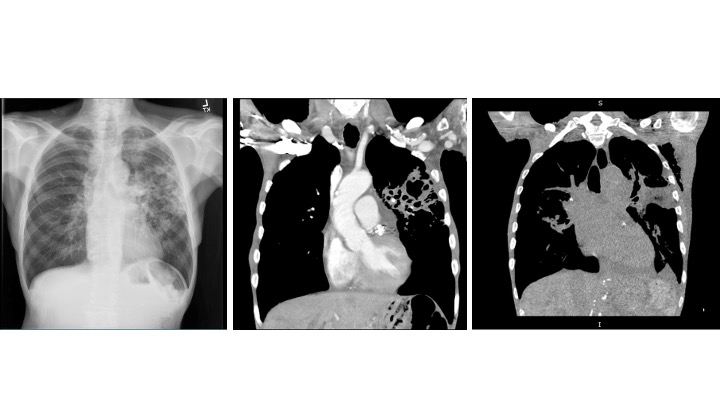
Figure: Endoscopic Pictures: Terminal Ileum Ulcers and Colonic Ulcers
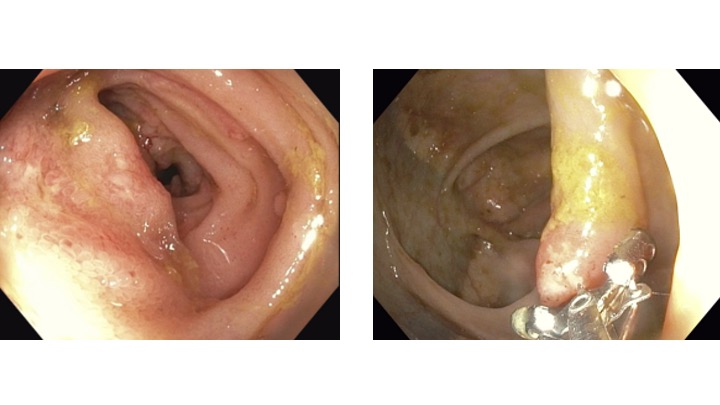
Figure: Chest Imaging
Disclosures:
Ahmad Alkurd indicated no relevant financial relationships.
Michael Meador indicated no relevant financial relationships.
David Okuampa indicated no relevant financial relationships.
Kelly Schulte indicated no relevant financial relationships.
Omar Khan indicated no relevant financial relationships.
Sarav Daid indicated no relevant financial relationships.
Ahmad Alkurd, MD, Michael Meador, MD, David Okuampa, MD, Kelly Schulte, DO, Omar Khan, MD, Sarav Daid, MD. P3496 - The Hidden Culprit: Colonic Tuberculosis Presenting as Refractory Anemia in a Dialysis Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
