Monday Poster Session
Category: Infections and Microbiome
P3471 - Syphilitic Proctitis: An Unusual Initial Presentation of Secondary Syphilis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RA
Rishav Agrawal, MD (he/him/his)
NewYork-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Rishav Agrawal, MD, Carl V. Crawford, MD
NewYork-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: Syphilis is a systemic infection with diverse clinical presentations. Multiple sexually transmitted infections, including gonorrhea, chlamydia, and HSV, can cause infectious proctitis, especially in men who have sex with men (MSM). Syphilis is a less frequent but important etiology for proctitis in this population and its clinical course and endoscopic findings remain poorly characterized.
Case Description/
Methods: A 61-year-old man with a history of GIST status post subtotal gastrectomy presented to clinic with 1 month of abdominal pain and constipation. He underwent CT A/P which demonstrated mild thickening of the rectum with adjacent lymphadenopathy concerning for new rectal malignancy. Colonoscopy revealed a patchy area of moderately inflamed mucosa in the rectum with one dominant ulcerated nodule (Figure 1). Biopsies were consistent with syphilitic proctitis, confirmed via positive T. pallidum immunostain. He endorsed unprotected ano-receptive sex 3-months prior with a partner who had genital ulcers. Within one week, the patient developed fever and a pruritic red maculopapular rash spreading from the abdomen to his torso and arms. He presented to the emergency room and labs showed elevated Creatinine to 2.1 mg/dL (baseline 1.1 mg/dL) and LFTs, with AST 72 U/L, ALT 110 U/L, ALP 737 U/L, and total bilirubin 2.9 mg/dL (2.5 mg/dL direct). He underwent MRCP, which was unremarkable, and his liver injury was felt to be consistent with syphilitic hepatitis. He underwent renal biopsy showing membranous nephropathy, thought to be due to secondary syphilis. He received two doses of IM Penicillin G with plans for a third dose after discharge, and his LFTs normalized with resolution of all symptoms within 10 days. CT A/P four days after discharge showed resolution of rectal thickening and lymphadenopathy.
Discussion: Syphilis is an important diagnostic consideration for proctitis, particularly in the MSM population. It can mimic rectal malignancy with imaging findings such as rectal wall thickening and adjacent lymphadenopathy. Definitive diagnosis relies on a direct visualization of rectal inflammation and/or ulceration via colonoscopy and testing for T. pallidum in tissue biopsies. This case further highlights how proctitis can predate systemic manifestations of the infection such as rash or hepatitis. IM penicillin led to rapid resolution of proctitis, hepatitis, and other systemic sequelae in this patient, emphasizing the importance of early diagnosis and therapy to prevent complications.
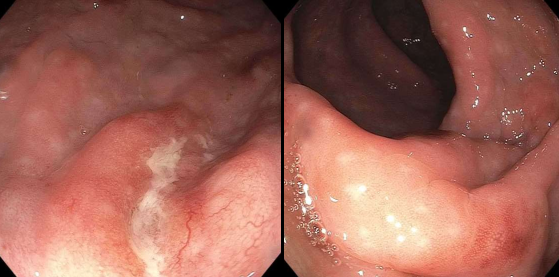
Figure: Figure 1. Colonoscopy images of inflamed rectal tissue with visible erythema, nodularity, and mild ulceration.
Disclosures:
Rishav Agrawal indicated no relevant financial relationships.
Carl Crawford: Ferring – Advisor or Review Panel Member, Consultant, Grant/Research Support, Speakers Bureau. lumen – Grant/Research Support. nestle – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Phathom – Speakers Bureau. vedanta – Grant/Research Support.
Rishav Agrawal, MD, Carl V. Crawford, MD. P3471 - Syphilitic Proctitis: An Unusual Initial Presentation of Secondary Syphilis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
NewYork-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: Syphilis is a systemic infection with diverse clinical presentations. Multiple sexually transmitted infections, including gonorrhea, chlamydia, and HSV, can cause infectious proctitis, especially in men who have sex with men (MSM). Syphilis is a less frequent but important etiology for proctitis in this population and its clinical course and endoscopic findings remain poorly characterized.
Case Description/
Methods: A 61-year-old man with a history of GIST status post subtotal gastrectomy presented to clinic with 1 month of abdominal pain and constipation. He underwent CT A/P which demonstrated mild thickening of the rectum with adjacent lymphadenopathy concerning for new rectal malignancy. Colonoscopy revealed a patchy area of moderately inflamed mucosa in the rectum with one dominant ulcerated nodule (Figure 1). Biopsies were consistent with syphilitic proctitis, confirmed via positive T. pallidum immunostain. He endorsed unprotected ano-receptive sex 3-months prior with a partner who had genital ulcers. Within one week, the patient developed fever and a pruritic red maculopapular rash spreading from the abdomen to his torso and arms. He presented to the emergency room and labs showed elevated Creatinine to 2.1 mg/dL (baseline 1.1 mg/dL) and LFTs, with AST 72 U/L, ALT 110 U/L, ALP 737 U/L, and total bilirubin 2.9 mg/dL (2.5 mg/dL direct). He underwent MRCP, which was unremarkable, and his liver injury was felt to be consistent with syphilitic hepatitis. He underwent renal biopsy showing membranous nephropathy, thought to be due to secondary syphilis. He received two doses of IM Penicillin G with plans for a third dose after discharge, and his LFTs normalized with resolution of all symptoms within 10 days. CT A/P four days after discharge showed resolution of rectal thickening and lymphadenopathy.
Discussion: Syphilis is an important diagnostic consideration for proctitis, particularly in the MSM population. It can mimic rectal malignancy with imaging findings such as rectal wall thickening and adjacent lymphadenopathy. Definitive diagnosis relies on a direct visualization of rectal inflammation and/or ulceration via colonoscopy and testing for T. pallidum in tissue biopsies. This case further highlights how proctitis can predate systemic manifestations of the infection such as rash or hepatitis. IM penicillin led to rapid resolution of proctitis, hepatitis, and other systemic sequelae in this patient, emphasizing the importance of early diagnosis and therapy to prevent complications.
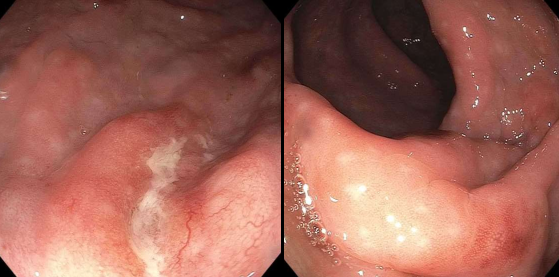
Figure: Figure 1. Colonoscopy images of inflamed rectal tissue with visible erythema, nodularity, and mild ulceration.
Disclosures:
Rishav Agrawal indicated no relevant financial relationships.
Carl Crawford: Ferring – Advisor or Review Panel Member, Consultant, Grant/Research Support, Speakers Bureau. lumen – Grant/Research Support. nestle – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Phathom – Speakers Bureau. vedanta – Grant/Research Support.
Rishav Agrawal, MD, Carl V. Crawford, MD. P3471 - Syphilitic Proctitis: An Unusual Initial Presentation of Secondary Syphilis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
